MRI of the veins of the brain is a modern diagnostic technique that allows you to obtain an accurate picture of the veins and determine the slightest deviations in the functioning of the vascular system.
Magnetic resonance imaging of veins is used to diagnose a wide range of diseases. The method is based on the effect of magnetic radiation on human tissue, which is absolutely safe and makes it possible to accurately visualize the structure of brain vessels.
Diagram of cerebral circulation on an MRI scan
Anatomy of cerebral veins, what is visible on MRI?
Veins are blood vessels that are designed to drain blood from the brain. Oxygenated blood enters the nerve center through the arteries, and after giving nutrients and oxygen to the cells, the blood returns to the heart through the veins.
Disturbances in the functioning of the cerebral veins can contribute to poor health, fatigue and the gradual development of cerebral edema. This is why timely and accurate diagnosis is so important.
Examination of the condition of the venous bed using a magnetic resonance imaging scanner is called MR venography.
In terms of information content, MRI of the arteries and veins of the brain is one step ahead of traditional diagnostic methods using X-rays or ultrasound. Using MR images, diagnosticians receive visual information about the functioning of the veins of the brain.
MR venography allows you to accurately determine:
- anatomical pattern of the venous system;
- congenital and acquired abnormalities in the structure and functioning of blood vessels;
- disturbances in trophism and blood flow from parts of the brain;
- possible damage to blood vessels and their consequences;
- the presence of tumor formations blocking the vascular bed.
A tomography examination is a completely safe procedure that allows not only detailed and high-quality visualization of the structural features of the venous network of the brain, but also scanning for preventive and diagnostic purposes with any frequency without negative impact on health.
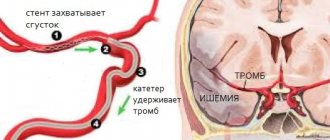
Difficulties in diagnosing thrombosis of the cerebral veins and venous sinuses
The article highlights the difficulties of diagnosing thrombosis of the cerebral veins and venous sinuses. Clinical examples are presented.
Thrombosis of the cerebral veins and venous sinuses is more common in young women than in men, but is generally rare (up to 1% of all cases of cerebral infarction) [1]. According to ISCVT (International Study on Cerebral Vein and Dural Sinus Thrombosis, 2004), the incidence annually is 3–4 cases per 1 million in adults and up to 7 cases per 1 million in children. The mortality rate for this disease ranges from 5 to 30%; during more than 2 years of observation, a corresponding figure of 8.3% was recorded. At the same time, more than 90% of patients had a favorable prognosis. The main risk factors for the development of thrombosis of the cerebral veins and venous sinuses in the population are infectious inflammatory processes (otitis, mastoiditis, sinusitis, septic conditions) and non-infectious causes. Non-infectious causes of thrombosis of the cerebral veins and venous sinuses can be localized or general. The most commonly cited are traumatic brain injury, tumors, head and neck surgery, and pacemaker implantation or central venous catheter placement. Common conditions that contribute to thrombosis of the cerebral veins and venous sinuses include conditions such as hemodynamic compromise (eg, congestive heart failure, dehydration), blood disorders (polycythemia, sickle cell disease, thrombocytopenia), and coagulopathy (disseminated intravascular coagulation syndrome). , deficiency of antithrombin, protein C and protein S), as well as thrombophilic conditions associated with pregnancy, childbirth and the use of oral contraceptives, antiphospholipid syndrome, systemic vasculitis. However, in 15% of cases the cause of sinus thrombosis remains unknown [5]. Difficulties in diagnosing thrombosis of the cerebral veins and venous sinuses are due to the polymorphism of its clinical picture and the variability of the structure of the cerebral venous system. Anatomical features of the structure of the cerebral venous system In the development of thrombosis of the cerebral veins and sinuses, an important role is played by the anatomical features of the structure of the cerebral venous system (Fig. 1). Unlike arteries and peripheral veins, cerebral veins lack a muscular wall and valve apparatus. The venous system of the brain is characterized by “branching”, a large number of anastomoses and the fact that one vein can receive blood from the basins of several arteries. Cerebral veins are divided into superficial and deep. Superficial veins - the superior cerebral vein, the superficial middle cerebral vein (Labbe vein), the inferior anastomatic vein (Trolar vein), the inferior cerebral veins - lie in the subarachnoid space and, anastomosing among themselves, form a network on the surfaces of the cerebral hemispheres. The main mass of venous blood from the cortex and white matter flows into the superficial veins, and then into the nearby sinus of the dura mater. Blood enters the deep cerebral veins from the veins of the choroid plexus of the lateral ventricles, basal ganglia, thalami, midbrain, pons, medulla oblongata and cerebellum. The superficial and deep veins drain into the sinuses of the dura mater. The superficial veins drain mainly into the superior sagittal sinus. The main collectors of the deep veins are the great cerebral vein (vein of Galen) and the straight sinus. Blood from the superior sagittal and straight sinuses enters the transverse and sigmoid sinuses, which collect blood from the cranial cavity and drain it into the internal jugular vein. In the development of thrombosis of the cerebral veins and venous sinuses, 2 mechanisms are involved that determine the symptoms of the disease. The first is occlusion of the cerebral veins, causing cerebral edema and impaired venous circulation. The second link in the pathogenesis of thrombosis of the cerebral veins and venous sinuses is the development of intracranial hypertension due to occlusion of large venous sinuses. Normally, cerebrospinal fluid is transported from the cerebral ventricles through the subarachnoid space of the lower and superolateral surfaces of the cerebral hemispheres, adsorbed in the arachnoid plexuses and flows into the superior sagittal sinus. With thrombosis of the venous sinuses, venous pressure increases, as a result of which the absorption of cerebrospinal fluid is impaired and intracranial hypertension develops [5]. Both of these mechanisms determine the clinical symptoms of sinus thrombosis.
