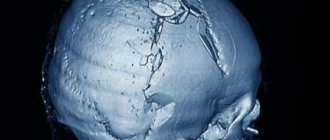
Skull of the “Stettian weaver” (Bonnet. 1904) We continue the series of publications devoted to neurosurgical diseases. The project was prepared jointly with the MBOO for helping children with neurosurgical diseases “He Needs You.” We want these “terrible” diagnoses not to put pressure on parents and not to take away their hope. In our publications, the best specialists and experienced parents will talk about ways to cure and overcome, give recommendations and show that life can go on with any, even such complex, diseases.
About the disease
Among the deformations of the skull there are congenital and acquired.
Congenital ones appear during pregnancy, and the child is born with a certain malformation. Acquired ones occur after childbirth, most often as a result of injury or certain intervention, such as surgery. Craniostenosis in children can be either congenital or acquired after birth. This defect is a premature fusion or absence of sutures in the bones of the skull, which normally should remain plastic for the natural growth and development of the child's brain. As a result, intracranial pressure increases and the shape of the skull changes. If we are talking about a developmental defect, craniostenosis in newborns may be accompanied by other defects that affect the brain and other organs of the body. In the case of an acquired disease, suture fusion occurs due to injury or surgery.
Craniostenosis occurs in one in 1000 newborns.
3242
send an SMS with the donation amount to this number
Others unwillingly
The first written mentions of skull deformation are found in ancient authors. In the V-IV centuries. BC e. Hippocrates, in his text “On Air, Waters and Places,” described the long-headed people, or macrocephals, living on the eastern shore of the Black Sea. Their elongated heads were a sign of belonging to the elite. However, from the text it becomes clear that macrocephals themselves voluntarily deformed the skulls of their babies.
“They consider those with the longest heads to be the noblest. ... as soon as the child is born, while his bones are still soft, his unhardened head is straightened with his hands and forced to grow in length through bandages and other suitable devices, as a result of which the spherical shape of the head deteriorates and its length increases.”
However, modern parents are often faced with congenital, unintentional deformation of the skull. And, unfortunately, it does not make their children a sign of belonging to the elite, rather the opposite...
The word "craniostenosis" comes from the Greek. cranio – “skull” and stenosis – “fusion of bones”. As recognized by the Association of Neurosurgeons of Russia, craniosynostosis (or craniostenosis) is “a disease manifested by the congenital absence or premature closure of the sutures of the skull. Premature synostosis in the area of the sutures of the skull leads to limited growth of the skull in the area of the closed suture, resulting in the development of craniocerebral disproportion. The clinical manifestation of craniocerebral disproportion is intracranial hypertension syndrome.”
Why is craniostenosis dangerous?
The absence of movable sutures in the skull severely limits the brain. Therefore, the sooner help comes for craniostenosis, the higher the likelihood of a complete cure for the child in the future. Compensation mechanisms in infants under 2 years of age are very high, but rehabilitation after this age turns out to be more complex and lengthy. If not treated promptly, the disease can cause the following conditions:
If you do not receive treatment in a timely manner, the disease can cause the following conditions:
- delayed physical, mental, intellectual development;
- disruption of normal brain functions;
- skeletal underdevelopment;
- compression and atrophy of the optic nerve up to complete loss of vision;
- headache;
- ophthalmological diseases;
- death.
Diagnostics
Surgery to eliminate craniosynostosis is indicated for all children, especially those with increased intracranial pressure, who have no contraindications for surgical treatment as such and who do not suffer from severe forms of syndromic craniosynostosis with multiple malformations. Preoperative preparation and planning play a huge role. For this purpose, the following is carried out:
- detailed craniometric measurements with calculation of asymmetry indices;
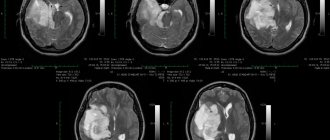
- computed tomography (CT) to detail all the features of craniosynostosis and possible brain damage. A 3D reconstruction of the skull is performed for modeling and planning the operation;
- magnetic resonance imaging (MRI) and MR angiography – if damage to brain tissue or its vessels is suspected;
- neurosonography - ultrasound examination to assess brain structures and the degree of intracranial hypertension.
What is craniostenosis in children?
First of all, it depends on whether the child has other developmental defects. Sometimes pathology accompanies various syndromes - then it is called syndromic. For example, it can occur simultaneously with fusion of fingers or toes, cleft palate or lip, or cerebral hernia.
If fusion of the sutures in the bones of the skull occurs without other developmental defects, it is considered non-syndromic, that is, independent.
Doctors classify the disease into types based on which cranial sutures are fused:
- metopic,
- lambdoid,
- coronary,
- sagittal.
Synostosis - or suture fusion - can involve one to several sutures. There is a concept of pansynostosis - complete overgrowth of all seams. This type of pathology can be considered the most severe; it is less common than others.
