Magnetic resonance imaging is an informative non-invasive way to study cerebral structures. Diagnosis of pathological processes in the brain using other methods is complicated by the presence of the skull, which performs a protective function. Scanning using an induction field allows you to identify the slightest changes. Foci of gliosis are most accurately detected on MRI of the brain; a specialist can determine the nature and localization of the process.
Various forms of gliosis on MRI images of the brain
The study is carried out using a tomograph consisting of a mobile table and a wide tunnel. The device generates a magnetic field, under the influence of which the hydrogen atoms in water molecules are aligned in a special way. Sensitive sensors read the response of scanned tissues, obtaining information about the degree of fluid saturation of brain cells.
A computer program converts the signal into a series of layer-by-layer images taken in axial, sagittal and frontal projections. Based on the images obtained, the doctor can, if necessary, reconstruct a 3D model of the brain.
Signs of gliosis
The human brain consists of an ependymal membrane, glial cells and neurons. The latter transmit nerve impulses throughout the body. Pathological processes affecting the central nervous system (CNS) in some cases lead to the death of neurons.
Glial cells in a normal state perform protective, trophic and secretory functions and are responsible for cellular metabolism. They make up 40% of the total mass of the brain matter. The destruction of neurons stimulates the process of filling the resulting voids with glia, which provide nutrition to the cells of the nervous tissue. In this case, the quantitative ratio of cerebral elements changes.
The process of replacing neurons with neuroglial cells is called gliosis and is considered a secondary disease of the central nervous system. The causes of the pathological phenomenon can be age-related changes, trauma, demyelination and ischemia of cerebral structures.
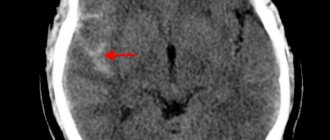
Microangiopathy of the brain, focal changes on MRI (axial projection)
In the early stages, gliosis has no clinical manifestations; the deviation can be diagnosed with a magnetic resonance scan of the brain. As the process progresses, characteristic symptoms arise:
- headache;
- paresis, paralysis;
- speech disorder;
- hearing loss;
- loss of visual acuity;
- lack of coordination in space;
- memory loss;
- decreased concentration;
- development of hypertension.
In newborns, loss of the swallowing reflex, hearing and vision impairment, and symptoms of hydrocephalus are noted.
The clinical picture depends on the type of gliosis, the localization of the process and the nature of the disease that caused the death of nerve cells. Supratentorial focal changes (located above the cerebellum) lead to impaired motor activity and fine motor skills.
Prevention
No drugs or methods of specific prevention of neuronal death have been developed. To maintain the activity of neuro-processes and brain vessels, we can only recommend:
- Lead a healthy lifestyle.
- Monitor your body weight.
- Maintain age-appropriate physical activity.
- Constantly monitor blood pressure, cholesterol , and blood sugar levels.
- Minimize bad habits.
- Practice a healthy balanced diet by minimizing foods containing animal fats.
- Train brain functions: solve puzzles/crosswords, learn poetry, foreign languages.
Foci of gliosis
Tissue proliferation occurs due to the death of neurons. This process can be diffuse or focal, depending on the etiology of the disease. The first type is characterized by the absence of limited pathologically changed areas. The cause is diffuse lesions of the central nervous system (brain and spinal cord).
Focal gliosis is characterized by single or multiple islands with a clear boundary. The location and size of pathological areas depends on the reasons that caused the death of neurons.
Single outbreaks
A limited area of growth of glial cells may be a consequence of age-related changes, chronic hypertension, or a localized inflammatory process. In children, the cause of the pathology is birth trauma, most often the altered area is located in the left or right parietal lobe.
Single lesions do not have clinical manifestations; the disease can be diagnosed by angiography of cerebral vessels, MRI, CT. In old age, the death of neurons is explained by natural causes; treatment in this case is aimed at slowing down the process.
Multiple lesions
Acute and chronic cerebral circulatory disorders and injuries lead to the appearance of several islands of gliosis. During the development of the pathology that caused the death of neurons, the number and size of altered areas may increase.