Clinic and diagnosis Clinical manifestations of thrombosis of the cerebral veins and venous sinuses depend on the location of thrombosis, the speed of its development and the nature of the underlying disease. Severe disorders of the venous circulation are characterized by headache, vomiting, swelling of the optic discs, focal and generalized convulsions, and progressive depression of consciousness. However, with early recognition of the process, the clinical picture may be less pronounced. Focal neurological disorders can occur with isolated thrombosis of deep or superficial veins or with the spread of thrombosis from the sinuses to the veins. Meningeal syndrome is considered a rare manifestation of uncomplicated sinus thrombosis. Cerebrospinal fluid pressure, according to most authors, is normal or moderately elevated. The composition of the cerebrospinal fluid can be either unchanged or with a slightly increased protein content and pleocytosis of no more than 200/3 [1, 11–13]. Septic thrombosis of the transverse and sigmoid sinuses is characterized by a pronounced range of body temperature, leukocytosis, and accelerated ESR, but the use of antibiotics can smooth out these manifestations. Swelling of the mastoid area, pain on palpation, and less filling of the internal jugular vein on the affected side are very common. Sometimes thrombosis of the sigmoid sinus spreads to the internal jugular vein, which is accompanied by local inflammatory changes along the vein [1]. In contrast to arterial thrombosis and thromboembolism, neurological symptoms in thrombosis of the cerebral veins and venous sinuses more often develop subacutely - within a period of several days to 1 month. (50–80% of cases), although an acute onset may also occur (20–30% of cases) [6]. The most common symptom of thrombosis of the cerebral veins and venous sinuses is intense headache (92% of patients), which is a reflection of the development of intracranial hypertension. It resembles the pain of subarachnoid hemorrhage and is not relieved by analgesics. In addition, according to ISCVT et al. [1, 7–13], the following symptoms are identified: – motor disorders – 42%; – convulsive syndrome – 37% (including status epilepticus – 13%); – psychomotor agitation – 25%; – aphasia – 18%; – visual impairment – 13%; – depression of consciousness (stunning, stupor, coma) – 13%; – disorders of the innervation of cranial nerves – 12%; – sensitivity disorders – 11%; – meningeal syndrome – 5%; – vestibulo-cerebellar disorders – 1%. In the long-term period, the most common symptoms are headache (14%) and convulsions (11%). The cavernous and superior sagittal sinuses are relatively rare sites of infection. More often, the intracranial process is the result of the spread of infection from the middle ear, paranasal sinuses, skin near the upper lip, nose and eyes. With thrombophlebitis of the marginal sinus, which usually occurs against the background of inflammation of the middle ear or mastoiditis, pain in the ear and pain when pressing on the mastoid process appear. After a few days or weeks, fever, headache, nausea and vomiting appear due to increased intracranial pressure. Swelling in the mastoid area, dilation of the veins and pain along the internal jugular vein in the neck occur. When the internal jugular vein is involved in the pathological process, pain in the neck and limitation of its movements are observed. Drowsiness and coma often develop. In 50% of patients, swelling of the optic discs is detected (in some patients it is unilateral). Seizures occur, but focal neurological symptoms are rare. The spread of the pathological process to the inferior petrosal sinus is accompanied by dysfunction of the abducens nerve and trigeminal nerve (Gradenigo syndrome). Thrombophlebitis of the cavernous sinus is secondary to oculonasal infections. The clinical syndrome is manifested by swelling of the orbit and signs of dysfunction of the oculomotor and trochlear nerves, the orbital branch of the trigeminal nerve and the abducens nerve. Subsequent spread of infection to the opposite cavernous sinus is accompanied by the occurrence of bilateral symptoms. The disease can begin acutely, with the appearance of fever, headache, nausea and vomiting. Patients complain of pain in the eyeball area, pain in the orbital area when pressed. Chemosis, edema and cyanosis of the upper half of the face are noted. Consciousness can remain clear. Ophthalmoplegia, sensory disturbances in the area of innervation of the ophthalmic branch of the trigeminal nerve, retinal hemorrhages and papilledema may occur. Infection of the superior sagittal sinus can occur when the infection is transferred from the marginal and cavernous sinuses or spreads from the nasal cavity, the focus of osteomyelitis, the epidural and subdural areas. The disease is manifested by fever, headache, swelling of the optic discs. Characteristic is the development of convulsive attacks and hemiplegia, first on one side and then on the other due to the spread of the pathological process to the cerebral veins. Movement disorders may manifest as monoplegia or predominant involvement of the lower extremities. All types of thrombophlebitis, especially those caused by infection of the ear and paranasal sinuses, can be complicated by other forms of intracranial purulent processes, including bacterial meningitis and brain abscess. Due to the absence of pathognomonic clinical symptoms of the disease, instrumental and laboratory research methods are of utmost importance in diagnosing thrombosis of the cerebral veins and venous sinuses. In recent years, the improvement of neuroimaging technologies has opened up new opportunities for the diagnosis of sinus thrombosis (MRI, MR, CT venosinusography). For example, when performing MRI in standard modes, it is now possible to determine signs of venous thrombosis, expressed in increased signal intensity in the T1 and T2 modes, as well as T2-FLAIR from the altered sinus (Fig. 2). When performing MR venosinusography, a decrease in the signal from blood flow in the right transverse sinus is detected, as well as a compensatory increase in the signal from blood flow in the left transverse sinus (Fig. 3). If after an MRI or CT examination the diagnosis remains unclear, it is possible to perform contrast digital subtraction angiography, which can detect not only sinus thrombosis, but also the rare isolated thrombosis of the cerebral veins. Also, during this study, it is possible to identify dilated and tortuous veins, which is an indirect sign of thrombosis of the cerebral venous sinuses [14]. At the same time, a careful assessment of neuroimaging data is necessary to exclude errors in diagnosis, which may include, for example, hypoplasia or congenital absence of the sinus [6, 15]. Treatment As already noted, the development of symptoms in thrombosis of the cerebral veins and venous sinuses is based on occlusion of the cerebral veins and sinuses, changes in brain tissue and the development of intracranial hypertension. This combination is potentially dangerous and may be associated with a poor prognosis in patients with thrombosis of the cerebral veins and venous sinuses. Therefore, it is necessary to carry out complex therapy, including pathogenetic therapy (recanalization of sinuses) and symptomatic therapy (fighting intracranial hypertension, infection) [1, 4, 10]. The main goal of therapy for thrombosis of the cerebral veins and venous sinuses is to restore their patency. Currently, the drugs of choice in this situation are anticoagulants, in particular low molecular weight heparins (LMWH). According to research, the use of direct anticoagulants in the acute period of thrombosis of the cerebral veins and venous sinuses improves the prognosis and reduces the risk of death and disability [16]. In addition, the ISCVT study obtained the following data for 80 patients with cerebral vein and venous sinus thrombosis treated with LMWH: 79% of them recovered, 8% remained mildly symptomatic, 5% had significant neurological impairment, 8% of patients died [1]. These data indicate the effectiveness and safety of the use of LMWH in the acute period of thrombosis of the cerebral veins and venous sinuses. In case of development of septic sinus thrombosis, antibacterial therapy should be carried out using high doses of broad-spectrum antibiotics, such as cephalosporins (ceftriaxone, 2 g/day IV), meropenem, ceftazidine (6 g/day IV), vancomycin ( 2 g/day i.v.). At the same time, there is no consensus on the feasibility and safety of anticoagulant therapy, although most authors adhere to the tactics of managing such patients with LMWH [18]. At the end of the acute period of thrombosis of the cerebral veins and venous sinuses, it is recommended to prescribe indirect oral anticoagulants (warfarin, acenocoumarol) at a dose at which the international normalized ratio (INR) is 2–3. Direct anticoagulants are administered to the patient until the INR reaches target values. In case of thrombosis of the cerebral veins and venous sinuses during pregnancy, the administration of indirect anticoagulants should be avoided due to their teratogenic potential and the possibility of penetration through the placental barrier. In such cases, continued treatment with indirect anticoagulants is recommended [18].
