Cryptogenic epilepsy is epilepsy for which the cause, despite testing, remains unknown. It is difficult to establish the nature of cryptogenic epilepsy, although it manifests itself symptomatically.
Forms of cryptogenic epilepsy:
- Lennox-Gastaut syndrome;
- West syndrome;
- Epilepsy accompanied by myoclonic-astatic seizures;
- Childhood epilepsy with absence seizures;
- Epilepsy with myoclonic absence seizures.
Signs and symptoms of cryptogenic epilepsy
Seizures are the main clinical manifestations of epilepsy. With West syndrome, the first manifestations of epilepsy can be recorded in the first year of a child’s life. Convulsions appear after the child wakes up, and have their own characteristic features. There is a contraction of the muscles of the neck and head on both sides, making a sort of “nodding movement” called “Saalam spasms.”
With Lennox-Gastaut syndrome, seizures are observed from 2 years of age. Manifestations of this syndrome are more often recorded in boys. Seizures have characteristic symptoms. Tonic convulsions occur with vegetative-vascular reactions (heartbeat increases, shortness of breath and redness appear). Due to loss of tone, the child falls and muscle twitching occurs.
Absence is a non-convulsive epileptic seizure that is not accompanied by loss of consciousness.
Symptomatic frontal lobe epilepsy.
The clinical symptoms of frontal lobe epilepsy (FE) are varied. The disease manifests itself in simple and complex partial seizures, as well as, most characteristically, secondary generalized paroxysms. The following forms of LE are distinguished: motor, opercular, dorsolateral, orbitofrontal, anterior frontopolar, cingulate, emanating from the supplementary motor area. Motor paroxysms occur when the anterior central gyrus is irritated. Characteristic are Jacksonian seizures that develop contralateral to the lesion. Convulsions are predominantly clonic in nature and can spread like an ascending (leg - arm - face) or descending (face - arm - leg) march; in some cases with secondary generalization. With a focus in the paracentral lobules, seizures can be observed in the ipsilateral limb or bilaterally. Post-ictal limb weakness (Todd's palsy) is a common phenomenon of LE. Opercular seizures occur when the opercular zone of the inferior frontal gyrus at the junction with the temporal lobe is irritated. Manifested by paroxysms of chewing, sucking, swallowing movements, smacking, licking, coughing; hypersalivation is characteristic. There may be ipsilateral facial twitching, speech disturbances, or involuntary vocalizations. Dorsolateral seizures occur when the superior and inferior frontal gyri are stimulated. They manifest themselves as adverse attacks with forced rotation of the head and eyes, usually contralateral to the source of irritation. When the posterior parts of the inferior frontal gyrus (Broca's center) are involved, paroxysms of motor aphasia are detected. Orbitofrontal seizures occur when the orbital cortex of the inferior frontal gyrus is irritated and are manifested by a variety of autonomic-visceral phenomena. Characterized by epigastric, cardiovascular (pain in the heart, changes in heart rate, blood pressure), respiratory (inspiratory shortness of breath, feeling of suffocation, compression in the neck, “coma” in the throat) attacks. Pharyngo-oral automatisms with hypersalivation often appear. Noteworthy is the abundance of vegetative phenomena in the structure of attacks: hyperhidrosis, pale skin, often with facial hyperemia, impaired thermoregulation, etc. The appearance of typical complex partial (psychomotor) paroxysms with automatisms of gestures is possible.