Seams that allow movement
The newborn's skull consists of five main bones: a pair of frontal bones, a pair of parietal bones and one occipital bone. These bones are connected by fibrous sutures that allow the bones to move relative to each other, facilitating birth and brain growth.
Normally, the coronal suture separates the two frontal bones from the parietal bones. The metopic suture separates the frontal bones. The sagittal suture separates the two parietal bones. The lambdoid suture separates the occipital bone from the two parietal bones.
But sometimes something goes wrong... Genetic mutations, which can be local in one area or have a systemic, widespread nature, lead to the sutures closing prematurely.
If the closure of one or another suture is accompanied by other anomalies, such craniostenosis is called “syndromic”. Syndromes characterized by premature closure of cranial sutures: Crouzon Syndrome, Apert Syndrome, Pfeiffer Syndrome, Satpre-Hotzen Syndrome, Carpenter Syndrome and others.
Craniostenosis can be a component of various hereditary syndromes. But in most cases, the hereditary nature of the disease is not confirmed, and craniostenosis does not appear in subsequent generations.
An unusually strong degree of craniostenosis (type scaphocephaly) was present in the so-called “Stettian weaver” (Bonnet, 1904). It was a worker from one of the weaving factories in Stettin. His skull was so long and narrow that the back of his head rested against his back when the unfortunate man tried to raise his head. It was said about the “Stettin weaver” that he never saw the sky and always looked gloomily at the ground. Persecuted for his ugliness by ridicule, he died of pleurisy in the 38th year of his sad life...
Sometimes not one, but several seams are subject to early overgrowth. This also leads to deformation of the skull.
In cases where sutures such as the coronal and sagittal close prematurely, the small dimensions of the upper part of the child’s skull seem to be fixed and their increase stops. Since the growth of bones in the preserved sutures of the skull continues, the so-called “tower” head appears in the adult. The skull becomes elongated upward and slightly backward.
How is craniostenosis treated in children?
There is only one way to eliminate the pathology - surgery. It is performed to restore the shape of the skull bones. After the bones take their natural shape, they are held together with mini-screws or mini-plates and surgical wires, which are removed after a year. They are removed after a year. During the operation, doctors use modern, technologically advanced biodegradable material, which does not need to be removed surgically - it gradually dissolves on its own, and in its place, the patient’s own bone tissue grows. This greatly simplifies the patient's recovery.
The best results can be expected if the surgery is performed between 3–4 months and 2 years of age. Severe deformations of the skull can sometimes be noticed only after the bones have completed their formation, that is, at the age of 5–6 years. In such cases, the pathology manifests itself as severe headaches, blurred vision and increased intraocular pressure, increased fatigue and irritability.
If the disease occurs as a response to craniotomy or after injury, the deformed section of the bone is removed and an implant made of modern material - polymer, metal or ceramic - is installed in its place.
Varya and three operations
Elena from Yaroslavl is the mother of eleven children, Varya is the eighth daughter. When Varyukha was born, doctors told her parents that she would live for a maximum of six months. And it will live like a plant. Microcephaly. Severe brain pathology. Her parents could not accept this test and abandoned her.
Three months later, Lena and Vadim Burov saw Varya’s photo in the Federal Base. “The guardians told us that we were crazy. At that time, in addition to our three natural children, we had four adopted children. The repeated commission questioned my husband and me for forty minutes, trying to understand our motives. Finally, we were allowed to take Varya. Nobody believed in her. Nobody believed that we could handle it.
I'll say more. When we arrived at the orphanage and saw her not in a photograph, but in real life, I was scared myself. Will we make it?
Varyusha had a triangular head. She herself was in very strong tension, she did not allow herself to be hugged or pressed. Shackled, she held her hands in front of her, her eyes were bulging, frightened, like those of a wolf cub.
“She’s like this all the time: in high tone, doesn’t smile, doesn’t coo... There are no emotions, there’s nothing,” the employees told us. Well, okay, we think we’ll figure it out... On the second day of our acquaintance, she was already smiling at us from ear to ear, lowering her hands, as if she realized that we were taking her away. At home, after a week and a half, she began to coo... Development began.
At 9 months, Varina’s photographs, thanks to the charitable foundations “Road of Life” and “He Needs You,” ended up in Moscow, at the Scientific Research Clinical Institute of Pediatrics named after Academician Yu. E. Veltishchev. We received a call from the institute with the words: “We looked at your pictures. Varya has severe craniostenosis. I urgently need to go for surgery, my brain is crushed.”
And we went for the first operation to Dmitry Yuryevich Zinenko. It turned out that despite microcephaly, Varya’s brain continued to grow. It is still growing. And the seams on the skull healed prematurely. Craniostenosis was confirmed. The type in which the sagittal suture heals. Scaphocephaly.
Varya had an incision made from her forehead to the back of her head and an artificial fontanelle was made. A day later she began to stand and took her first steps. No support. The brain received nutrition - and a powerful leap in development occurred. She started crawling right there in the department. The entire staff gathered to look at this miracle. She started babbling.
