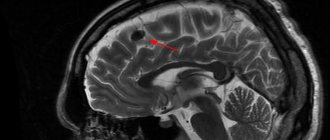
MRI: T1-weighted axial view. Red arrow (1) indicates the right hemisphere of the brain, (2) gray matter, (3) white matter
Brain changes on MRI can be caused by various reasons. Experts are confident that the earlier the disease is identified and treatment is started, the greater the chances of a successful outcome. Magnetic resonance imaging of the head vessels can be performed on most people without any serious side effects or long-term consequences. Modern contrast agents based on gadolinium chelates do not cause complications in 98% of cases. The only serious obstacle to the diagnostic procedure is the presence of metal in the human body, which requires another method of examination, for example, CT.
- What diseases cause lesions in the brain on MRI?
- Prices for MRI of the brain
What brain pathologies does MRI show?
The distribution of white and gray matter and pathological processes within the brain are illustrated in detail by MRI. Magnetic scanning is one of the high-precision non-invasive methods of instrumental diagnostics for neurosurgeons, neurologists, and, less often, psychiatrists. Analysis of changes in the two main components of the brain - gray and white matter - is important for clinical diagnosis and therapy of a huge number of diseases: epilepsy and episyndrome, stroke, Alzheimer's disease, malignant and benign neoplasms, multiple sclerosis, infectious and inflammatory processes, post-traumatic injuries, etc.
Distribution of gray and white matter in the brain
Gray matter
The gray matter of the brain is responsible for most of the functions of higher nervous activity and is represented by neuron bodies, glial cells, a cluster of dendrites, thin tiny blood vessels - capillaries - and unmyelinated axons. The main histological structures are centers, each of which controls some action: the act of urination, defecation, heartbeat, etc. Neurosurgeons consider the gray color to be conventional; rather, this substance has an earthy tint. The composition of the main structures of the brain is clearly distinguishable, mainly due to differences in water and protein content. This allows one zone to be differentiated from another on tomograms. Pathological processes localized in the gray matter lead to disturbances in perception, speech, emotions, memory, sensory sensitivity, will, muscle movements, etc.
White matter
The white color is caused by bundles of nerve fibers covered with a myelin sheath. The main purpose of this brain structure is the transmission of impulses from the main centers to the periphery (lower links of the nervous system).
Characteristics and localization of lesions
Depending on the location, the outbreak can be:
- perivascular (located around small sclerotic arterioles in the thickness of the white or gray matter);
- supratentorial (localized above the cerebellar tentorium);
- subependymal (under the ependyma - the membrane lining the inside of the ventricles of the brain);
- marginal, or marginal (located under the membranes of the brain).
In count:
- single;
- plural.
The focus of gliosis is an area of dead neurons , therefore it does not have the functions of conducting a nerve impulse, accumulating and using information.
The more intact areas there are in the brain and the larger the lesion, the more pronounced the clinical picture of the disease .
- Hemorrhagic cerebral stroke: what it is, symptoms and consequences
What brain diseases can MRI detect?
Changes in white matter on MRI in various pathologies
MRI of the brain is performed to diagnose:
- tumors. MRI is one of the highly informative methods in identifying oncological processes in the brain; it allows one to establish the relationship of the tumor with surrounding tissues;
- metastatic lesions (tumor screenings). For many malignant neoplasms, the brain is the target organ.
- lesions that appeared against the background of various angiopathy, hypertension, atherosclerosis, migraine, hyperhomocysteinemia;
- inflammatory processes, including those of an autoimmune nature: multiple sclerosis, sarcoidosis, etc.;
- infections: HIV, tuberculosis, herpes, neurosyphilis, mycoplasmosis, etc.;
- post-traumatic changes after receiving a direct blow to the head or to identify lesions after radiation therapy, which is also considered by radioradiologists as an altering factor;
- various metabolic disorders, toxic damage;
- heart attacks and strokes, foci of ischemia, dyscirculatory encephalopathy (impaired blood microcirculation is manifested by hypoxic/dystrophic changes in the brain);
- vascular malformations;
- anomalies and developmental defects.
What diseases cause lesions in the brain on MRI?
