02 Sep 2021 at 14:47 MRI of the head in Tushino 8829
According to current statistics, cerebral ischemia is diagnosed in every fourth resident of our country. As a rule, this phenomenon is age-related, however, its symptoms are increasingly observed among representatives of the younger generation (up to 40 - 45 years). In order to minimize the negative consequences of this dangerous disease, it is necessary to promptly contact specialists and listen to their professional recommendations.
General information about cerebral ischemia
Ischemia is a deterioration in the blood supply to organs and tissues due to impaired blood flow as a result of narrowing of vascular channels.
There are acute (stroke) and chronic forms of ischemia. About 90% of brain pathologies associated with blood vessels are related to chronic ischemia. The disease is common and has a high degree of disability. Pathology requires professional consultation and treatment. The brain requires more oxygen consumption than other organs. This is due to intense metabolism and accelerated metabolism. When blood supply deteriorates, less oxygen, red blood cells, and glucose enter the brain, its metabolism is disrupted, and hypoxia develops.
As a result, blood stasis occurs, a tendency to blood clots appears, and neurotoxins are produced. These processes provoke cell death. In the chronic form of the disease, the white matter is affected, and connections between the subcortex and frontal lobes are disrupted. Such changes, if left untreated, contribute to the development of dementia. In the chronic form of ischemia, an increase in intellectual-mnestic deficit is observed. At the initial stage, the patient experiences anxiety and depression. Further development of the disease leads to maladaptation in the social and everyday environment.
Treatment is aimed at improving blood circulation, metabolism, eliminating hypoxia, which helps reduce clinical manifestations and preserve brain tissue.
Mechanism of formation and pathogenesis
The basis of the disease is the weakening of normal nutrition of cerebral structures.
There are several options, but in all known cases there is a slowdown in the movement of liquid connective tissue through the vessels as a result of a mechanical obstruction.
And what was its cause: stenosis (narrowing) of the lumen, blockage with a cholesterol plaque, thrombus, malformation, aneurysm, other anomalies of anatomical development - needs to be clarified.
Without receiving nutrients and oxygen, tissues begin to die. Death or necrosis, however, does not reach a certain critical mass, at which the process becomes an avalanche-like, uncontrollable character - such an emergency condition is called a stroke.
Discirculatory encephalopathy, another name for chronic ischemia (abbreviated as CICI), is considered a precursor to acute necrosis of cerebral tissue.
Recovery is very difficult, but it is necessary to achieve lasting correction. The patient's life is at stake. Requires hospitalization in a neurological hospital.
Symptoms of cerebral ischemia
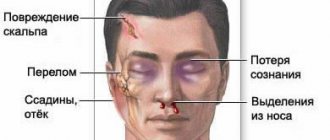
Symptoms of cerebral ischemia may occur periodically. There is a gradual deterioration in the patient's condition and progression of dementia.
Ischemia is manifested by the following symptoms:
- memory impairment;
- irritability;
- constant fatigue;
- sudden change in mood;
- inability to control emotions;
- slow thinking;
- loss of consciousness;
- failure of sleep mode;
- apathy;
- frequent headaches;
- blood pressure above or below normal;
- forgetfulness;
- inadequate reactions to events;
- marble skin tone;
- the appearance of new moles;
- involuntary muscle contraction.
In the last stage, it is difficult for the patient to provide self-care.
General signs
Common signs of a TIA include:
- severe tinnitus;
- flashes of light in the eyes;
- severe hiccups;
- nausea or vomiting;
- speech problems;
- pain in the back of the head;
- dizziness;
- severe headaches;
- coordination problems;
- convulsive state;
- blood pressure surges;
- transient amnesia.
Patients experience pale skin, absent-mindedness, and inability to concentrate. If the pathology is localized in the cervical region, then situational attacks cause the appearance of severe muscle weakness - the patient may fall, lose the ability to freely move the limbs, most often the victim is fully conscious. In severe cases, a person requires immediate emergency care.
Causes
The main cause of the development of pathology is atherosclerosis. Fat deposits accumulate on the walls of blood vessels, which leads to a narrowing of the lumen. In addition, the following factors provoke cerebral ischemia are identified:
- heredity;
- heart rhythm disturbances;
- squeezing of blood vessels;
- elevated blood sugar levels;
- diabetes;
- pathologies of the circulatory system;
- changes in blood pressure;
- vasculitis;
- heart pathologies, myocardial infarction;
- taking narcotic drugs;
- thrombosis;
- undergone operations;
- difficult or premature birth;
- abnormalities in the structure of blood vessels;
- pathologies of the central nervous system (CNS);
- severe toxicosis during pregnancy;
- renal ischemia;
- excess weight;
- influence of toxic gases;
- brain tumors (malignant and benign).