Anterior (frontopolar) seizures occur when the poles of the frontal lobes are irritated. They are characterized by simple partial seizures with impaired mental functions. They manifest themselves as a feeling of sudden “failure of thoughts,” “emptiness in the head,” confusion, or, conversely, a violent memory; a painful, painful feeling of the need to remember something. A violent “influx of thoughts”, a “whirlwind of ideas” is possible - a feeling of a sudden appearance in the mind of thoughts that are not related in content to the current mental activity. The patient does not have the opportunity to get rid of these thoughts until the end of the attack. Cingular seizures originate from the anterior cingulate cortex of the medial frontal lobes. They manifest themselves mainly as complex, less often simple partial seizures with behavioral and emotional disturbances. Characterized by complex partial seizures with automatisms of gestures, facial flushing, fearful expression, ipsilateral blinking movements, and sometimes clonic convulsions of the contralateral limbs. Paroxysmal dysphoric episodes with anger, aggressiveness, and psychomotor agitation may occur. Seizures emanating from the supplementary motor area were first described by Penfield, but were systematized only recently. This is a fairly common type of attack, especially considering that paroxysms that occur in other parts of the frontal lobe often radiate to the supplementary motor area. Characterized by the presence of frequent, usually nocturnal, simple partial attacks with alternating hemiconvulsions and archaic movements; attacks with cessation of speech, unclear, poorly localized sensory sensations in the trunk and limbs. Partial motor seizures usually manifest themselves as tonic convulsions, occurring either on one side or the other, or bilaterally (at the same time they look like generalized ones). Characteristic is tonic tension with raising of the contralateral arm, adversion of the head and eyes (the patient seems to be looking at his raised arm). The occurrence of “inhibitory” attacks with paroxysmal hemiparesis has been described. Attacks of archaic movements usually occur at night with high frequency (up to 3-10 times per night, often every night). They are characterized by a sudden awakening of patients, screaming, a grimace of horror, a motor storm: waving arms and legs, boxing, pedaling (reminiscent of riding a bicycle), pelvic movements (as during coitus), etc. The degree of disturbance of consciousness fluctuates, but in most cases consciousness is preserved. These attacks should be differentiated from hysterical and paroxysmal night terrors in children. An EEG study for LE may show the following results: normal, peak-wave activity or slowing (periodic rhythmic or continuous) regionally in the frontal, fronto-central or frontotemporal leads; bifrontal independent peak-wave foci; secondary bilateral synchronization; regional frontal low-amplitude fast (betta) activity. Lesions localized in the orbitofrontal, opercular and supplementary motor areas may not show changes when applying surface electrodes and require the use of depth electrodes or corticography. When the supplementary motor area is damaged, EEG patterns are often ipsilateral to seizures or bilateral, or the phenomenon of secondary bilateral Jasper synchronization occurs. Treatment of LE is carried out according to the general principles of treatment of localization-related forms of epilepsy. Carbamazepine (20-30 mg/kg/day) and valproate (50-100 mg/kg/day) are the drugs of choice; diphenine, barbiturates and lamotrigine are reserved. Valproate is especially effective in cases of secondary generalized seizures. If monotherapy is ineffective, polytherapy is used - a combination of the drugs listed above. Complete resistance of attacks to AED therapy is a reason to consider surgical intervention. The prognosis of PE depends on the nature of the structural damage to the brain. Frequent attacks, resistant to therapy, significantly worsen the social adaptation of patients. Seizures originating from the supplementary motor area are usually resistant to traditional AEDs and require surgical treatment.
Diagnosis and causes of cryptogenic epilepsy
It is difficult to accurately determine the causes of this type of epilepsy. However, the doctor, studying outpatient records and conducting a detailed survey, finds out the presence of:
- Fetal hypoxia;
- Presence of intrauterine infection;
- Injuries during childbirth.
An accurate and detailed description of the manifestations of the attack itself plays an important role in diagnosis. Parents should pay close attention, as a preschool child may not always be able to confidently describe his feelings. If parents notice any deviations in the child’s behavior, they should definitely visit a doctor. A pediatrician or neurologist should indicate what you should pay special attention to. The difficulty is presented by absence seizures (non-convulsive seizures), in which the child freezes for several seconds.
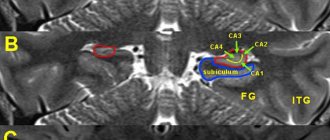
EEG (electroencephalogram) and MRI (magnetic resonance imaging) are used to diagnose cryptogenic epilepsy. The EEG can record typical convulsive activity, which is inherent in generalized seizures. In order to confirm the presence of seizures in a child, overnight video-EEG monitoring is required. This technique is expensive and is carried out only in specialized medical centers. It allows you to confirm or refute the disease with complete accuracy.
Using a hammer instrument, mild paralysis and signs of incoordination can be detected. Structural defects in the brain can be detected using MRI. CT (computed tomography) in this case is not very informative.
Long-term successful therapy of focal epilepsy (based on a clinical case)
O.V. ANDREEVA
, Ph.D.,
P.N.
VLASOV , Doctor of Medical Sciences, Professor,
Clinic of Headache and Autonomic Disorders of Academician Alexander Vein, Department of Nervous Diseases, Faculty of Medicine, Moscow State Medical and Dental University.
A.I. Evdokimova The article is devoted to the problem of choosing an effective antiepileptic drug. The most common manifestations of epilepsy are considered, a clinical case of successful treatment of cryptogenic focal epilepsy with complex partial seizures using a classic antiepileptic drug is described.
Recently, due to the expansion of the arsenal of antiepileptic drugs (AEDs) for the successful treatment of partial seizures, a completely new problem has arisen - the problem of drug selection, which is an important component of the effective treatment of epilepsy.