Currently, there are no studies clearly regulating the duration of use of oral anticoagulants. According to the recommendations of EFNS (2006), indirect anticoagulants should be used for 3 months. for secondary thrombosis of the cerebral veins and venous sinuses, which developed in the presence of a so-called transient risk factor, from 6 to 12 months. – in patients with idiopathic thrombosis and in the presence of “minor” thrombophilic conditions, such as deficiency of proteins C and S, heterozygous mutation of Leiden factor or mutations in the prothrombin gene (G20210A). Lifelong anticoagulant therapy is recommended for patients with recurrent venous sinus thrombosis, as well as for the diagnosis of congenital thrombophilic conditions (homozygous Leiden factor mutation, antithrombin deficiency) [17]. In addition to basic therapy, measures should be taken to prevent complications such as seizures and intracranial hypertension. These conditions require management according to general rules (prescription of anticonvulsants, elevated head of the bed, mechanical ventilation in hyperventilation mode with positive expiratory pressure, administration of osmotic diuretics). The effectiveness of glucocorticosteroids for cerebral edema resulting from thrombosis of the cerebral veins and venous sinuses has not been proven [19]. In some cases, in severe forms of thrombosis complicated by dislocation of brain structures, the issue of performing decompression hemicraniotomy, which is a life-saving operation, may be considered [20, 21]. This article presents the case histories of 3 patients who were at different times in the 2nd neurological department of the National Center of Neurology with a diagnosis of cerebral sinus thrombosis. The goal is to demonstrate modern capabilities for diagnosing and treating venous circulatory disorders. Patient K., 31 years old, was admitted to the Scientific Center with complaints of intense headache, nausea, and vomiting. History of illness: within 2 weeks. received treatment for herniated intervertebral discs using large doses of glucocorticosteroids and diuretics. On February 8, 2010, an intense headache that was not relieved by taking analgesics, nausea, vomiting, and photophobia suddenly appeared. The condition was regarded as increased intracranial pressure, and therefore diuretics were prescribed on an outpatient basis. On February 16, 2010, a generalized tonic epileptic seizure suddenly developed. The ambulance team hospitalized the patient to the clinic with a diagnosis of “Subarachnoid hemorrhage. Brain contusion,” which was subsequently removed. After treatment (venotonics, glucocorticosteroids, nootropics), the headache regressed. However, on March 7, 2010, headache, nausea, and vomiting suddenly reappeared. On March 19, 2010, the patient was hospitalized at the NCN. On examination: pronounced expansion of the saphenous veins on the face. The neurological status shows mild stiffness of the neck muscles. There are no focal symptoms. Laboratory research methods. Lupus anticoagulant – 1.10%, negative result. Antibodies to cardiolipins IgG – 15.8 U/ml, the result is weakly positive (normal is up to 10 U/ml). Homocysteine – 16 µmol/l (normal – up to 15 µmol/l). Antigen to von Willebrand factor – 273% (normal – up to 117%). Blood coagulation factors – without deviation from normal values. A blood test for thrombophilic mutations is negative. An examination by an ophthalmologist revealed signs of intracranial hypertension: hyperemia and swelling of the optic discs, dilation and congestion of the veins in the fundus. Instrumental research methods: when performing MRI in T2 mode, an increase in the intensity of the MR signal from the superior sagittal and left sigmoid sinuses was noted (Fig. 4). When performing MR venosinusography, there is no blood flow in both transverse, superior sagittal and left sigmoid sinuses. Noteworthy is the increase in blood flow through the superficial cerebral and facial veins (Fig. 5). Diagnosis: thrombosis of both transverse, left sigmoid and superior sagittal sinuses. Treatment was carried out: nadroparin 0.6 ml 2 times/day subcutaneously for 10 days with a transition to warfarin (INR level 2–3), venotonics (diosmin orally, aminophylline intravenously), carbamazepine (convulsive syndrome). 10 days after the start of therapy, an improvement in well-being was noted - the headache decreased. During MR venosinusography, positive dynamics were noted - blood flow was restored in both transverse sinuses. After 4 months after treatment, the appearance of blood flow through the superior sagittal sinus was noted (Fig. 5). Anticoagulants are continued.
Patient M., 36 years old. She was admitted to the National Center of Neurology with complaints of intense headache and pulsating noise on the right. Life history: migraine attacks without aura have been recurring since adolescence. She took estrogen-containing contraceptives for a long time. Medical history: On August 11, 2009, an intense headache suddenly developed, different in nature from ordinary migraine pain, which was not relieved by analgesics. Later, a pulsating noise in the right ear, a feeling of “heaviness” in the head, nausea, staggering when walking, and weakness appeared. On August 21, 2009, she was hospitalized at the National Center of Neurology. Upon examination: no cerebral, meningeal or focal symptoms were detected. Laboratory research. Lupus anticoagulant – 1.15%, negative result. Antibodies to cardiolipins IgG – 30 U/ml (normal – up to 10 U/ml). After 3 months upon repeated examination at the Rheumatology Center - 10 U/ml, within normal limits. Homocysteine – 11 µmol/l (normal – up to 15 µmol/l). Coagulogram – without features. Blood coagulation factors – without pathology. A blood test for thrombophilic mutations is negative. Instrumental research methods. Standard CT and MRI revealed no pathology. Contrast CT angiography revealed the absence of a signal from blood flow along the right sigmoid sinus (Fig. 6). Thrombosis of the right sigmoid sinus was diagnosed.
Treatment was carried out: nadroparin 0.6 ml 2 times/day subcutaneously with a transition to warfarin with an INR of 2–3 (6 months), aminophylline, rutoside. Due to repeated migraine attacks and prolonged pain syndrome, propranolol and antidepressants from the selective serotonin reuptake inhibition group were prescribed. During treatment, the headache disappeared. After 6 months During a control study (MR venosinusography), restoration of blood flow through the right sigmoid sinus was noted (Fig. 7). Taking into account the absence of signs of coagulopathy and a verified cause of sinus thrombosis, anticoagulant therapy continued for 6 months.