Bad habits - smoking, drinking alcohol - have a negative impact on the blood supply to organs. Age-related changes can also contribute to the development of the disease. Elderly people are more susceptible to cerebral ischemia.
Prevention
To prevent the development of transient ischemic attacks, you should follow the recommendations of specialists:
- take prescribed medications in accordance with the prescribed prescription;
- control blood pressure levels;
- monitor blood cholesterol levels;
- give up bad habits: alcohol and nicotine addiction;
- regularly take medications that prevent the formation of blood clots;
- be regularly checked by your doctor.
To prevent a transient ischemic attack from having consequences, you should lead an active and healthy lifestyle:
- eat on time and often;
- eliminate or reduce the consumption of fatty, smoked and salty foods;
- play sports: swimming, therapeutic exercises;
- spend more time outdoors.
If you adhere to all of the above, the prognosis for full recovery will be positive.
Yusupov Hospital is located near the center of Moscow. Patients are accepted here around the clock. You can make an appointment and get advice from specialists by calling the clinic.
Stages of development and types of cerebral ischemia
The disease develops in stages. There are several stages:
- First stage. It manifests itself as a deterioration in the quality of sleep, mood swings, and a feeling of constant fatigue and heaviness. Symptoms are nonspecific, which complicates the diagnosis of pathology at an early stage.
- Second stage. A disturbance in the functioning of the central nervous system occurs, the patient experiences dizziness, memory loss, coordination of movements, and gait are impaired. Mental work becomes impossible.
- Last stage. Significant neurological impairment is present. The disease manifests itself as loss of ability to work and the ability to care for oneself. Fainting occurs, the patient cannot independently describe his condition.
The form of cerebral ischemia is:
- Spicy.
It manifests itself as a sudden disruption of the blood supply to the brain. The patient experiences severe dizziness and muscle weakness. - Chronic.
Gradually progresses in the absence of therapy. Changes occur as a result of hypoxia. Symptoms appear periodically, and the arteries gradually wear out.
By localization and distribution they are divided:
- Focal.
Develops when a blood clot appears. Leads to the death of cells of the vascular canal. - Global.
Remission occurs when there is a drop in blood pressure or cardiac arrest.
Severity criteria
There are 3 degrees of severity of TIA. They indicate the positive or negative dynamics of the disease:
- mild degree - lasts approximately 10 minutes, focal symptoms that disappear without consequences;
- moderate degree - lasts from 10 minutes or more, the attack occurs without consequences for the patient’s health;
- severe - transient cerebral ischemic attack is prolonged, and neurological signs worsen.
According to ICD-10, transient ischemic attack has a standard classification:
- TIA in the VBB (vertebrobasilar area);
- TIA in the carotid region;
- TIAs are multiple or bilateral;
- transitional blindness syndrome;
- TGA (transient global amnesia);
- unspecified TIA.
The type and severity of local decrease in blood circulation in the head can only be determined by a qualified medical professional.
Diagnosis of ischemia
The first priority is to take a history and examine the patient. A hardware examination and collection of analyzes are also carried out:
- Ultrasound Dopplerography of the vessels of the cervical spine and head;
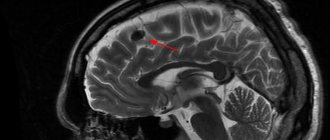
- MRI;
- magnetic resonance angiography;
- CT;
- ophthalmoscopy (to examine the fundus);
- ECG (to identify pathologies of the cardiovascular system);
- blood chemistry.
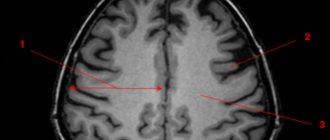
If cognitive impairment is detected, neuropsychological testing is necessary. Using Doppler ultrasound, it is possible to detect atherosclerotic plaques and differentiate them. In addition, the study helps to determine arterial stenosis, their changes, and cerebral vascular spasms. To study cerebral vessels, triplex scanning and color duplex scanning are also used. Using MRI, “silent” infarctions, enlarged ventricles of the brain, and changes causing cortical atrophy are determined.
Types of chronic insufficiency of blood supply to the brain
Brain with blood vessels ( bottom view
).
The branches of the main vessels of the brain at its base form a vicious circle called the circle of Willis.
Thanks to this, if one of the vessels is narrowed or blocked, the blood supply to the brain is fully or partially restored. (Image: Science and Life) There are three main types of cerebrovascular accidents.
In Binswanger's disease, due to thickening of the walls and narrowing of the lumen of small arteries, diffuse damage to the internal structures of the brain occurs - the so-called white matter. Multiple small lesions are areas of dead neurons. In patients, circadian (daily) pressure fluctuations are disrupted: at night it either drops too sharply, or, conversely, increases, although the pressure should decrease slightly at night. One of the main symptoms of the disease is sleep disturbance. The patient has trouble falling asleep or sleeps with frequent awakenings. Other typical signs are the slow progression of memory and intelligence impairments up to dementia (dementia); increasing gait disturbances, urination and defecation disorders. It is known that Binswanger's disease can occur even at a relatively young age - up to 35 years.
