Often, a diagnosis such as “Mild diffuse changes in the bioelectrical activity of the brain” can be heard from a doctor after undergoing an electroencephalogram - a non-invasive method of assessing and recording the electrical activity of the cerebral cortex using a special device called an electroencephalograph. As a result of its implementation, all electrical phenomena in the cerebral cortex, including its activity, are recorded on paper in the form of a curve, which allows a specialist to evaluate the functioning of the organ in full.
Subsequently, the patient and his relatives may have quite natural questions: what is this and why are diffuse changes in the bioelectrical activity of the brain dangerous for health? Despite the fact that this diagnosis sounds scary, not everything is so bad: timely therapy can return the patient to the usual rhythm of life.
Diffuse brain lesions and their occurrence
As is known, the functional unit of the central nervous system (neurons) is especially sensitive to an insufficient amount of oxygen supplied to them. Clinically, this is expressed in the destruction of interneuronal connections, decreased activity and metabolic disorders, both in the cells themselves and in the sections to which they belong. These processes can lead to the death of part of the brain matter and a decrease in its performance.
Therefore, the root cause of diffuse damage and, accordingly, changes in bioelectrical activity is the poor provision of its components with microelements against the background of the influence of various negative factors.
Organic diffuse damage can occur due to pathologies that are accompanied by swelling, inflammation and the appearance of scar tissue in the medulla. For example, these could be the following diseases: encephalitis, meningitis, atherosclerosis and toxic poisoning by various chemicals.
Patients who have been infected with a neuroinfection or have been under the influence of toxic substances for a long time can be justifiably referred by the attending physician to study the biological activity of the brain using an electroencephalograph. It is a medical electrical measuring device that, using special sensors, measures and records the potential difference between points of the brain located deep in the brain or on its surface.
Subsequently, the obtained data is recorded in the form of an electroencephalogram - a curve or graphic image of an oscillatory electrical process. During data decoding, the following types of rhythms are assessed, which characterize the state of brain activity at the moment:
- Alpha - the highest rates are recorded in a person’s resting state; normally, the polymorphic activity of this type of waves should be within the range of 25 - 95 μV;
- Betta - these waves appear in the presence of vigorous activity;
- Gamma rhythm is determined when solving intellectual problems and situations that require increased attention and concentration;
- Kappa - determined in the temporal lobe during mental processes;
- Lambda - is formed in the occipital zone, when processing visual information;
- Mu - starts in the occipital part and is observed in a calm state of the subject;
- To complete the picture, delta, theta and sigma rhythms are assessed, which are indicators of sleep, or are included in the presence of pathology.
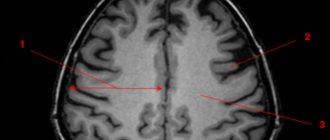
Depending on the degree of destruction of brain structures and the location of the affected area, the amplitude of oscillation of the electroencephalograph sensor will differ from accepted norms and is expressed graphically as follows:
- the presence of uncharacteristic hyperrhythmic activity in the absence of dominant regular bioelectrical activity;
- a deviation in the values of the electroencephalogram can manifest itself in the asymmetry of the graphic image of brain activity, while symmetrical areas will give different values and frequencies of amplitude oscillations;
- the main indicators by which the degree of diffuse damage is determined will exceed normal values (delta -, alpha -, theta - values).
If these deviations are present on the diagram, then the specialist, after decoding, will write in the preliminary conclusion the following diagnosis: “diffuse damage to brain structures,” the degree of severity of which will depend on the quantitative value of the deviations.
Often, mild and moderately pronounced diffuse changes in the bioelectrical activity of the brain are diagnosed only after undergoing an electroencephalogram, since their manifestations have a lesser impact on the life of the patient and often go unnoticed both for himself and for others.
But after the final diagnosis is made, everything falls into place - the specialist can clearly explain the reason for the occurrence of some deviations: the appearance of headaches of unknown origin, sudden changes in mood, excessive irritability, deterioration in general well-being and loss of interest in previous hobbies.
The dynamics of restoration of brain activity depend on how soon treatment is started, but this process is long and usually takes a long time - from several months to several years after the first signs of the disorder appear.