The principle of constructing an image during MRI of the brain is based on combining many slices, ranging in size from 1 mm, into a single whole, but the doctor can evaluate each layer separately
An example of damage to gray matter with the formation of foci is heterotopia and its most common variant is subependymal, which is associated with epilepsy and developmental delay. In the diagnosis of this pathology, magnetic resonance imaging of the brain is the predominant study. Epileptic seizures may appear in adulthood, which requires exclusion of a tumor. Changes in the gray matter are found in schizophrenia (loss of tissue density in the superior frontal lobule, left superior temporal gyrus), bipolar disorder, etc. Foci in the brain of a patient suffering from mental disorders are often found, but the main criterion for diagnosis is symptoms.
Differentiation of white matter pathologies includes a whole spectrum of diseases, but MRI of the brain also shows areas that do not always indicate disease and are a normal variant in older people. The latter are included in the concept of “benign aging of the brain.” Destructive zones can occur against the background of hypoxia and ischemia. On MRI, changes in the white matter of the brain associated with focal lesions are found in:
An MRI image shows changes in the white matter of the brain: green arrows indicate multiple demyelinated lesions in multiple sclerosis
- Multiple sclerosis. MS is an inflammatory (autoimmune) disease that causes spots in the white matter of the brain. The pathogenesis is not known for certain. Similar areas are found in herpesvirus infection, leukoencephalopathy, intoxication, therefore, before making a diagnosis, tomogram data is always assessed after analyzing the clinical situation and testing the cerebrospinal fluid. An MRI of the spinal cord is often required.
MRI: acute disseminated encephalomyelitis
- Acute disseminated encephalomyelitis. Multifocal lesions appear on tomograms 1.5-2 weeks after contact with the pathogen or vaccination. Other structures of the nervous system may also be involved in the process. Better visualization of lesions is provided by contrast. The size of the demyelinated areas is larger than in multiple sclerosis, and the disease is more often diagnosed at a young age.
MRI: Neuroborreliosis (tick-borne encephalitis)
- Lyme disease. Magnetic resonance scanning shows pinpoint lesions, a similar picture can be observed in autoimmune diseases. But for this nosology, a specific rash on the skin and a malaise resembling a cold and arthralgia are also typical. Tomograms show a hyperintense signal from the spinal cord and accumulation of paramagnetic in the region of the root zone of the VII pair of cranial nerves.
Sarcoidosis on MRI: yellow arrows indicate lesions of the membranes, cranial nerves, similar changes are present in the trunk
- Sarcoidosis of the brain. The diagnosis is difficult to establish only with magnetic scanning; sometimes final verification occurs after a biopsy. The picture on the tomograms resembles the changes characteristic of multiple sclerosis.
Negative dynamics on tomograms performed at monthly intervals for leukoencephalopathy
- Progressive multifocal leukoencephalopathy. The pathogenetic factor is infection with the Cunningham virus, which affects people with immunosuppression (severe dysfunction of the immune system). There is damage to the arcuate fibers of the white matter, with contrast there is no accumulation effect. Pathological foci are often localized on one side, sometimes symmetrical changes are visible.
Life prognosis for patients with gliosis
To talk about life prognosis, you need to remember what causes gliosis. Usually the disease is provoked by severe diseases of the cardiovascular and nervous systems. Therefore, mortality statistics from gliosis are imperfect: some patients die from primary diseases. But the average number of years that an adult with a similar diagnosis can live is two or three years.
With timely and high-quality treatment, this period can increase by almost one and a half times.
You can increase this period if you consult a doctor in time.
The fact is that only a doctor can determine how life-threatening glial tumors are. And only in a specialized clinic will it be possible to conduct a correct diagnosis and develop further therapy.
People living with gliosis experience paralysis, hearing and vision problems, and memory and attention disorders.
Unfortunately, even with proper treatment, the patient’s life is complicated by the side effects of the disease. For example, if a person develops supratentorial gliosis, it will be followed by hallucinations, the shapes and scales of objects will be distorted, and cognitive connections between the image of an object and its name will be disrupted. There is no guarantee that treatment will stop the development of gliosis completely, but this does not eliminate its need.
Dystrophic changes in the brain on MRI
Cerebral angiography
When the blood supply is disrupted, oxygen and trophic starvation of cells (ischemia) develops. This leads to degenerative processes and is accompanied by dysfunction. The severity of the latter is variable, depending on whether blood is completely blocked or a partial influx remains. Dystrophic changes can be local or diffuse. Total brain damage is recorded in meningitis, encephalitis, focal changes are typical for cysts, small ischemic processes, and the formation of post-traumatic scars.