Patient K., 56 years old, was admitted on August 13, 2010. She made no complaints due to decreased criticism of her condition. Life history: arterial hypertension, deep vein thrombosis of the legs. History of the disease: On August 13, 2010, the color perception of surrounding objects suddenly became impaired (the color of the house changed). Relatives noticed inappropriate behavior - the patient began to “talk.” Weakness developed in the left arm and leg, walking was impaired, and convulsive twitching appeared in the left arm and leg. The ambulance team transported her to the National Center. On examination: partially disoriented in place and time. Adynamic. Sleepy. Reduced criticism of one's condition. Speech is not impaired. Meningeal symptoms are negative. There are no oculomotor disorders. The face is symmetrical, the tongue is in the midline. There are no bulbar disorders. Mild left-sided hemiparesis with increased muscle tone of the plastic type. Tendon and periosteal reflexes are alive, S>D. Babinski reflex on the left. In the left limbs there are periodic clonic convulsive twitches of varying amplitude, lasting up to 1 minute. There are no sensory disorders. Laboratory tests: homocysteine – 39 µmol/l (normal – up to 15 µmol/l), von Willebrand factor antigen – 231% (normal – up to 117%). Lupus anticoagulant – 1.1%, negative result. Antibodies to cardiolipins IgG – 24 U/ml, the result is weakly positive (normal is up to 10 U/ml). Blood coagulation factors – without pathology. An examination by an ophthalmologist revealed signs of obstructed venous outflow. Instrumental studies: MRI of the brain revealed an infarction with a hemorrhagic component, complicated by subarachnoid hemorrhage in the right hemisphere of the brain, as well as thrombosis of the right transverse sinus (Fig. 8). Diagnosis : infarction with a hemorrhagic component in the right hemisphere of the brain due to thrombosis of the right transverse and sigmoid sinuses, complicated by subarachnoid hemorrhage.
Treatment was carried out: enoxaparin 0.4 ml 2 times/day subcutaneously with a transition to warfarin (continuous use) under the control of INR 2–3; venotonics (rutoside, aminophylline). Due to the detected hyperhomocysteinemia, folic acid and vitamin B12 were also prescribed. In addition, antihypertensive therapy was carried out. After 10 days from the start of therapy, the disappearance of clonic twitching in the left arm and leg, an increase in strength and range of motion were noted, the patient became more adequate, oriented in place and time. Upon repeated examination, the appearance of a signal from the blood flow along the right transverse sinus was noted (Fig. 9). Taking into account thrombosis of the right transverse sinus, a history of deep vein thrombosis of the legs, and an increase in homocysteine levels, the patient was recommended for continuous therapy with anticoagulants and folic acid.
Conclusion In the 3 demonstrated cases, among the possible causes, the increased thrombogenic potential of the blood (increased level of von Willebrand factor antigen, hormonal therapy, hyperhomocysteinemia) should apparently be given first place. The thrombophilic state could serve as a trigger for the development of venous sinus thrombosis. Thus, in this situation, the main direction of pathogenetic therapy is the prescription of direct anticoagulants with a transition to indirect anticoagulants and maintaining INR values at 2–3. In addition, the importance of a thorough history taking has been demonstrated, in particular, close attention to the presence of an infectious process, traumatic brain injury, venous thrombosis, and taking medications that can provoke the development of a hypercoagulable state. The importance of a physical examination is also emphasized, which may reveal indirect signs of impaired venous outflow through the cerebral veins and venous sinuses (dilation of the facial veins in the first patient). In 2 patients, examination of the fundus revealed signs of impaired venous outflow and intracranial hypertension: congestive, swollen, hyperemic optic discs, dilated, congested veins in the fundus, absence of spontaneous venous pulse. All these signs, along with an indication of a new-onset, intense, difficult-to-treat headache, should give the clinician a reason to exclude disorders of cerebral venous circulation, which in turn is the key to successful treatment of patients and secondary prevention of this type of pathology.
How to do an MRI of cerebral veins
The classic MR venography protocol is a cycle of several sequential actions:
- the patient is placed on a horizontal platform in the “supine” position, a special RF coil is installed in the head area, which amplifies the tomograph signal;
- the moving part with the person is directed into a round magnet;
- Doctors go into the next room to monitor the operation of the devices on the computer.
You need to be prepared that during operation, medical equipment may make sounds in the form of pops, clicks or knocks. To make the process more comfortable, medical patients are offered to wear headphones and undergo the screening accompanied by pleasant musical accompaniment.
MRI with contrast
In most cases, MRI is able to convey a fairly clear image even without the use of contrast. But, occasionally, for a certain pathology, when targeted thoroughness of the examination is required, a contrast agent may be used.
Contrast is used if a tumor is suspected. A substance that can accumulate in pathologically altered structures and clearly display them on photographs.
Thanks to this, the location of a benign or malignant tumor that interferes with venous outflow, damage and changes in the structure and functioning of the brain veins is accurately determined.
In most cases, the contrast agent is safely eliminated by the body without any negative consequences. Patients with a history or a tendency to allergic reactions are first tested for sensitivity to the dye.
Indications and contraindications for MRI of cerebral veins
Indications for magnetic resonance imaging of cerebral veins may include the following symptoms and conditions:
- frequent headaches;
- sudden dull headache;
- traumatic brain injuries;
- tinnitus, dizziness, fainting;
- a feeling of pressure and fullness in a certain area of the head;
- feeling of pressure on the eyeballs;
- coordination problems;
- problems with memory, speech;
- a sharp decline in cognitive abilities and the ability to concentrate in young patients;
- cognitive impairment in older people;
- single or repeated epileptic seizures.
If one or more of the above symptoms occur, patients should consult a doctor who will give a referral for an MRI of the veins of the brain.
Diagnostician prepares patient for examination
MR venography can be indicated not only in the presence of any ailment, but also for preventive purposes for the early detection of vascular diseases.
Contraindications to the procedure
MRI is considered a safer method of visual diagnosis of internal body structures than CT. However, MR scanning also has a number of contraindications, which can be divided into absolute and relative.
Absolute contraindications include:
- the presence of metal objects in the body (fragments from wounds, shot);
- a pacemaker or neurostimulator installed in the patient;
- cochlear implants, vascular clips;
- the patient’s weight category is over 130 kilograms and body girth from 150 centimeters;
- first trimester of pregnancy;
- age up to 5 years.
Before prescribing a referral for an MRI of the cerebral veins, the doctor must check the patient for the presence of risk factors.
Relative contraindications do not negate the diagnosis, but require careful preliminary preparation. The procedure is not indicated in the case of:
- severe damage to the cardiovascular system in the acute stage;
- presence of tattoos on the body containing paint with metal particles;
- mental disorders in the acute stage;
- fear of being in a confined space;
- inability to maintain long-term immobility.
Prostheses made of non-ferromagnetic materials do not prohibit MRI screening if the following requirements are met:
- availability of documents for the prosthesis;
- the prosthesis was installed no later than 3 months before the diagnosis;
In addition, if the prosthesis is located outside the scanning area, its presence will not interfere with the screening.
Difficulties in diagnosing thrombosis of the cerebral veins (CV) and venous sinuses (SV) are associated with the variety of clinical manifestations, the localization of thrombosis, the rate of its development, and the cause of the disease [1–3]. The MV and dural sinuses contain about 70% of the blood flowing to the brain, however, thrombosis of the MV and VS is much less common than arterial thrombosis. The course of thrombosis of MV and VS is extremely variable - from progressive and recurrent to benign and curable [4].
This disease has been known for more than 200 years - the first description of thrombosis of MV and VS was made by J. Morgagni in 1761 [5]. In 1825, the French physician M. Ribes [6] described a patient with headache, epileptic seizure and delirium, who was found to have thrombosis of the MV and VS.