Diffuse axonal injury (DAD) of the brain is most often a consequence of traumatic brain injuries and concussions, which could cause rupture of small vessels and capillaries. Since the neurons of the thalamus and hypothalamus are sensitive even to short-term lack of nutrients, and their axons to mechanical damage, the EEG will be characterized by transient and persistent disturbances in the functioning of subcortical structures and the brain stem.
The severity of the damage depends on the strength of the manifestation of secondary signs of injury - the extent of edema, disorganization of intercellular metabolism and the complications that they caused.
Pronounced diffuse changes in the bioelectrical activity of the brain are usually diagnosed in the absence of long-term treatment of the underlying cause of the underlying disease, such as atherosclerosis, since in this disease the organ structures do not receive sufficient oxygen and other nutrients due to the narrowing of the lumen of blood vessels. In this case, the electroencephalogram shows a significant decrease in the threshold of convulsive readiness, which indicates the patient’s predisposition to the development of epilepsy.
A severe degree of diffuse disorders develops against the background of necrotic processes and the formation of scar tissue. At the same time, a disturbance in the conductivity of the electroencephalograph signal is clearly visible in the affected area, which indicates an advanced stage of the disease. The cause of the pathology may be diffuse astrocytoma and other brain tumors.
Despite the detailed identification of the location of diffuse tissue destruction, electroencephalography cannot accurately indicate the cause of abnormalities in the appearance of disturbances in brain activity, so the patient requires a comprehensive examination, including MRI and CT.
Again, some deviations in brain epiactivity may be present on the electroencephalogram even in a child, which is explained by imperfect development of the nervous system. Moreover, if the manifestations are not significant and do not affect the life support systems, then in this case radical treatment is not prescribed, and the patient is placed under the supervision of a neurologist who can compensate for the difference in indicators with medications.
Coma patterns and triphasic waves
Unusual generalized BEAGM changes observed in comatose patients include alpha coma, beta coma, and spindle coma.
Three-phase waves are positive, high-amplitude sharp fluctuations of more than 70 microvolts. A positive wave is usually preceded by a slow negative wave. Typically, the first negative wave has a higher amplitude than the second. The standard clinical correlate of triphasic waves is metabolic or other type of encephalopathy.
Alpha, beta and spindle coma are less common in clinical practice, but the most dangerous. All patterns of coma usually indicate a severe degree of encephalopathy. It should be noted that the patient's psychomotor reaction is a good prognostic factor in these conditions.
Triphasic waves are classically associated with hepatic encephalopathy. However, they are not specific and can be observed in uremic encephalopathy, as well as in other types of metabolic disorders. Many other diseases may have a triphasic morphology. Like regulatory changes in BEAGM, triphasic waves are quite often observed in the context of a pseudoepileptic seizure.
SOURCE: https://vekzdorov.info/o-chem-svidetelstvuet-nalichie-diffuznyh-izmenenij-golovnogo-mozga.html https://diagnostinfo.ru/drugie/efi/diffuznye-izmeneniya-na-eeg.html https: //golovnie-boli.com/bolezni-golovnogo-mozga/legkie-diffuznye-izmeneniya-bioelektricheskoj-aktivnosti-golovnogo.html
Causes of diffuse changes
Disorganization of the bioelectrical activity of the brain cannot occur just like that. Usually it is preceded by various deviations in the organization of the brain matter, for example, injuries or diseases, due to which processes are disrupted and interneuronal connections are destroyed.
The bioelectrical activity of the brain can be disorganized for several reasons:
- Head injuries. The degree of deviation is determined by the severity of the injury. Thus, with a concussion, mild and moderately pronounced diffuse changes in the BEA of the brain are most often diagnosed, and severe traumatic brain injuries subsequently lead to the formation of zones with volumetric lesions of impulse conduction.
- Inflammatory diseases of a neuroinfectious nature. Most often, the spinal cord and subarachnoid space are affected, which disrupts the metabolism between its structures and stops the normal circulation of cerebrospinal fluid in the ventricles. This process can lead to swelling of the white matter and the formation of scar tissue in areas of mechanical damage, which manifests itself in the irritative nature of diffuse disorders. That is, the electroencephalogram will have a large number of beta oscillations of high frequency and amplitude.