In this regard, recommendations for the treatment of epileptic syndromes are constantly updated and the place of classical AEDs is reviewed. The latest generation of drugs are obtained, as a rule, by targeted synthesis or improvement of an existing molecule, due to which the properties of AEDs are improved or new ones appear. The antiepileptic properties of drugs, which doctors have been successfully using for several decades, were discovered by accident. They did not undergo the now generally accepted 4 phase studies before the widespread clinical introduction of AEDs, however, they are all well studied (millions of patients were treated) and are characterized by effectiveness comparable to the “new” and “newest” AEDs [2]. According to PEP companies, the advantages of these drugs are better tolerability, linear pharmacokinetics, lack of enzyme induction and other properties. At the same time, any AED, both classic and “new,” has its own therapeutic niche and side properties [1].
This article discusses the most common manifestations of epilepsy, namely partial seizures, with an example of a clinical case of successful therapy with classical antiepileptic drugs.
Below we present a very indicative long-term (from 1995 to the present) clinical observation of the effective use of the drug Pagluferal for the relief of complex partial seizures of epilepsy. Pagluferal was developed based on the prescription of the famous Russian psychiatrist M.Ya. Sereysky, called the Sereysky mixture. The launch of industrial production of the drug was initiated due to the popularity of this prescription among neurologists and its wide distribution in industrial pharmacies.
The effectiveness of the antiepileptic drug Pagluferal is due to the properties of the components included in its composition.
Table 1 shows the three existing dosages of the drug.
| Table 1. Composition of the antiepileptic drug Pagluferal | |||
| Pagluferal®-1 | Pagluferal®-2 | Pagluferal®-3 | |
| Composition per tablet | |||
| Phenobarbital | 25 mg | 35 mg | 50 mg |
| Calcium gluconate | 250 mg | 250 mg | 250mg |
| Caffeine sodium benzoate | 7.5 mg | 7.5 mg | 10 mg |
| Bromized | 100 mg | 100 mg | 150 mg |
| Papaverine hydrochloride | 15 mg | 15 mg | 20 mg |
Phenobarbital (5-ethyl-5-phenylbarbituric acid) is a derivative of barbituric acid, has a strong anticonvulsant, hypnotic, antispasmodic and sedative effect.
The mechanism of action of phenobarbital is multiple and is primarily associated with increased GABAergic inhibition mediated by postsynaptic chloride current receptors—the opening of chloride channels. (An increase in the content of chlorine ions inside neurons entails hyperpolarization of the cell membrane and reduces its excitability.) It has been shown that at therapeutic concentrations it enhances GABAergic transmission and inhibits glutamatergic neurotransmission, especially mediated by glutamate alpha-amino-5-methylisoxazole-4-propionate (AMPA )-receptors. In high concentrations, it affects the flow of sodium ions and blocks the flow of calcium ions through cell membranes (L- and N-type channels) [1, 3, 5, 7, 10].
The effectiveness of phenobarbital, which is part of the drug Pagluferal, is described in the Italian study FIRST (1997), which studied the effect of treatment of the first and second generalized seizure on long-term prognosis. The study found that the majority of physicians preferred FB (47% after the first seizure and 39% after the second seizure) as initial therapy for their patients compared with carbamazepine, valproate, or phenytoin [11]. It is important to note that the drug is included in the list of essential medicines of the World Health Organization [13], as well as in the List of vital and essential medicines, approved by Decree of the Government of the Russian Federation dated December 7, 2011 No. 2199-r [4]. In the latest recommendations for prescribing first monotherapy according to the type of seizure or epileptic syndrome ILAE (2013), FB is classified as category “C” for focal and primary generalized seizures in both children and adults [8]. Pharmacokinetic studies indicate greater clinical effectiveness of FB when used in combination drugs (Gluferal, Pagluferal) [9].
Calcium gluconate. The calcium gluconate contained in the drug Pagluferal plays an important role, replenishing the deficiency of calcium ions necessary for the process of transmitting nerve impulses, activating the action of enzymes involved in the synthesis of neurotransmitters. Lack of calcium in the body leads to seizures.
Caffeine-sodium benzoate (caffeine) - being a psychostimulant, increases reflex excitability of the spinal cord, stimulates the respiratory and vasomotor centers, stimulates metabolic processes in organs and tissues. The main feature of the use of caffeine in the drug is the stimulation of metabolic processes in muscle tissue and the central nervous system, which is important in the treatment of epileptic seizures.
Papaverine hydrochloride is an antispasmodic agent with myotropic action that has a hypotensive effect. Reduces tone and relaxes smooth muscles of internal organs and blood vessels.