Multiple foci of gliosis cause disruption of the central nervous system, increasing the clinical manifestations of the underlying disease. More often, the causes of several (more than 3) affected areas are strokes, heart attacks, atherosclerosis and compression of cerebral vessels.
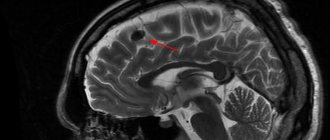
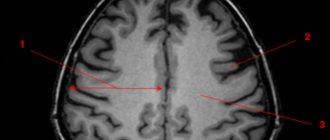
Multiple foci of gliosis (shown by arrows) on MRI
Diet
There is no special diet, but it is recommended to adhere to the diet recommended for the underlying disease that initiates the process of formation of glial lesions ( Diet for stroke , Diet for hypertension , atherosclerosis , diabetes mellitus , Diet for obesity , etc.). In general, it is recommended to adhere to a low-calorie diet with sufficient vitamin content (vegetables, fruits) and a minimum content of animal fats in the diet.
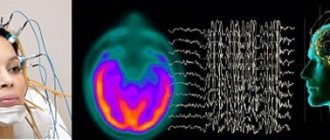
What does gliosis look like on an MRI?
Magnetic resonance imaging is the most effective type of diagnostics of brain diseases. Layer-by-layer scans visualize the slightest changes in the structure of the cerebral substance, making it possible to clarify the size and location of the pathological area.
Single foci of gliosis on MRI of the brain on T1-weighted images appear as light spots with a clear border. A change in color indicates white matter dystrophy and pathological proliferation of glial cells.
The advantage of MRI is the ability to assess the condition of the tissues located around the glial lesion, the nature of the blood supply to the scanned area (including the supratentorial space). Layer-by-layer images visualize changes in cerebral structures and dysfunction of the vascular system. MRI allows for timely diagnosis of pathological processes that cause neuronal death and facilitates the appointment of effective treatment.
Tomograms with gliosis of vascular origin show disturbances in the patency of the veins and arteries of the brain, areas of compression, and narrowing of the lumen of the bloodstream. The method reflects changes characteristic of demyelinating, necrotic, ischemic, and inflammatory processes.
Magnetic resonance imaging is informative regarding pathologically changed areas in the frontal lobes and allows identifying periventricular gliosis localized in the region of the ventricles of the brain. Single lesions with a diameter of 3 mm in the supratentorial space are clearly visible on MRI images.
List of sources
- Vereshchagin N.V., Gulevskaya T.S. Pathology of the brain in atherosclerosis and arterial hypertension. – M.: Medicine, 1997. – 228 p.
- Vasiliev V.N., Kindyashova V.V., Kozhevnikova V.V., Tikhomirova O.V., Lomova I.P., Serebryakova S.V. Clinical and diagnostic significance of microfocal brain lesions of vascular origin among management specialists // Medical, biological and socio-psychological problems of safety in emergency situations. 2014. No. 3. pp. 27-32.
- Gladky P. A., Sergeeva I. G., Tulupov A. A. Infectious lesions of the brain. Tutorial. Novosibirsk 2015. – 24 p.
- Putilina M.V. Chronic cerebral ischemia//Attending physician. 2005. No. 5.
- Yanishevsky S.N. Brain damage in patients with type 2 diabetes // International Journal of Endocrinology. No. 8(64). 2014 pp. 89-97.
MRI results: cerebral gliosis
The study protocol includes a description of the state of the sub- and supratentorial space. Based on the results of an MRI of the brain, the doctor evaluates:
- location of midline structures;
- perivascular spaces of the frontal, parietal lobes; areas of the basal ganglia;
- homogeneity of the white matter structure;
- localization, size of focal changes, presence of perifocal (marginal) infiltration;
- condition of the pituitary gland, ventricles of the brain;
- the presence of pathological formations;
- functionality of blood vessels in the area of interest.