But three months passed, and a keel formed on her forehead. Like a rooster's comb. We went again to the Yu.E. Veltishchev Institute, did a CT scan, and it turned out to be trigonocephaly. Another, metopic, suture has fused.
The condition began to worsen. Varya stood all the time, resting her head on the pillow, and slept only in the fetal position. At night I cried constantly. It was clear that her head was very bothering her. This means the brain has grown.
A few months later she had a second operation. Cut from ear to ear. As Dmitry Yuryevich Zinenko, who again performed the operation on Varya, later said, the brain expanded literally before our eyes during the operation.
Varya began to sleep peacefully and learned to speak in short words. It was obvious that she felt better. Despite the prognosis and microcephaly, her head continues to grow. From the moment of birth to the present day, Varina’s head has grown by 13 cm. This is a very good result. In a healthy child, the head grows 10 cm in the first year of life. But for some reason the bones do not allow the brain to grow, they quickly grow together. There is probably some genetic reason for this...
A year and a half later, Varya’s condition began to deteriorate again. She became lethargic, refused to eat... They did a CT scan, sent me to the Veltishchev Institute, and received the answer: “The brain is compressed. Surgery will be required."
For the third time, Dmitry Zinenko operated again. He said: “If I hadn’t operated on myself last time, I wouldn’t have believed it...” It must be said that Dmitry Yuryevich is the only doctor who did not refuse us. He just saves Varka. Every time. We were turned down by all well-known clinics. The brain is growing, but no one believes that it is growing.
A month after the operation, Varya again experienced a leap in development - she began to pronounce many words at once. The brain receives nutrition - oxygen, and the child develops. Now she will go to kindergarten. At the moment, of course, she has developmental delays. But if you remember that she was given at most six months to live...
She is very active, loves to dance, says “hi” to everyone! and “bye!”, and her funniest word is “pomikaka.” It means "tomato". He loves our next adopted daughter, Sonechka with cerebral palsy, very much. He takes pity on her and always gives her his hands to help her get up.
Of course, at times we have sleepless nights. Sometimes Varya suffers from headaches. And if she doesn’t have any pain, she just wakes up my husband and me, “Dad! Mother!" – and satisfied, she goes to bed next to us. I am sure that any child should be given a chance to cope with the disease and get back on their feet. You can’t give up on a child. Not at all."
If you need medical help or advice, you can submit an application for remote consultation and hospitalization in specialized hospitals here.
Download the leaflet, it contains a lot of useful information: contacts of doctors, information on treatment, care and rehabilitation.
Endoscopic operations
In the last 10-15 years, endoscopic reconstructive operations for craniostenosis have been especially widely used abroad. They are given to children up to 6 months. These are complex operations lasting about 3 hours using special pediatric neuroendoscopes, high-speed drills with specially designed burs that prevent damage to the dura mater and other endoscopic instruments. All manipulations are carried out under video control through an incision of no more than 4-5 cm. Such operations are characterized by low blood loss and a short rehabilitation period. 3-4 days after the operation and control computed tomography, the children are already discharged from the hospital.
In foreign neurosurgical clinics, operations for craniosynostosis are performed only by highly qualified neurosurgeons who specialize in working with young children. They actively use minimally invasive methods of endoscopic correction of cranial deformities, providing excellent functional and cosmetic results with minimal risk of blood loss and postoperative complications.
Modern neurosurgical techniques
In modern neurosurgery, many surgical techniques are used to correct craniosynostosis, the choice of which is made based on the results of the examination, taking into account the form of craniosynostosis and the required volume of intervention. This:
- linear craniotomy;
- circular craniotomy;
- unilateral and bilateral flap craniotomy;
- fronto-orbital extension;
- reconstructive operations with remodeling of the skull bones and various methods of osteosynthesis;
- total reconstruction of the skull bones;
- endoscopic cranioplasty;
- combined reconstructive techniques, for example, a combination of craniotomy and distraction devices or cranial orthoses (orthopedic devices).
Craniotomy operations involve cutting the skull bones parallel to the fused suture and removing 5-10 mm of bone tissue along the cut. Over time, the bone tissue grows and the integrity of the skull is restored. To prevent new premature fusion of bones, their edges are treated with special compounds.
In the case of polysynostosis, flap surgical techniques and multiple fragmentation of the skull bones are often used. In this case, individual small fragments of bone are removed, creating the opportunity for unhindered growth of the skull and brain. Bone flaps correctly aligned during surgery are fixed with bioabsorbable plates and suture material. By the time the physiological shape of the skull is restored, they are utilized by the body, without requiring a new intervention for removal.
If not only the brain, but also the facial skull is deformed, the frontal bone and orbital region are reconstructed and the position of the upper jaw is corrected. Titanium distraction devices of various designs are especially often used for reconstruction of the facial skull. They are installed during surgery. Spring structures begin to gradually move the bones apart immediately after surgery; other models are adjusted manually, starting from the 7th day after surgery in increments of 1 mm per day. Over the course of six months, the distractors form the correct shape and size of the skull, and then are removed.