Clinical manifestations may include:
- headache;
- high blood pressure;
- the appearance of paresthesia (a feeling of numbness or tingling in the limbs), loss of sensitivity;
- deterioration of vision (up to blindness, which indicates damage to the optic nerve), memory, decreased intellectual abilities;
- insomnia;
- hyperkinesis (uncontrolled muscle contractions) and convulsions.
As the pathology progresses, paresis and paralysis are expected, so it is important to do an MRI of the brain vessels at the first symptoms of trouble. Single lesions can be detected in young men and women and do not always indicate pathology. The doctor’s tactics are dynamic observation and repeated magnetic scanning after 3-6 months, which will allow not to miss the development of any serious disease, for example, multiple sclerosis. Over the age of 60-65 years, lesions are found in almost all patients, which is explained by natural aging. These changes are irreversible, but the progression of the process can be slowed down with adequate treatment.
Provoking factors include:
- chronic alcohol and nicotine intoxication;
- stressful situations;
- irrational work and rest regime;
- obesity;
- low physical activity;
- persistent increase in blood pressure;
- diabetes;
- hypercholesterolemia.
The type of dystrophic disorders in the gray and white matter of the brain on MRI will depend on the nature of the pathological process.
Diagnostics
Focal changes in the brain are difficult to diagnose in the initial stage. Detection of pathology is made difficult by the rather sparse symptoms.
Ultrasound diagnostics with Doppler sonography reveals abnormalities in the vessels of the brain (asymmetry, increased venous blood flow, stenosis, atherosclerosis). CT scan (computed tomography) determines previous heart attacks, accumulation of fluid in cavities and thinning of tissues (atrophy of brain structures).
The most reliable and accurate results can only be obtained by examining magnetic resonance imaging (MRI) of the skull. The image is obtained by interacting an electromagnetic field with hydrogen atoms.
This diagnosis allows you to evaluate the functioning of neurons and detect changes in the density of brain tissue. Having identified asymptomatic stages of focal lesions, it is possible to begin timely therapy.
MRI allows you to obtain images in three planes (transverse, longitudinal and frontal) and identify the cause of malnutrition of brain structures:
- Necrotic single lesion in the cerebral cortex, resulting from narrowing or closure of a spinal artery by a thrombus (congenital pathologies, the result of atherosclerosis or spinal hernia);
- Multiple focal lesions – pre-stroke condition (diagnosis allows timely treatment to begin and the development of irreversible processes to be prevented);
- Changes in the frontal or parietal lobe - small lesions that occur with hypertension and crises;
- Microfocal lesions - diagnosed by injection of a contrast agent, typical for older patients, or the presence of congenital anomalies.
The detected pathology using MRI allows one to assess the rate of disease progression and choose the right treatment tactics.
Vascular changes in the brain on MRI
MRI: ischemic zone during stroke (highlighted with a red oval)
If cerebrovascular pathology is suspected, special attention is paid to the condition of the arteries during MRI of the brain. The study always involves the introduction of contrast, and it is called magnetic resonance angiography. In urgent situations in case of vascular accidents, CT is performed, since X-ray diagnostics takes less time and clearly demonstrates the area of damage during hemorrhages, but after stabilization of health, magnetic resonance angiography is quite justified. The study shows atherosclerotic plaques, blood clots and aneurysms (protrusions), their localization, and wall deformation.
With an ischemic stroke, darkened and blurred areas of irregular shape are visible almost immediately on magnetic tomograms, appearing on a computer scan only at the end of the first day. The lesion is often unilateral. The outpouring of blood from a ruptured vessel gives an intense light color, but only in the first hour and a half from the moment of the disaster, and then becomes invisible on MRI, although it is clearly visualized using CT. As a consequence of a stroke, a fluid-filled pseudocyst is formed, and deformation of the nerve tissue appears. MRA is indispensable in the diagnosis of tumor angiogenesis. Increased vascularization of a pathological focus is always suspicious of a malignant neoplasm, which grows and feeds due to increased blood flow. If the vessels do not keep up with the growth of the tumor, areas of ischemia and necrosis appear.