Large epidemiological and clinical studies are limited by the small number of patients with CF and VS thrombosis. Most publications about this disease are casuistic reports. Results from multicenter studies have only been published within the last 15 years, including the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVDST) [7], based on 624 observations. The Italian registry includes data from 706 cases of MV and VS thrombosis [8]. One of the latest retrospective studies [9], including 152 patients with MV and VS thrombosis, was conducted in 2021.
Epidemiology
To date, there are no epidemiological studies on MV and VS thrombosis, so the exact incidence rate is unknown. The first data on the incidence of MV and VS thrombosis were obtained from autopsy results. H. Ehlers and C. Courville [10] in 1936, summarizing the results of 12,500 autopsies, identified 16 cases of thrombosis of MV and VS, but data from modern studies [4] indicate that the incidence is 10 times higher.
The prevalence of MV and VS thrombosis is heterogeneous. In most patients, the disease develops between the ages of 20 and 50 years. Children and elderly people also get sick. In this regard, the epidemiology of the disease is separately described for different age groups. According to ISCVDST, the incidence of thrombosis of MV and VS in adults is 3-4 cases per 1 million, and in children and newborns - 7 cases per 1 million child population. Until the mid-60s, the incidence of thrombosis of MV and VS in men and women was considered equal, however, according to recent reports [7], thrombosis of MV and VS occurs more often in women, especially in the age group from 20 to 35 years (male: female ratio equals 3:1). The high prevalence of the disease in women of childbearing age is most likely associated with pregnancy, the postpartum period, and the use of oral contraceptives [11]. According to a study conducted in the USA in 1993-1994, about 12 births out of 100,000 are complicated by the development of MV and VS thrombosis [7]. An increase in the proportion of women among patients with MV and VS thrombosis over the past decade has been shown; currently it is about 70%. The predominance of female patients is explained by hormonal factors. About 1/3 of women of childbearing age in Western countries use oral contraceptives, which accounts for approximately ½ of patients with MV and VS thrombosis [12].
There are no reliable data regarding geographic or ethnic differences in incidence, but several studies have reported noteworthy results. In 2021, data from a study were published in the Adelaide region (Australia) with an adult population of about 1 million. In a retrospective analysis of all cases of MV and VS thrombosis for the period 2005-2011. the incidence was 15.7 cases per 1 million population per year; an almost equal distribution of patients by gender was found (52% women, 48% men) [13]. Prevalence of MV and VS thrombosis in the Netherlands in 2008–2010. amounted to 13.2 cases per 1 million population; to Hamadan (Iran) in 2009-2015. — 13.5 cases per 1 million population [12].
Localization
Thrombosis is more often localized in the dural sinuses than in the M.V. The most common thrombosis is the superior sagittal, sigmoid and transverse sinuses, and then - in descending order: thrombosis of the cortical veins, cavernous sinus, cerebellar veins. Thrombosis of the superior sagittal sinus occurs in 46% of cases, sigmoid or transverse sinuses - in 32%, several sinuses - in 20%, superior sagittal sinus and superficial cerebral veins - in 40% of cases [4]. In 2/3 of cases, thrombosis is not limited to one sinus, but spreads to adjacent sinuses and veins. Isolated thrombosis of the superior sagittal sinus is observed in 13-55% of cases, sigmoid and transverse sinuses - in 10%; in 40% of cases, sinus hypoplasia is observed, which is difficult to distinguish from thrombosis [14].
In a retrospective study by J. Liang et al. [15] the following data were obtained: thrombosis of the superior sagittal sinus occurred in 72.7% of cases, left transverse sinus - in 43.2%, left sigmoid sinus - in 43.2%, right transverse sinus - in 36.4%, right sigmoid - in 36.4%, straight sinus - in 9.1%. In 47.7% of cases, thrombosis of the MV and VS was accompanied by secondary changes in the brain (infarctions were detected in 43.2% of cases, hemorrhages in 27.3%). Most often, secondary changes were localized in the frontal (31.8%) and parietal (36.4%) lobes. Subarachnoid hemorrhages occurred in 13.6% of cases, subdural hematomas - in 4.5%.
L. Zhou et al. [16] revealed thrombosis of the transverse sinus in 65.0% of patients, sigmoid sinus in 55.6%, and superior sagittal sinus in 54.7%. Secondary brain changes were found in 56.4% of patients. Edema of limited areas of the brain was observed in 30.8% of patients, massive edema - in 4.3%, intracranial hematomas - in 15.4%, subarachnoid hemorrhages - in 4.3%.
Risk factors
The diseases that are most often associated with thrombosis of the MV and VS include infections of the orbital region, mastoiditis, inflammatory diseases of the middle ear and face, and meningitis. Inflammatory processes in the area of the mastoid process or face are a predisposing factor for the development of thrombosis of the transverse and sigmoid sinuses. Cavernous sinus thrombosis is caused by infections of the paranasal sinuses (ethmoid and sphenoid) [3, 4]. S. Imam et al. [17] described thrombosis of MV and VS in a 39-year-old patient with chickenpox.
Risk factors for the development of aseptic thrombosis of MV and VS are taking oral contraceptives, pregnancy, the postpartum period, traumatic brain injury (including mild), implantation of a pacemaker or prolonged standing of a subclavian venous catheter with its thrombosis, tumors, collagenosis (systemic lupus erythematosus, disease Behçet, Sjogren's syndrome), blood diseases (polycythemia, sickle cell anemia, thrombocytopenia), antiphospholipid syndrome, thrombophilia (most often caused by mutations in the factor V Leiden and prothrombin genes, deficiency of antithrombin III, protein C), nephrotic syndrome. A history of indications of episodes of increased blood clotting (deep vein thrombosis, thromboembolism of the arteries of the pulmonary trunk system, stroke, myocardial infarction, multiple miscarriages) suggests a state of primary hypercoagulation. Conditions accompanied by secondary hypercoagulation include late pregnancy, childbirth, and the presence of a brain tumor. Hemodynamic disturbances include dehydration, anemia, and congestive heart failure. Changes in the vascular wall can occur as a result of injury, brain tumor, or viral encephalitis [3, 4]. In some cases, a connection between MV and VS thrombosis and temporal arteritis, Wegener's granulomatosis [18] and Churg-Strauss syndrome [19] has been suggested.
In obstetric and gynecological practice, thrombosis of MV and VS mainly occurs in the postpartum period, especially during the first 3 weeks after birth. Risk factors for the development of the disease include dehydration, anemia, cesarean section, arterial hypertension, infectious diseases, maternal age (15-24 years), thrombophilia [4]. Thrombophilia accounts for 34.1% of all causes of thrombosis of MV and VS [4]. Most often we are talking about an abnormality of factor V, which gives it resistance to activated protein C; mutations of the antithrombin III genes and proteins C and S are less common. Thrombosis can also be caused by a deficiency of factors of the anticoagulation system of the blood and resistance of factor V to protein C. In addition, hyperhomocysteinemia predisposes to thrombosis. According to a study by Y. Kapessidou et al. [20], hereditary and acquired forms of thrombophilia were the cause of thrombosis of MV and VS in 64% (7 out of 11) of cases, including protein S deficiency detected in 4 patients, idiopathic thrombocytopenic purpura - in 2 patients (in one case associated with systemic lupus erythematosus, in another - with antiphospholipid syndrome).