Another type of dyscirculatory encephalopathy - the so-called multi-infarct conditions - is characterized by multiple small infarctions in the brain (micro-strokes). This means that in a certain area of the brain, due to blockage of the vessel, necrosis of the nervous tissue occurs. This affects both the superficial (gray matter) and deep (white matter) structures of the brain.
The main reason for the development of multi-infarction conditions is the narrowing and hardening of intracerebral arteries during arterial hypertension. Another common cause is heart disease accompanied by atrial fibrillation. In such patients, blood clots form in the cavities of the heart - thrombi, which can clog the vessels supplying the brain with blood. Increased blood clotting also contributes to the formation of blood clots. Another cause of multi-infarction conditions is atherosclerotic damage to intracerebral arteries.
Discirculatory ecephalopathy also develops with damage to the main (carotid and vertebral) arteries, which are not located inside the brain, but provide blood flow to the brain. Lesions can have different natures and causes - thrombosis, stenosis, bends and kinks of various etiologies.
There are three stages of dyscirculatory encephalopathy. The duration of each of them may be different. Much depends on the degree of hypertension or atherosclerosis, lifestyle, habits, heredity, concomitant diseases, etc. At the initial stage of the disease, people often complain of headaches, dizziness, noise in the head, decreased memory (non-professional) and performance. Patients are absent-minded, irritable, tearful, and their mood is often depressed. They usually have difficulty switching from one activity to another.
Functional areas of the brain.
When the blood supply to certain areas of the brain is disrupted, patients experience corresponding neurological symptoms (image: Science and Life)
At the next stage of the disease, memory impairment, including professional memory, progresses. The range of interests narrows, rigidity of thinking (obsession on some problem), incompatibility appear, the intellect suffers, and a change in personality occurs. Such patients are characterized by daytime sleepiness and poor night sleep. Neurological symptoms intensify, movements slow down, their coordination is impaired, mild speech disturbances appear, staggering when walking, and performance is significantly reduced.
At the last stage of the disease, gross changes in brain tissue make neurological symptoms even more pronounced, and mental disorders intensify, including dementia (dementia). Patients completely lose their ability to work, stop recognizing loved ones, perform inappropriate actions, and may get lost when going for a walk.
Treatment
The main task in the treatment of cerebral ischemia is to normalize cerebral circulation. It is necessary to improve blood circulation and tissue metabolism. Drug therapy is aimed at the main links of pathogenesis. Patients are prescribed a course of drugs with different principles of action:
- neurometabolic;
- vasoactive;
- antiplatelet agents.
In addition to taking medications, it is necessary to eliminate risk factors such as arterial hypertension, atherosclerosis and others. Correction of nutrition and lifestyle is necessary. If blood pressure is high, antihypertensive medications are prescribed. For a complex effect on the central nervous system, nootropic drugs are prescribed. In the treatment of cerebral ischemia, antioxidant agents are of great importance. To improve reparative functions, drugs that have a metabolic effect are used.
In case of established cerebral ischemia, as a complex drug therapy, the doctor may prescribe: antihypertensive medications to control blood pressure (amlodipine, atenolol, anaprilin, enalapril, etc.). Attention! All medications prescribed by a doctor should be taken under control. There are contraindications.
Treatment of cerebral ischemia in the elderly
The treatment plan takes into account the existing pathologies of the elderly patient. The set of activities includes:
- Taking anti-sclerotic drugs. Recommended for hyperlipidemia not corrected by diet. Provides improvement of lipid metabolism, prevents neurodegenerative changes.
- Taking antihypertensive drugs. Antihypertensive drugs and blood pressure control are the main measures to prevent manifestations of ischemia. However, with a long history of high blood pressure, its normalization can aggravate chronic pathology and cause an increase in cognitive impairment of the “frontal” type.
- Use of antiplatelet agents. Necessary for severe atherosclerosis of the vessels of the head, for diagnosing disorders of the rheological properties of blood.
- Acetylcholinesterase inhibitors. They have an effective effect on cognitive disorders.
- Membrane protectors. Improves intellectual and mnestic functions. After taking a course of drugs, improvement in memory and communication is observed.
- Antidepressants. Prescribed for severe astheno-depressive disorders.
Complications
The lack of an effective treatment plan leads to a long-term lack of oxygen supply to the brain. This can provoke:
- stroke;
- necrotic changes in brain cells;
- epileptic seizures accompanied by fainting;
- inflammation of the veins of the lower extremities, the appearance of blood clots;
- atherosclerotic changes in blood vessels;
- paralysis.
In addition, sensitivity is impaired, and pain becomes chronic. The patient develops a depressive syndrome.