Treatment
Therapy involves solving three problems. Eliminating the root cause, relieving symptoms, preventing complications.
There are two methods: conservative or surgical. In the vast majority of cases, the use of medications and, if necessary, lifestyle adjustments are sufficient. What medications are prescribed?
For hypertension and symptomatic increase in blood pressure:
- Means for lowering blood pressure. Beta blockers (Propranolol, Anaprilin, Metoprolol), ACE inhibitors (perindopril in different variations), calcium antagonists (Diltiazem or Verapamil), diuretics (Veroshpron, Hypothiazide), also diuretics, also centrally acting medications (Moxonidine).
- Statins. To adjust the concentration of cholesterol and other lipids in the bloodstream.
In addition, patients are advised to correct their diet (minimum fat and up to 7 grams of salt per day), adequate drinking regimen (1.3-1.8 liters or more, as needed, taking into account the recommendations of a specialist).
Diabetes:
- Antihyperglycemic agents, insulin as needed.
- Statins.
It is also possible to use medications to lower blood pressure levels.
Lenticulostriate type:
The deposition of calcium salts does not always require correction. There is no specialized treatment. Symptomatic drugs are used.
As for the amyloid form:
- A nicotinic acid. The main means of combating violations.
- Immunosuppressants, glucocorticoids (Prednisolone and analogues), cytostatics as needed. But this occurs extremely rarely. The purpose of these drugs is to reduce the activity of the body's defenses.
Systematic administration of vitamin-mineral complexes is indicated for all categories of patients.
Physiotherapy and acupuncture have proven themselves well.
Surgical correction is rarely needed. If there are clear foci of microangiopathy and there is a critical disturbance in the nutrition of nerve tissue in this particular area of the brain. With an additional condition: the drugs do not help.
Attention:
None of these methods can completely eliminate the disorder in the later stages. Foci of gliosis and scars do not disappear anywhere.
However, there is every chance of bringing the disorder under control. Moreover, the body, through the development of collaterals, can cope quite well on its own. You just need to support him.
Normal magnetic resonance imaging of the brain
MRI of the brain, normal
The normal MRI of the brain is a relative concept, depending on the age, gender of the patient, changes in tomograms are necessarily compared with symptoms. The doctor evaluates the symmetry of the lobes, the size of the ventricles, blood vessels, the uniformity of their filling with a contrast agent, the absence of neoplasms, malformations, and much more. A computer program builds layer-by-layer images, after examination they are printed onto films and examined by placing them on a X-ray viewer. Next, fill out a conclusion form indicating the preliminary diagnosis. It is hardly possible to decipher an MRI of the brain on your own without special training: an inexperienced person, even if he sees a lesion, will not figure out what caused its appearance. All questions can be asked to the doctor who conducted the study. In unclear situations with ambiguous results, obtaining a second opinion is justified. Often patients, having read the words “neoplasm, tumor, NEO” in the conclusion, try to immediately find out the prospects of the disease from the radiologist, which fails. These questions can be answered by a neurosurgeon after receiving the biopsy results. Sometimes, to complete the picture, it is necessary to additionally do an MRI of the cervical spine.
Possible complications
{banner_banstat9}
Consequences are relatively rare. Years pass from the development of microangiopathy to the final outcome. However, you cannot relax.
Possible problems include:
- Stroke. Acute cerebrovascular accident. Provokes the death of nerve tissue. Severe disability with neurological deficit. The death of a person is possible and even probable.
- Encephalopathy. The process is similar, but there is no destruction of cerebral structures yet.
- Vascular dementia. Dementia due to insufficient brain nutrition.
Complications develop spontaneously. Treatment is the only way to prevent them.
Types of lesions
There are several types of focal GM diseases. The most dangerous are neoplasms. In the early stages, brain tumor symptoms can be confused with migraines and other illnesses. But with growth, the functioning of neurons deteriorates and signal transmission to the brain is disrupted. If the tumor grows, it begins to invade more and more new territories, and the clinical picture begins to increase.
Another type of focal disease is a cyst (a small cavity with liquid contents). For a long time, cavities do not make themselves felt until they begin to grow and increase in size. Despite the fact that they are not prone to growth and increase in size, like neoplasms, they are also considered a foreign body. Cysts can cause compression of blood vessels, which complicates the flow of blood to the brain.