Bromisal - depressing the central nervous system, has a sedative and moderate hypnotic effect. Strengthens inhibition processes and promotes their concentration. Well tolerated.
Clinical case
Patient E.I. 43 years old. She first came to the clinic in 1995 with complaints of recurring (with a frequency of 3-4 times a month) complex partial seizures, during which consciousness is lost. The attack is manifested by phonation in the form of mooing, growling, lasting up to 20-30 s, without falling, any accompanying motor automatisms, without tongue biting and involuntary urination.
From the anamnesis of the disease and life it is known: heredity for epilepsy is not burdened, the mother at birth was 25 years old from her first pregnancy, which occurred in the 3rd trimester with an increase in blood pressure, for which outpatient therapy was carried out; the first physiological term birth, which proceeded without complications; early perinatal period - without features. At the age of 1.7 years (early 1970s), for the first time in my life, a single febrile seizure occurred; at 3 years, during daytime sleep, there was a generalized convulsive seizure, with vomiting and tongue biting. The patient was treated with Sereysky mixture powder, during which no seizures were recorded. At the age of 12 years, the Sereysky mixture was replaced with the drug Pagluferal-3, which the patient regularly took 1 tablet at night. Despite the fact that no attacks were recorded for more than 15 years, the drug was not discontinued. From the age of 17, complex partial seizures of the described nature began to bother me with a frequency of up to 1-2 times a year, with a subsequent increase (up to 3-4 times a month) by the time of treatment, she took Pagluferal-3 (50 mg/day).
The allergic history is unremarkable.
Somatically: chronic gastritis.
Mental development corresponds to age and education, there are no complaints about memory loss (the patient studies at the Institute of Economics, and additionally takes German language courses).
Neurological status: signs of parasympathetic vegetative dystonia are revealed in the form of mild acrohyperhidrosis, without cerebral and focal neurological symptoms.
EEG: upon repeated examinations - a hypersynchronous variant with the distribution of the alpha rhythm to the anterior leads, rare discharges of a sharp wave - a slow wave in the frontal-anterior temporal leads; in one of the EEGs there is asymmetry due to an increase in the amplitude of discharges: a sharp wave - a slow wave on the right.
Fundus: no pathology.
MRI: slight expansion of the subarachnoid spaces in the frontal areas. No focal structural changes in the brain substance were detected.
The patient was diagnosed with cryptogenic focal epilepsy with complex partial waking seizures of high frequency, without personality changes.
Due to relapse and increased frequency of attacks, it was decided to replace Pagluferal-3 with carbamazepine with controlled release of the active substance and gradually increasing the dose to 600 mg/day. After 3 weeks At a dose of carbamazepine 400 mg/day, the patient complained of periodic short-term episodes of dizziness and the appearance of a maculopapular rash on the anterior surface of the chest and on the anterior surface of the forearms. Carbamazepine was discontinued and replaced with sodium valproate up to 500 mg/day, the attacks stopped, but the patient began to be bothered by almost constant severe gastralgia, which did not go away for more than 1 month. and causing significant inconvenience to the patient, because she was studying at a university and these unpleasant sensations did not allow her to concentrate on studying. After discussion with the patient, it was decided to return to Pagluferal therapy with a gradual increase in the daily dose to 75, and subsequently to 100 mg/day. At a dose of Pagluferal-3 (100 mg - 2 tablets at night), attacks have not been recorded for more than 10 years. The patient categorically refused repeated proposals to try to stop the antiepileptic drug.
EEG (in dynamics): slight disorganization in the background recording, no regional epileptiform changes were detected.
Concentration of phenobarbital in blood plasma at a drug dose of 100 mg/day: C min (before taking the drug) = 16.3 mcg/ml. The treatment is well tolerated: the patient does not feel any signs of taking the drug. Clinical and biochemical blood tests without clinically significant abnormalities.
Ultrasound of the heart and abdominal organs: without pathology.
It is currently known that the patient is engaged in a family business, graduated from two universities, and has two healthy children.
The presented clinical case is very indicative in terms of the high effectiveness of the drug Pagluferal (the current drug remission lasts more than 25 years), excellent tolerability (the patient graduated from two universities, speaks two foreign languages well, has two healthy children) and long follow-up (more than 30 years). The absence of deviations in the somatic status, clinical and biochemical blood tests indicates the absence of a cumulative toxic effect of the drug. Twice attempts to switch the patient to carbamazepine and sodium valproate ended in failure due to side effects of therapy: in the first case, when carbamazepine was administered, a rash appeared, and skin manifestations are fraught with serious complications, including the development of exfoliative dermatitis; in the second case, the prescription of sodium valproate was accompanied by prolonged gastralgia, which significantly reduced the patient’s quality of life. The availability and high effectiveness of Pagluferal are important factors in choosing a drug.
