Damage to the abducens nerve of the eye is one of the ophthalmological pathologies that have much in common with neurological disorders. With this disease, the movements of the eyeball are distorted. It often happens that it does not move, especially when you need to look to the right. Let's tell you more about this disease and its treatment.
In this article
- Pathogenesis of the disease
- Causes of abducens neuropathy
- Symptoms of pathology
- Diagnosis of abducens neuropathy
- Treatment of abducens neuropathy
Pathogenesis of the disease
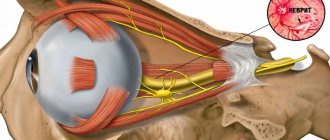
The abducens nerve of the eye is included in the category of fibers of the central nervous system. Its main function is to ensure the mobility of the visual organs. The nerve is responsible for the movements of the eyeballs, eyelids, dilation and constriction of the pupil. With neuropathy of the abducens nerve, a malfunction of the extraocular muscles occurs, and communication with the central nervous system of the body is disrupted. Thanks to the work of the abducens nerve, a person can look around without turning his head. Impaired functioning leads to ophthalmological pathologies, the most common of which is strabismus - strabismus.
Lesions of the abducens nerve cause the eyeball to not move evenly in different directions. Problems arise when the pupil moves in the opposite direction from the bridge of the nose. The mobility of the rectus lateral muscle of the eye is impaired. This leads to the development of a converging form of heterotropia, as the intrinsic muscle “pulls” the eyeball towards itself. People who are faced with this problem suffer from dizziness, diplopia - double image, and lose orientation in space.
Strabismus is not the only problem that a person with abducens neuropathy may face. This pathology is especially dangerous in childhood. It often causes the development of amblyopia. This condition is often called "lazy eye." The disease occurs due to the fact that the organs of vision do not participate in the visual process at the same time. Against the background of neuropathy, paresis often develops - peripheral paralysis. This disease is included in the neurological group. It is characterized by damage to the facial nerve, impaired facial expressions, and disruptions in the production of tear fluid.
Syndromes of cranial nerve damage in ophthalmology
Department of Microsurgery No. 1 Head. department: Voronovich T.F. Intern: Ivankova A.G.
Oculomotor nerve - n. oculomotorius (III pair) - is a mixed nerve, contains motor and parasympathetic fibers.
Motor fibers innervate the external muscles of the eye: superior rectus muscle (upward and inward movement of the eyeball); inferior rectus muscle (movement of the eyeball downward and inward); medial rectus muscle (inward movement of the eyeball); inferior oblique muscle (movement of the eyeball upward and outward); muscle that lifts the upper eyelid.
Parasympathetic fibers innervate the internal muscle of the eye - the muscle that constricts the pupil (m. sphincter pupillae), and are responsible for convergence (reduction to the center) of the ocular axes and accommodation.
Symptoms of defeat.
Ptosis (drooping of the eyelid) is caused by paralysis of the muscle that lifts the upper eyelid
Divergent strabismus is the installation of the eyeball outward and slightly downward due to the action of the unresisting lateral rectus (innervated by the VI pair of cranial nerves) and superior oblique (innervated by the IV pair of cranial nerves) muscles.
Diplopia (double vision). Double vision occurs as a result of deviation of the visual axis of one eye relative to the other; with monocular vision, it is usually caused by a change in the properties of the refractive media of the eye (cataracts, clouding of the lens).
Mydriasis (pupil dilation) with lack of pupillary response to light and accommodation; the pupil dilates as sympathetic innervation is maintained. The disappearance of the pupillary reflex to light occurs both on the affected side and on the opposite side, since the conjugacy of this reaction is interrupted. If at the same time light falls on the contralateral, unaffected eye, then the pupil reflex to light occurs on both sides.
Paralysis (paresis) of accommodation causes deterioration of vision at close distances.
Paralysis (paresis) of eye convergence is manifested by the inability to rotate the eyeballs inward.
Trochlear nerve - n. trochlearis (IV pair) - innervates the superior oblique muscle, which turns the eyeball outward and downward.
Symptoms of defeat. Paralysis of the muscle causes the affected eyeball to deviate upward and somewhat inward. This deviation is especially noticeable when the affected eye looks down and towards the healthy side, and is clearly manifested when the patient looks at his feet (when walking up the stairs).
Abducens nerve - n. abducens (VI pair) - innervates the lateral muscle of the eye, which rotates the eyeball outward.
Symptoms of defeat. Outward movement of the eyeball is impaired. This happens because the medial rectus muscle is left without an antagonist and the eyeball deviates towards the nose (convergent strabismus - strabismus convergens). In addition, double vision occurs, especially when looking towards the affected muscle.
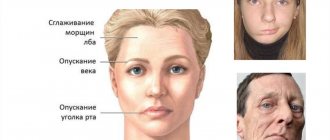
Bell's palsy (an idiopathic form of neuropathy of the facial nerve - innervates the facial muscles) - is manifested by paralysis of the facial muscles caused by damage to the facial nerve. When trying to close the eye, the eyelids on the affected side do not close, the eyeball remains uncovered, deviates upward and outward, and only the sclera fills the palpebral fissure (Bell's symptom).