- Atherosclerosis of blood vessels and other diseases accompanied by impaired patency of blood vessels. When examining a patient at the initial stage of these diseases, an electroencephalogram usually indicates the presence of mild to moderately pronounced diffuse changes in the bioelectrical activity of the brain. However, if the situation worsens, signs of their progression will manifest themselves in a deterioration in the conductivity of interneuronal connections and, as a consequence, in distortion of the graphic image.
- Exposure to radiation or chemical poisoning. Exposure to radiation affects the entire body, but especially activity, that is, brain function. The consequences of both radiological and toxic poisoning are irreversible, which affects the patient’s ability to carry out everyday activities. Diffuse tissue destruction caused by these reasons requires serious restorative therapy. Diffuse changes in the structure of the brain can be triggered by disturbances in the functioning of the hypothalamus and pituitary gland.
During the diagnostic process and based on the results of a conversation with the patient, the specialist must find out as accurately as possible why diffuse tissue destruction occurred - after all, the patient’s life often depends on how quickly the final diagnosis is made and the cause of the disease is eliminated:
- mild structural disorganization in the structure of the brain appears after suffering minor head injuries, concussion;
- moderate severity of the pathology is a consequence of an inflammatory or infectious disease;
- Severe diffuse changes in the biological activity of the brain are diagnosed in patients exposed to long-term radiation training or chemical poisoning, and the consequences of such exposure are mostly irreversible or difficult to treat.
In children, a delay in the bioelectrical maturity of the brain is expressed in the appearance of deviations in the reproduction of certain neurophysiological processes, for example, this may be a violation of motor skills, emotional disorders or developmental delays. The emphasis of certain disturbances will depend on the location of the zone of diffuse changes.
In this case, early maturation of brain activity may be the reason for the formation of areas of increased epiactivity. If left untreated, this pathology can lead to the appearance of convulsions and epileptic seizures.
Periodic diffuse epileptiform discharges
Electrical discharges in this type of generalized changes in BEAGM occur at regular intervals. The discharges are multiphase and have an epileptiform morphology. Thus, they are similar to periodic lateral epileptiform discharges (PLEDs), except that they have a generalized rather than lateral distribution.
They are sometimes called generalized periodic epileptiform discharges (GPED). In contrast, the term bi-PLED generally refers to periodic discharges that are asynchronous.
Burst-suppression pattern or mild periodic EEG changes
Moderate regulatory changes in the EEG are characterized by a burst of activity (a mixture of sharp and slow waves), periodically alternating with episodes of inhibition (activity <10 μV). As a rule, episodes of inhibition are longer (usually 5-10 s) than bursts of activity (1-3 s). In some patients (for example, a child), the change in excitation and inhibition of the cerebral cortex can occur very quickly. Appearance of pathological EEG, “burst-suppression” pattern
Electrobrain inactivity
Electrobrain inactivity (EMI) is characterized by activity less than 2 μV; To make a diagnosis of brain death, the electroencephalogram must be recorded according to strict rules. These requirements determine recording time, interelectrode distance, test reactivity, and recording continuity.
Severe encephalopathic electroencephalogram patterns are nonspecific with respect to etiology, but represent extremely dangerous degrees of encephalopathy. Because sedatives may cause or worsen these abnormalities, interpretation of the findings should only be performed by a neurologist. The above types of generalized disorders indicate very severe brain dysfunction if sedatives are excluded as a cause.
Intermittent discharges, including burst-suppression patterns, are somewhat more common in anoxic injuries than in other systemic disorders. Intermittent epileptiform discharges may be caused by high doses of sedatives such as barbiturates, benzodiazepines, or propofol.
In the appropriate clinical context, certain periodic patterns may aid in the diagnosis of Creutzfeldt-Jakob disease (CJD) and subacute sclerosing panencephalitis (SSP). Classically, the periodicity for CJD is approximately 1-2 seconds, while for PSP it is about 4-10 seconds.
Rhythmicity or periodicity is one of the hallmarks of electrographic seizures; Thus, paroxysmal discharges are quite often observed in the structure of pseudoepileptic seizures.
Attention! EMR may be the basis for a diagnosis of clinical death. However, contrary to popular belief, an EEG is not required for a neurologist to conclude brain death and is only used as an auxiliary test.
Diffuse changes after injury
Often the consequence of mechanical damage or severe contusion of the head is the rupture of long functional processes of nerve cells - axons. In this case, the patient is diagnosed with diffuse brain injury, and the severity of the damage is determined by the number of disorders the development of which it provoked.