Thus, using the example of the given successful clinical case, it is shown that the drug Pagluferal is highly effective and indispensable in clinical practice in the treatment of certain categories of patients. The active ingredients included in its composition have a synergistic effect, positively influencing metabolic processes in the central nervous system and muscle tissue.
At present, when new anticonvulsants are being actively developed and introduced into clinical practice, Pagluferal retains its position in the therapeutic arsenal, since it meets the requirement of breadth of action—target [1, 2] that an antiepileptic drug must have. This can be explained by the strengths of the drug - a wide spectrum of action, a long half-life (the ability to take the drug once or twice a day), high efficiency and good tolerability at a low cost of treatment.
Literature
1. Karlov V.A.
Strategy and tactics of epilepsy treatment today. Journal neurol and psychiatrist. them. S.S. Korsakova, 2004, 104, 8: 28-34. 2. Karlov V.A., Karlov V.A. Epilepsy in children and adults, women and men. M.: Medicine, 2010: 577-606. 3. Mashkovsky M.D. Medicines: a manual for doctors. 1993, 1: 36-38. 4. Order of the Government of the Russian Federation of December 7, 2011 No. 2199-r, Moscow. Russian newspaper. 2011, No. 5660. 5. Register of Medicines of Russia. 2007: 921-922 6. Arankumar G, Morris H. Epilepsy update: new medical and surgical treatment options. Cleveland Clin J Med 1998, 65:527-37. 7. Brodie MJ, Dichter MA. Antiepileptic drugs. N Engl J Med 1996, 334: 168-75. 8. Glauser T, Ben-Menachem E, Bourgeois B et al. Updated ILAE evidence review of antiepileptic drug efficacy and effectiveness as initial monotherapy for epileptic seizures and syndromes. Epilepsia, 2013, 54(3): 551–563. 9. Pharmacokinetic effectiveness of phenobarbital in children with epilepsy. Mater. 2nd Int. scientific-practical conf. "Unconventional methods of treatment in pediatrics." Dubna, 1993: 169. 10. Hauptmann A. Luminal bei Epilepsie. Munch Med Wochenschr. 1912, 59: 1907-9. 11. Kwan PM. Brodie Phenobarbital for the treatment of epilepsy in the 21st century: clinical review. Epilepsia, 2004, 45(9): 1141-1149. 12. Musicco M, Beghi E, Solari A et al. Treatment of first tonic-clonic seizure does not improve the prognosis of epilepsy. Neurology, 1997, 49: 991-998. 13. Vlasov PN, Petrukhin VA, Karlov VA et al. Antiepileptic Drug Therapy During Pregnancy in Moscow Region: Comparing of 1998 and 2013 years. Epilepsia, 2014, 55 (2): 130, doi: 10.1111/epi.12675. 14. WHO Model List of Essential Medicines, 16th list (pdf). WHO, 2009. Source: Medical Council, No. 17, 2014
What is the treatment for generalized epilepsy
Effective treatment of this type of epilepsy directly depends on the form of the disease, as well as the nature of the attacks. And if it does not always allow the patient to forget about his illness, ideally it should be aimed at maximizing the reduction in the frequency and severity of attacks.
Anticonvulsant therapy for generalized epilepsy is usually recommended to begin no earlier than the second attack and only if an accurate diagnosis has been established. It is usually started by prescribing a base drug specifically for this epiform (for example, valproate, etc.), starting with a dose that is approximately a quarter of the standard therapeutic dose. Over the next two to three weeks (with the indispensable condition of good tolerability and the absence of a therapeutic effect), the starting dose is increased by another half, further bringing it to the average therapeutic dose. Such monotherapy is usually quite effective in the case of idiopathic generalized epilepsy.
If no positive dynamics are observed as a result of treatment, or the condition is worsened by various side effects, the doctor may replace the drug with another one. Therapy can be considered successful when complete remission occurs (without attacks) within three years from the start of treatment, after which a dosage reduction is possible.
Generalized epilepsy today is not a death sentence for the patient, because a timely correct diagnosis and effective therapy allows the patient to significantly improve the quality of his life already in the first stages of treatment. Are you or your loved ones concerned about this disease? Experienced medical specialists are always ready to provide you with the necessary assistance and give you the opportunity to look into the future with confidence!