Symptoms of defeat. Unilateral paresis of facial muscles, weakness.
The patient cannot raise an eyebrow on the affected side, frown, wrinkle his nose, close his eyes tightly, puff out his cheek, stretch out his lips, or whistle.
The muscle tone on the affected side is reduced, the cheek is “parous”; change in the width of the palpebral fissures; When teeth are bared, the oral fissure is pulled to the healthy side.
Due to paralysis of the orbicularis oculi muscles, the eyelids do not close (lagophthalmos - hare's eye).
Food gets stuck between the cheek and gum, tears can flow down the cheek, taste is lost on the front 2/3 of the tongue on the affected side, and hearing is worsened on the same side (hyperacusis). Sometimes, due to swelling surrounding the geniculate ganglion, the fibers that control the lacrimal gland are switched off, which leads to the cessation of tear production (dry eye syndrome), which is fraught with the occurrence of keratitis due to lagophthalmos.
Superior orbital fissure syndrome (also known as syndrome ) is a symptom complex that occurs as a result of damage (inflammation or compression) to the III (oculomotor), IV (trochlear), VI (abducens) pairs of cranial nerves, the optic nerve (1 branch of the trigeminal nerve) passing through the fissure .
The superior orbital fissure (fissura orbitalis superior) is formed by the body of the sphenoid bone and its wings, connecting the orbit with the middle cranial fossa.
Pass into the eye socket:
- three main branches of the optic nerve (ophthalmicus) - lacrimal, nasociliary and frontal nerves (nn. laerimalis, nasociliaris et frontalis) - determine the sensitivity of the eyeball;
- trochlear nerve (n.trochlearis). – determines the movement of the eyeball;
- abducens nerve (abducens) – determines the movement of the eyeball;
- oculomotor nerve (oculomolorius) - determines the movement of the eyeball and upper eyelid.
leaves the eye socket
- superior ophthalmic vein (ophthalmica superior). – determines the outflow of venous blood from the eyeball
a characteristic symptom complex develops :
- complete ophthalmoplegia, i.e. immobility of the eyeball;
- ptosis (drooping of the upper eyelid);
- mydriasis (pupil dilation);
- decreased tactile sensitivity of the cornea and eyelid skin;
- dilatation of retinal veins;
- neuroparalytic keratitis;
- slight exophthalmos.
However, “superior orbital fissure syndrome” may not be fully expressed when not all, but only individual nerve trunks passing through this fissure are damaged.
Palpebromandibular synkinesis of Marcus-Hun.
With this disease, the eyelids lift with each jaw movement while chewing food. Treatment is carried out in cases of severe ptosis and in the presence of significant eyelid movement. Discovered at birth.
Etiology: synkinesia caused by a congenital disorder of nerve connections between the fibers of the oculomotor nerve, innervating the muscle that lifts the upper eyelid, and the fibers of the trigeminal nerve, innervating the masticatory muscles.
As a rule, the first signs of the syndrome are detected when the baby is feeding. The eyelid on the affected side will move up and down when the jaw moves during feeding.
Appearance of palpebromandibular synkinesis of Marcus-Hun. Unilateral ptosis with decreased function of the muscle that lifts the upper eyelid. The latter rises on the affected side when the jaw moves. Raising the eyelid also results from a lateral displacement of the lower jaw in the direction opposite to the diseased eye.
Causes of abducens neuropathy
The disease rarely develops on its own. It is usually a consequence of other diseases. Most often, neuropathy of the abducens nerve occurs against the background of pathologies of the cardiovascular system, after traumatic brain injury and neurosurgical operations. Much less often, the disease is congenital. Cases of a hereditary form of pathology are not excluded, but they are not so common in medical practice. Doctors consider the main causes of the development of abducens nerve neuropathy
- endocrine disorders (diabetes mellitus, hypothyroidism, hyperthyroidism);
- neurological pathologies (osteochondrosis of the cervical spine, multiple sclerosis, stroke);
- complications of infectious diseases (encephalitis, diphtheria, meningitis);
- intoxication of the body (poisoning with ethyl alcohol, chemicals, alcohol);
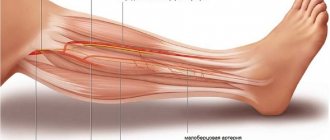
- chronic arterial pathologies (atherosclerosis, arteritis, phlebitis);
- cardiovascular diseases (varicose veins, arrhythmia, angina).
Doctors cannot always immediately determine what exactly caused the development of neuropathy of the abducens nerve of the eye. Diagnosis of this disease is often carried out by several specialists simultaneously, including: neurologists, cardiologists, endocrinologists, and traumatologists.
The disease is easier to detect in children than in adults. One of the causes of abducens neuropathy is hydrocephalus. This disease allows doctors to immediately carry out procedures that will allow them to diagnose the pathology.