A characteristic feature of such an injury is the unconscious state of the victim, and the longer the comatose state lasts, the worse the prognosis - in most cases the patient remains either deeply disabled or his death is recorded.
This is explained by the fact that moving parts of the brain can shift, and fixed parts can twist, while even a slight shift of cerebral zones threatens a person with complete or partial rupture of axons. The same destructive process can occur with small vessels feeding the anterior section and cortex. As a result, diffuse, that is, uniform death of structural units occurs, which significantly complicates the procedure for diagnosing pathology.
Causes and morphology of DAP
The most common causes of TBI in DAP:
- severe bruise on windshields in an accident;
- a fall;
- hit with a heavy object;
- concussion syndrome in children, in which the brain is severely bruised after a sharp shaking, as well as a beating or fall.
DAP syndrome is the result of contusions caused by angular acceleration of the head. In this case, there may not be a direct collision with the object of injury.
As a result, some patients do not have skull fractures or other visible wounds, which makes diagnosis somewhat difficult. Statistics show that it is oblique damage that leads to axonal damage and the occurrence of DAP.
Morphologically, this injury is characterized by the following three foci of damage:
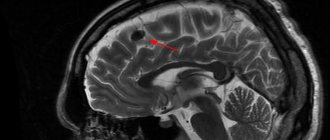
- brain;
- corpus callosum;
- brainstem and diffusely distributed ruptures.
The first two focal signs are macroscopic, which are located in the form of a hematoma up to five mm, looking like torn tissue with bloody edges. A few days after TBI, the lesion becomes pigmented and then scars. A wound in the corpus callosum may resolve with the formation of a vascular cyst.
Axonal disorders in trauma
Consequences and changes in the body
Mild diffuse damage to brain structures usually does not pose a threat to the patient’s life, and its symptoms disappear within a few months after exposure to negative factors. A slight deviation in the development of bioelectrical maturity may be present in children, but this is not critical - in the absence of a catalyst for diffuse disorders and the use of timely restorative therapy, such deviations disappear by adolescence.
Moderately pronounced diffuse changes in BEA are manifested in disruption of the functioning of individual brain structures. For example, graphically, the electrical activity of the cerebral cortex may differ slightly from accepted norms, which in practice manifests itself in signs of moderate disorganization of the work of the anterior sections: impaired memory, vision, hearing, and excessive irritability.
Moderate diffuse changes in the bioelectrical activity of the brain can cause such consequences as:
- decreased performance;
- the emergence of problems at the psychological level;
- absent-mindedness;
- physical slowness.
If the disturbances and symptoms are severe, such as after diffuse axonal injury (DAD), then the severity of the consequences depends on the number of days during which the patient was unconscious.
For example, if the coma lasted less than a day and the skull injury was insignificant, then recovery from the coma begins with the return of eye movements (for example, blinking), then a gradual restoration of consciousness occurs, verbal contact expands, and negative neurological disorders fade away, but do not completely disappear even after a long period of time. treatment.
Pronounced diffuse changes in the bioelectrical activity of the brain are usually recorded in a patient after severe head injuries. Clinically, this manifests itself in the formation of multiple foci of destruction of axonal connections and the opening of bleeding, due to which the organized work of the functional centers of the brain is disrupted. In this case, on the electroencephalogram, significant damage to the thalamus stops the appearance of synchronous EEG waves on the side of the damage.
The body’s protective reaction to such changes in the brain substance is coma, that is, a dangerous state between life and death, which is characterized by loss of consciousness, impaired response to external stimuli, weakened reflexes, erratic rhythm of breathing and heartbeat, changes in vascular tone, and impaired thermoregulation of the body.
A long-term comatose state can be the cause of the patient’s death, since during it the functioning of the regulatory formation structures responsible for the functioning of the body’s life support organs fades away. It is impossible to bring such a person to his senses and return him to a normal life.
Even under favorable circumstances, severe and moderate diffuse changes can provoke swelling of the brain, death of its individual parts, metabolic disorders, inflammation and other pathological general cerebral changes. Even if the patient survives, this is not in vain for him: in the future, his health worsens, brain activity and motor skills are impaired, and mental disorders develop. Children experience regression and noticeable developmental delays.