If there are characteristic foci of gliosis, the doctor clarifies the genesis of the changes, indicating the main diagnosis in the conclusion.
Foci of gliosis (shown by arrows) on an MRI image of the brain in axial projection
If you suspect any cerebral pathologies, you can undergo an MRI at the Magnit diagnostic center.
Cystic formations
Neuroglial cysts are a fairly rare finding as a result of MRI diagnostics. A benign cystic lesion can potentially occur anywhere in the brain. Glial tissues act as a kind of cement, forming space for neurons and protecting them. With the help of glia, neuronal tissue is nourished. The images show parenchymal cysts with smooth, rounded borders and minimal reflective signal. Glionic cysts account for less than 1% of intracranial cystic formations.
Most often, glial cysts are congenital pathologies that occur during the development of the fetal neural tube, when glial cells grow into membrane tissue, inside which the white tissue of the spinal cord will be located. The formations can be intra- or extraparenchymal, with cysts of the first type being more common. The frontal lobe of the brain is considered the most typical location.
An X-ray or CT scan reveals a cavity filled with cerebrospinal fluid, with swelling of the surrounding tissues. These cavities do not harden. They must be distinguished from arachnoid cysts, dilation of the perivascular space, neurocysticercosis (infection with bovine tapeworm larvae), ependymal and epidermoid cysts.
Typically, glial cysts do not manifest themselves in any way; they are incidental findings during examination for other disorders and diseases. One of the mistakes of MRI diagnostics is the difficulty in identifying a glial cyst and gliosis or degeneration of brain tissue.
Diagnostics
To identify changes in the structure of the brain matter, neuroimaging methods are mainly used - MRI and CT studies. The study of microstructural changes that have occurred in the white matter is performed using the DT-MRI method (diffusion tensor MRI). The study reveals anisotropy (different structure of individual areas) of the white matter, which manifests itself in different degrees of myelination, direction and diameter of the fibers.
Neuroimaging reveals the primary disease that provoked the proliferation of neuroglia. Angiography allows you to determine the condition of the elements of the vascular system and the disorders that have arisen against the background of atherosclerotic vascular lesions. The brain of children under 1 year of age is examined using neurosonography.
Symptoms
Damage to this type of tissue is usually accompanied by the following symptoms:
- sudden surges in pressure;
- regular headaches localized in various areas;
- decreased sensitivity;
- stiffness of movement, gait changes due to problems with the sense of balance;
- frequent dizziness;
- there is a sharp deterioration in vision and hearing;
- speech problems;
- simple mental actions begin to cause problems, memory deterioration appears.
Symptoms also include aggression and tearfulness. Neurotic changes may be observed, headaches will not be constant. In some cases, nausea, epilepsy attacks, and difficulty pronouncing certain words and even phrases appear.
Causes
Any tissue changes can occur for various reasons, including congenital disorders. The main ones are:
- as a result of surgery;
- with excessive alcohol consumption;
- natural aging;
- as a result of a heart attack, after hemorrhage;
- after inflammation of the meninges;
- birth and other injuries;
- atrophic tissue disorders, demyelinating encephalitis, and multiple sclerosis.
It should be borne in mind that in adults, as a result of timely detection of the disease and treatment, it is possible to protect the source of the spread of changes. But for children, such chances are extremely small; they rarely live more than 3 years.
Treatment
There is no specific treatment for cystic-glial changes that have occurred in the brain. The main task of the doctor is to stop the progression of the pathological process. Drug therapy prescribed by a doctor involves taking drugs that improve the activity of brain structures:
- Nootropic.
- Prevents the formation of blood clots.
- Improving the rheological characteristics of blood.
- Stimulating cerebral blood flow.
- Normalizing blood pressure indicators.
- Painkillers, antispasmodics.
- Strengthening the walls of blood vessels.
- Activating metabolic processes in brain tissue.
- Antioxidants, vitamins.
Surgical intervention is indicated if the cystic gliosis formation is large in size and compresses the surrounding tissues, which provokes a mass effect and is associated with the appearance of severe neurological symptoms.