Symptoms of pathology
The disorders that occur in the human body with this pathology affect various areas. The extent of optic nerve damage may also vary from patient to patient. Much depends on the immune system and the general condition of the body. Sometimes it happens that neuropathy affects the oculomotor nerve completely. In some cases, a partial disruption of its functions occurs. Therefore, it is very important for the doctor to analyze in detail the symptoms, which can be varied. The main signs of the disease include:
- drooping eyelid;
- pain in the eyes;
- immobility of the eyeball;
- decreased visual acuity;
- dilated pupils;
- diplopia.
A common consequence of abducens neuropathy is heterotropia. Typically, the patient develops convergent strabismus. More often this occurs in advanced forms of the pathology. Some people complain of high blood pressure, which is often due to problems with the brain. Headaches are another common symptom of this disease. It often happens that patients do not pay attention to the malaise and associate it with prolonged visual work.
What is abducens nerve palsy?
Paresis of the abducens nerve of the left eye and the right eye occurs with the same frequency. In most cases, the disease affects one side, rarely both. Paresis of the abducens nerve can be suspected by characteristic features: the patient has difficulty turning his eye towards the affected nerve. Paresis of the abducens nerve impairs the function of the rectus lateralis muscle, and the patient cannot fully avert the eye to the side. The patient experiences diplopia when looking straight ahead, which intensifies when the eye is turned towards the affected side. Other symptoms of abducens nerve palsy include:
- forced position of the head (impaired vision leads to an attempt to adapt to the changes that have arisen, which provokes the occurrence of involuntary positions);
- uneven gait (also associated with visual impairment);
- loss of orientation;
- dizziness.
Diagnosis of abducens neuropathy
The level of development of medical technologies does not cause problems with the diagnosis of pathology. Abducens neuropathy does not occur overnight. Its development occurs gradually. Diagnosis of the disease is usually carried out not only by an ophthalmologist, but also by a neurologist. First of all, the doctor interviews the patient, collects a detailed history, and inquires about the presence of other diseases.
The first thing the doctor must do is to determine the cause of the neuropathy. Usually, an ophthalmoscopy is performed by an ophthalmologist for this purpose. This procedure allows you to analyze in detail the condition of the fundus. Ophthalmoscopy is performed to diagnose retinal breaks, identify thinned areas of the eye nerve, and analyze the condition of the fundus vessels. To carry out the procedure, oculists use an ophthalmoscope or fundus lenses.
If neuropathy of the abducens ophthalmic nerve is suspected, doctors often prescribe angiography of the ocular vessels to patients. Using a fluorescent dye and a special camera, the doctor takes a series of pictures called angiograms. They depict the vessels of the retina. Angiography allows you to identify pathologies of the optic nerve, a predisposition to blockage of blood vessels, and inflammatory processes occurring in the tissues of the eyeball.
If the patient's condition is severe, doctors may recommend magnetic resonance imaging or computed tomography. This study allows you to obtain accurate data on the condition of the tissues and blood vessels of the eyeball. MRI and SCT diagnostics can be performed on adults and children. The list of contraindications to these procedures is quite small, which is why doctors often prescribe these studies to their patients.
Treatment of abducens neuropathy
Treatment of pathology largely depends on the causes of its occurrence. The basis of treatment for this disease is strengthening the muscles of the eyeball. This allows you to activate blood flow. For this purpose, ophthalmologists prescribe eye drops, including:
- "Taufon";
- "Irifrin";
- "Emoxipin";
- "Vita-Yodurol";
- "Visiomax".
If pain occurs, doctors prescribe the following medications:
- "Tegretol";
- "Finlepsin";
- "Amelotex";
- "Dexalgin";
- "Baklosan";
- "Rekoksa";
- "Timonil."
These drugs have both an analgesic and anti-inflammatory effect, relieve muscle spasms, and reduce the excitability of nerve fibers. Any medications must be prescribed by a doctor. He will select a maintenance daily dose and frequency of administration.
Physiotherapy procedures, such as electrophoresis, have a good effect. To carry it out, doctors use the drug Neuromidin. It improves and stimulates impulse conduction in the nervous system. Treatment of neuropathy often includes wearing occlusive dressings and training glasses. In pediatric therapy, ophthalmologists often use stereo images, which they offer patients to view on a computer monitor.
It is very important to keep the muscles of the eyeball toned. To do this, doctors recommend that patients perform eye exercises. There are special complexes that are aimed at treating abducens nerve neuropathy. Most of them include exercises such as closing your eyes, alternate winking, and moving your eyes to the right side.
Symptoms
- Muscle weakness;
- ptosis of the upper eyelid (usually symmetrical, bilateral);
- ophthalmoplegia.
Additional symptoms:
- hearing loss in which the structures of the inner ear, vestibulocochlear nerve or central parts of the auditory analyzer are affected (sensorineural hearing loss);
- loss of sensation in the limbs associated with damage to peripheral nerve fibers (neuropathy);
- loss of coordination of movements (ataxia);
- parkinsonism;
- depression.