Based on the results of several case-control studies [21–23] and one meta-analysis [8], there is a strong association between the use of oral contraceptives and the development of MV and VS thrombosis. The risk of thrombosis may vary depending on the composition of the drugs. Third-generation oral contraceptives are characterized by an increased risk of developing the disease [21], and the risk of its development when using contraceptive patches is similar to the risk when taking oral forms [24]. In approximately 1/3 of the cases cited in the literature, the etiology of MV and VS thrombosis remains unclear [4].
Clinical picture
The clinical picture of MV and VS thrombosis is variable. The average period from the onset of symptoms to diagnosis is 7 days [7]. The most common initial symptom of thrombosis of MV and VS is a sudden intense headache, which, as a rule, is diffuse and difficult to relieve with analgesics. Its course can be acute (less than 48 hours), subacute (from 48 hours to 30 days) and chronic (more than 30 days). Then, focal and general cerebral symptoms such as depression or confusion, epileptic seizures (usually partial with secondary generalization and post-attack paralysis), hemiparesis, aphasia, congestive optic discs, and mental disorders occur. Neurological symptoms in thrombosis of MV and VS most often develop subacutely, in a period from several days to 1 month (in 50-80%), although an acute onset can also be observed (in 20-30%) [25].
The International Headache Society has defined diagnostic criteria for headache in thrombosis of MV and VS:
A. New-onset headache that meets criteria C and D.
B. Thrombosis M.V. and VS diagnosed using neuroimaging methods.
C. Simultaneous development of headache, focal neurological symptoms and thrombosis of the MV and VS.
D. Headache that regresses within 1 month after the start of specific treatment.
With thrombosis of the MV and VS, venous congestion develops in the brain due to obstruction of venous outflow. Irritation of the receptors located in the wall of the MV and the interoceptors of the meninges with increased pressure in the venous system of the brain causes the appearance of headaches. Disruption of venous outflow leads to an increase in intracranial pressure and the development of hypoxia, resulting in necrotic changes in brain tissue. About 90% of patients describe persistent intense headache, more pronounced in the morning, as the main complaint with thrombosis of MV and VS. Typically, pain increases when the patient is in a horizontal position [25, 26].
Headache due to thrombosis of MV and VS has no specific features. Its clinical manifestations depend on the location and severity of thrombosis, the age of the patient, and the time from the onset of the disease. It is less common in elderly patients than in young patients, which may be due to a lower incidence of intracranial hypertension and decreased activity of the pain perception system in the elderly [26].
Headache due to thrombosis in 50% of cases has a subacute onset, intensifies over several days, but can be paroxysmal in nature. In 10% of cases, a thunderclap headache occurs. Gradually, the pain becomes persistent, refractory to painkillers and persists at night, intensifying with physical activity and the Valsalva maneuver.
Subjective characteristics of headache have no diagnostic value. Diffuse, predominantly bursting, headache is more common, and local pain is less common (42%). The intensity of pain is usually moderate or high. In most cases, headaches worsen at night and early morning, accompanied by nausea, vomiting and phonophobia. It can imitate migraine, tension headache, cervicalgia and is in no way related to the localization of the pathological process [27].
Headache may be a consequence of the chronic course of thrombosis of MV and V.S. Its peculiarity is that there are no indications of an acute episode of headache or the occurrence of neurological symptoms, however, MRI in the venosinusography mode reveals signs of thrombosis of one of the V.S. The predominant type is a bilateral headache of a pressing or bursting nature with a tendency to persist, aggravated by physical stress or emotional experience [2].
A prospective study examined headache characteristics in 123 patients with MV and VS thrombosis. Patients with intracranial hypertension and meningitis were excluded from the study. It was shown that in 14% of patients, headache was the only manifestation of the disease. In 88% of patients, thrombosis involved the transverse sinuses, and almost all (except one) cases of unilateral venous thrombosis had ipsilateral headache. Patients often characterized the headache as constant, one-sided, of high intensity and pulsating in nature. In most cases, patients noted a sudden onset of the attack; 3 patients described the “thunderous” nature of the headache. The pain syndrome regressed within several days or weeks after the start of treatment for MV and V.S. thrombosis. The prognosis was favorable in all cases. The authors suggested that the pathogenesis of headache in the absence of intracranial hypertension is associated with irritation of nerve endings in the walls of occluded MVs and VSs [28].
Swelling of the optic discs is observed in 45-86% of patients with thrombosis of the MV and V.S. The initial manifestations may be epileptic seizures, the frequency of which ranges from 10 to 60%. Focal neurological symptoms (paresis, dysarthria, visuospatial disturbances, homonymous hemianopsia) occur in 15% of patients [7, 27].
The results of a three-year clinical study of patients with MV and VS thrombosis showed that 60% (29 out of 48) of patients developed headaches: migraine (14), tension-type headache (13), other types of headache (2). Upon further evaluation (mean period 44 months), chronic migraine was diagnosed in 25% (6 of 24) of patients. Microhematomas were detected in most patients. In a study by R. Cumurciuc et al. [29] in 30% of patients with thrombosis of MV and VS, chronic headache was observed within 3 months. In a retrospective study by L. Zhou et al. [16], which included 117 patients with thrombosis of the MV and VS, it was shown that headache was observed in 87.2% of patients, epileptic seizures - in 31.6%, focal neurological symptoms - in 29.9%, visual disturbances - in 26.5%, disturbances of consciousness - in 15.4%.
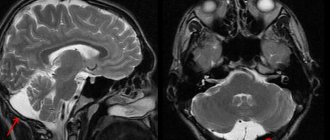
Diagnostics
Due to the absence of pathognomonic clinical symptoms, instrumental research methods are of utmost importance in the diagnosis of MV and VS thrombosis. In recent years, the improvement of neuroimaging technologies has opened up new opportunities for diagnosing the disease (MRI, MRI and CT venosinusography). Under K.T. and MRI in standard modes can reveal cerebral edema, foci of necrotic changes in brain tissue, a filling defect in the area of confluence of sinuses (“delta sign”), as well as signs of venous thrombosis (increased signal intensity from an altered VS in T1 and T2 modes, and also T2-FLAIR) [2, 3, 30].