In addition, in children, even a slight disturbance of brain activity can lead to hyperactivity, increased excitability or, conversely, inhibition, regression of acquired skills, and delayed mental and speech development. All these deviations can be expressed to one degree or another, but such a child is in dire need of treatment, since its absence will only worsen the situation.
Features of the clinical picture
Coma with diffuse brain damage lasts up to three weeks and is manifested by the following symptoms:
- the pupil reflex is impaired;
- gaze paralysis occurs;
- breathing rhythm changes;
- muscle tone increases;
- paresis of the legs and arms appears;
- hypertension is diagnosed;
- febrile or subfebrile temperature and other autonomic disorders appear.
When a patient with DAP wakes from a coma, he or she is in a vegetative state with the following symptoms:
- eyes open to stimuli or on their own;
- the gaze is not concentrated and does not follow moving objects.
A vegetative state, accompanied by impaired reflexes and symptoms of disconnection of the functions of the cerebral hemispheres, can last, on average, from several days to several years. The longer you stay in it, the sooner signs of polyneuropathy appear, such as:
- weakening of the hands;
- chaotic muscle movement;
- neurotrophic disorders;
- increased heart rate;
- swelling;
- tachypnea, etc.
After emerging from a vegetative state, the personality disappears. The main signs of violations after exit:
- extrapyramidal disorders;
- mental disorders manifested by a lack of interest in the reality surrounding the patient, aggression, amnesia, dementia.
Treatment and prevention
The success of treating diffuse changes in the bioelectrical activity of the brain depends on the speed of diagnosis and the degree of pathology that caused them. At the same time, the patient must be clearly aware of the seriousness of the situation - delaying or refusing treatment can provoke the development of a number of other complications.
In especially severe cases, in the presence of concomitant diseases, the help of a neurosurgeon may be required, but if the situation allows, then preference is given to drug therapy.
The speed of restoration of interneuronal connections and, accordingly, normalization of the difference in biopotentials depends on a large number of factors, including the degree of damage to the brain matter - the less it is, the more successful the result of therapy will be, while the patient’s usual rhythm of life will be possible several months after the start of treatment.
The treatment plan is drawn up by the attending physician, usually a neurologist or other specialist who is responsible for treating the cause of the diffuse changes. The rate of normalization of bioelectrical activity depends on the success of the therapy and the cause of such changes - for example, it is easier to eliminate the cause of atherosclerotic vascular damage than to solve problems caused by radiation exposure or toxic effects.
To restore brain activity, the first step is to prescribe medications that eliminate the root cause of circulatory disorders, as well as substances that normalize and relieve neurological and psychopathological syndromes. To cleanse the body after poisoning, antitoxic drugs are prescribed, aimed at neutralizing the poison and removing its breakdown products.
To normalize intracellular metabolism, vitamin complexes are used that contain microelements that improve the functioning of the central nervous system structures, for example, omega-3 fatty acids and B vitamins.
Various physiotherapeutic treatment methods will help improve well-being: for example, magnetic therapy or electrophoresis. Ozone therapy also brings good results, the essence of which is to administer ozonated saline solution intravenously to the patient.
Since the main cause of mild irritative changes in the bioelectrical activity of the brain is impaired blood supply due to narrowing of the lumen of blood vessels, a preventive measure will be correction of the patient’s lifestyle - it is strongly recommended to adhere to a healthy lifestyle and limit the consumption of foods containing animal and vegetable fats. You should also give up bad habits and increase the number of walks in the fresh air.
As a preventative measure, some specialists may prescribe the use of various herbal remedies with a pronounced nootropic effect, which will help enhance brain activity and restore the cognitive functions of the cortex.
Of course, the use of such drugs cannot replace full-fledged drug treatment, however, combined use with basic drugs can significantly help in the treatment of diffuse changes in the bioelectrical activity of the brain; the main thing is to coordinate this with your doctor.
Recovery
Rehabilitation and recovery depends on the disease that led to the disorder of bioelectrical activity. So, with a hemorrhagic stroke, the patient will have to undergo 2-3 months of rehabilitation for lost neurological functions. After treatment of the underlying disease, the electrical activity of the cerebral hemispheres is restored on its own. However, to speed up brain matter regeneration, you should include all B vitamins in your diet, and add walks in the park and morning exercises to your daily routine.