If after MRI or CT the diagnosis remains unclear, it is possible to perform digital subtraction angiography, which can detect not only VS thrombosis, but also the rare isolated MV thrombosis. Also, during digital subtraction angiography, it is possible to detect dilated and tortuous veins, which is an indirect sign of V.S. thrombosis. At the same time, a careful assessment of neuroimaging data is necessary to exclude diagnostic errors that may be caused, for example, by hypo- or aplasia of the sinuses [2, 3]. In a recent study by J. Kang et al. [31] it was shown that the ASL perfusion method with MRI allows diagnosing MV and VS thrombosis with high accuracy.
If hereditary thrombophilia is suspected, the level of homocysteine, the concentration and activity of antithrombin III, proteins C and S, and thrombophilic mutations are determined: mutations in the methylenetetrahydrofolate reductase gene - C 677 T
;
mutations in the blood coagulation factor V gene - G 1691 A
(factor V Leiden);
mutation in the prothrombin gene - G 20210 A
[2, 3, 25].
When taking oral contraceptives and liver disease, the concentration of all three factors of the blood anticoagulation system decreases simultaneously, and during pregnancy, primarily proteins C and S. With nephrotic syndrome, the concentration of antithrombin III decreases, and proteins C and S increase. Disorders of the anticoagulation system of the blood are far from the only cause of thrombosis of MV and VS: the disease can be caused by antiphospholipid syndrome and coagulopathy. The diagnosis is confirmed by the study of lupus anticoagulant, antibodies to cardiolipin and β2-glycoprotein, blood clotting factors, and determination of von Willebrand factor.
Treatment
The main goal of treatment for thrombosis of MV and VS is to restore their patency. According to various studies, the use of direct anticoagulants in the acute period of thrombosis of MV and VS improves the prognosis and reduces the risk of disability. The effectiveness of heparin in therapeutic dosage has been proven in double-blind, placebo-controlled studies. The hemorrhagic component in thrombosis of MV and VS is not a contraindication to the administration of heparin in a therapeutic dose. The initial dose of heparin is 5000 units and is administered intravenously as a bolus, after which they switch to intravenous drip administration at a rate of 1000 units/hour. The average daily dose of the drug is 20,000-40,000 units. Activated partial thromboplastin time should be monitored every 3 hours; it should be doubled compared to the norm. If the desired result cannot be achieved, the heparin dosage is gradually increased every 6-8 hours by 100-200 units. Upon completion of the acute phase of the disease, it is recommended to transfer the patient to oral warfarin. In this case, while the administration of direct anticoagulants continues, warfarin is prescribed under the control of the international normalized ratio (INR) (INR 2-3), then heparin is discontinued, and oral administration of warfarin is continued for 8-12 months [4, 32].
In the ISCVDST study [7], 80 patients out of 624 with MV and VS thrombosis received low molecular weight heparins. 79% of them recovered, 8% had mild symptoms, 5% had significant neurological impairment, and 8% died. These data indicate the effectiveness and safety of the use of low molecular weight heparins in the acute period of thrombosis of MV and VS.
J. Scott et al. [33] were the first to report the effectiveness of local thrombolytic therapy (TLT) for MV and VS thrombosis. Along with drug TLT [34], in recent years, for thrombosis of the MV and VS, instrumental methods of removing blood clots from the sinuses of the dura mater have been used - thrombectomy [35] and decompressive craniotomy [30].
Mortality
The mortality rate for thrombosis of MV and VS is 5-10% [5, 30]. The decrease in mortality is due to an increase in the quality of hospital care and improved diagnosis of the disease [36], as well as a decrease in the incidence of traumatic brain injuries and severe infectious diseases. The use of anticoagulant therapy and decompressive craniotomy had a positive effect on patient survival [12, 30].
Recurrent course
The incidence of recurrence of MV and VS thrombosis remains unknown. In a study by P. Palazzo et al. [37], which included 187 patients, the average follow-up period was 73 months, the average duration of anticoagulant treatment was 14 months. Repeated thrombosis of MV and VS was diagnosed in 6 patients, extracranial venous thrombosis - in 19. The rate of recurrence of venous thrombosis after 1 year was 3%, after 2 years - 8%, after 5 years - 12%, after 10 years - 18%. According to the results of the ISCVDST study [7], the incidence of recurrent thrombosis of MV and VS was 2.2%, extracranial venous thrombosis - 3%; the observation period was 16 months.
Forecast
When treatment is started in the early stages of MV and VS thrombosis, the prognosis is favorable in more than 90% of patients. In the absence of treatment for thrombosis of MV and VS, the prognosis is unfavorable in 15% of cases, mortality reaches 10%, but even with significantly pronounced neurological disorders, complete spontaneous recovery is possible. Risk factors for the development of an unfavorable prognosis of the disease are the rapid progression of thrombosis with depression of consciousness, generalized epileptic seizures at the onset of the disease, childhood and old age of patients, localization of thrombosis (cerebellar veins and deep MVs) [4, 7].
The authors declare no conflict of interest.
What does MRI of cerebral veins show?
MRI is a highly accurate method that allows you to obtain a three-dimensional picture of the venous network of the brain in three projections.
MRI screening helps identify a range of potentially life-threatening diseases and conditions:
Venous stagnation
It occurs due to a violation of the ability of blood vessels to perform their function of draining blood from the brain. Stagnation of venous blood contributes to headaches, dizziness, and fatigue. But its main danger lies in the gradual development of oxygen starvation of the brain and swelling, which can lead to serious impairment of well-being.
Neoplasms
Benign and malignant neoplasms can compress the venous bed, complicating the outflow of blood and leading to a rapid deterioration in overall health
Thrombosis of veins and sinuses
Blockage of the venous bed by a thrombus can lead to disruption of the outflow of blood in the brain area. Symptoms appear gradually and often include headache, dizziness, vomiting and confusion. Venous thrombosis rarely develops acutely, often occurring with moderately severe symptoms.
Thrombophlebitis of the cerebral veins
Inflammation that occurs due to blockage of the lumen of a vessel by a thrombus. The disease is accompanied by fever, headaches and vomiting.
Stroke
Cerebral vein stroke is not that common. 98% of cerebral strokes occur due to bleeding from the arteries. The remaining 2% are hemorrhages caused by damage to the veins. Symptoms of the disease develop gradually and may not be taken into account by patients for a long time, which makes diagnosis difficult using conservative methods.
Aneurysm
A protrusion of the vessel wall, which over time can lead to hemorrhage into the medulla.
Encephalopathy
Encephalopathy is the name given to dystrophic changes in brain tissue due to insufficient nutrition and oxygen supply. Encephalopathy can occur, among other things, as a result of disturbances in venous outflow in a local area of the brain or chronic pulmonary and heart failure.
MR venography can detect almost any pathology of the cerebral veins, even at the initial stage of their occurrence.
Intracranial and intravertebral phlebitis and thrombophlebitis
Thrombosis - in case of disruption of the outflow of venous blood from the cranial cavity, venous stagnation develops. There are a number of causes of venous stagnation. Such causes may include heart failure, pulmonary failure, brain tumors, traumatic brain injury, compression of extracranial veins, compression of intracranial veins in the case of craniostenosis and cerebral hydrops, as well as thrombosis of the cerebral veins and dural sinuses. Thrombosis of the cerebral veins can occur against the background of their previous inflammation - thrombophlebitis.
CLINICAL PICTURE AND SYMPTOMS
Thrombosis of superficial cerebral veins
Thrombosis of the superficial veins of the brain in most cases is a complication of various pathological processes in the body, such as inflammation, infectious diseases, surgical interventions, traumatic brain injuries, etc. Sometimes it can be a complication of pregnancy, childbirth, or abortion. The leading role in the pathogenesis of cerebral vein thrombosis is played by a pathological change in their walls, a violation of blood clotting, and a slowdown in blood flow, which leads to the formation of blood clots. Quite often, thrombosis of the cerebral veins is combined with thrombosis of the dural sinuses, as well as with thrombosis of the veins of the lower extremity.
Common infectious symptoms include increased body temperature, changes in blood tests such as increased ESR and neutrophilic leukocytosis. When examining the cerebrospinal fluid, an increase in the amount of protein, slight pleocytosis is noted, and in some cases blood is detected. Quite often, the first manifestations of the disease are headache, nausea, and vomiting. Impaired consciousness may occur in combination with psychomotor agitation. As the disease progresses, focal brain symptoms appear. Focal brain symptoms include epileptic seizures, aphasia, alexia, hemianopsia, paresis and paralysis of the limbs, etc.
The symptoms of superficial vein thrombosis are explained by the fact that against the background of impaired blood outflow, hemorrhagic infarctions develop, localized in the gray and white matter of the brain. In addition, intracerebral and subarachnoid hemorrhages are observed. In most cases, thrombophlebitis of the superficial veins of the brain develops in the postpartum period. In this case, when examining the cerebrospinal fluid, its hemorrhagic nature is noted.
Thrombosis of deep cerebral veins and vein of Galen (great cerebral vein)
Clinically, this disease is characterized by a particularly severe course; in typical cases, the patient’s condition is comatose. During the examination, pronounced cerebral symptoms are noted. The stem and subcortical structures turn out to be functionally incapable. Diagnosing this disease while the patient is alive is extremely difficult. When making a diagnosis, it is necessary to pay attention to the appearance of general local brain symptoms that occur against the background of thrombophlebitis of the upper extremities. Brain symptoms can also occur in the presence of foci of inflammation in the body, which occurs in the postpartum period, with diseases of the paranasal sinuses, ears, etc. In some cases, the disease is characterized by a chronic course over many years.
Thrombosis of the dural sinuses
Often this pathology is formed as a result of the ingress of an infectious agent from a nearby focus, which can be purulent processes in the orbit, paranasal sinuses, purulent otitis, mastoiditis, osteomyelitis of the skull bones, as well as purulent lesions of the scalp and face (boils, carbuncles). The spread of the infectious agent occurs through the diploic and cerebral veins. Thrombosis of the cerebral sinuses can develop against the background of thrombophlebitis of the veins of the upper and lower extremities, as well as the pelvis. In this case, there is a hematogenous mechanism for the development of the disease.
In some cases, thrombosis of the cerebral sinuses is accompanied by thrombophlebitis of the retinal veins, purulent meningitis, and brain abscess. Often, thrombosis of the cerebral sinuses develops in people suffering from tuberculosis, malignant neoplasms, and other diseases in which cachexia develops.
The clinical picture of venous sinus thrombosis is characterized by an increase in body temperature, a sharp headache, accompanied by vomiting. Blood changes in the form of leukocytosis are observed. Symptoms characteristic of increased intracranial pressure are noted. Symptoms of damage to the cranial nerves appear. Patients may be restless and may experience epileptic seizures. In some cases, patients, on the contrary, become drowsy, apathetic, lethargic. Focal symptoms in each specific case correspond to the location of the affected venous sinus.
Thrombosis of the sigmoid sinus
This pathology is the most common. Typically, thrombosis of this sinus develops as a complication of mastoiditis or purulent otitis. The appearance of headache and bradycardia is characteristic. Sometimes patients complain of diplopia. Body temperature rises to high levels, chills appear. The patient's condition may become soporous or comatose. Consciousness is impaired, which is manifested by delirium and agitation. On examination, there is a tilt of the head towards the pathological focus, as well as swelling of the tissue in the mastoid area. When palpated in this area, pain is determined. In some cases, the pathological process may spread to the jugular veins. In this case, symptoms of damage to the glossopharyngeal, vagus and hypoglossal nerves are added to the clinical picture.
Cavernous sinus thrombosis
Thrombosis of the cavernous sinus in most cases develops as a consequence of a septic condition with purulent diseases of the face, ear, paranasal sinuses and orbit. During examination, pay attention to emerging signs of venous stagnation, such as exophthalmos, venous hyperemia of the eyelids and their swelling, swelling of the periorbital tissues, chemosis, congestion in the fundus, and possible atrophy of the optic nerves. Symptoms of damage to the oculomotor nerves usually occur, which is manifested by external ophthalmoplegia. The superior branch of the trigeminal nerve is involved in the pathological process, which is clinically manifested by pain and hyperesthesia in the area of its innervation. Cavernous sinus thrombosis can be either unilateral or bilateral. With bilateral damage, the pathological process can spread to the adjacent sinus.
Thrombosis of the superior longitudinal sinus
The clinical manifestations of this disease depend on its etiology, on the rate of thrombus formation, on its localization in the superior longitudinal sinus, on the degree of involvement of the veins that flow into it into the pathological process. Thrombosis of this sinus can be septic and aseptic in nature. Thrombosis of the superior longitudinal sinus is most severe. When examining the patient, tortuosity of the veins of the temples, forehead, crown, root of the nose, as well as the eyelids is noted, which is associated with their overflow with blood. In addition to congestion and tortuosity of the veins, swelling of the above areas is noted. A characteristic feature of this pathology is the appearance of frequent nosebleeds. On percussion, pain is noted in the parasagittal region. There is an increase in intracranial pressure, and convulsive seizures develop. In some cases, lower paraplegia may occur in combination with urinary incontinence. The above symptoms add up to a general neurological syndrome.
TREATMENT
Treatment should be carried out exclusively by a neurologist. Self-medication is unacceptable.
A necessary condition is the sanitation of the source of infection, which led to the development of thrombosis of the cerebral veins and sinuses. In case of thrombosis or inflammation of the sigmoid sinus of a purulent nature, immediate surgical intervention is necessary. The scope of the operation includes opening and drainage of the area of the primary lesion, as well as opening of the sigmoid sinus and removal of the blood clot.
If thrombosis is complicated by the development of a brain abscess, which is most often localized in the temporal lobe and in the cerebellum, it is necessary to open and drain the abscess cavity. In the case of treatment of cavernous sinus thrombosis, in order to achieve a positive effect, it is necessary to open ulcers localized on the face, in the orbit, paranasal sinuses, etc.