Modern society is susceptible to many mental pathologies, among which a separate group are nervous eating disorders, in particular bulimia.
It is noteworthy that men suffer from this disease much less frequently than representatives of the fair half of society, due to a number of reasons that will be discussed further. Bulimia literally means “bovine hunger” in Greek. Other names for this deviation are kinorexia, i.e. wolf hunger. Bulimia nervosa is an eating disorder characterized by regular, uncontrollable bouts of overeating.
The danger is not only the fact of lack of control over the amount of food eaten, but also the subsequent unhealthy concern about controlling body weight. Therefore, most bulimics resort to radical measures designed to neutralize (eliminate) the aftereffect of consumed foods on body weight.
Types of food pathology
Bulimia nervosa has different forms of manifestation, but has a common pattern of eating behavior: periods of uncontrolled food intake alternate with periods of active weight loss. Overeating (hyperphagia) can be:
- paroxysmal;
- permanent nature;
- at night.
A bulimic is unable to independently control outbreaks of irresistible hunger. When starting to eat, a person is unable to stop on his own until he clearly feels pain in the stomach and nausea.
People suffering from bulimia are more concerned about their figure than others. After another attack, they usually feel depressed due to guilt and remorse after what happened. Therefore, patients try in any way to avoid weight gain. For this reason, bulimia is divided into two types:
- classic nervous (cleansing ). She is characterized by a constant preoccupation with food and a desire to consume it in repeated episodes. Getting rid of hyperphagia involves taking drugs that have diuretic and laxative properties, forced gastric emptying (vomiting), and enema;
- compulsive _ Its peculiarity is that uncontrolled preoccupation with food is accompanied by careful monitoring of body weight. This type is characterized by other drastic measures for weight loss - exhausting mono-diets, additional physical activity, conscious fasting. At the same time, bulimics do not rid themselves of what they eat artificially. At a certain point, a person breaks down and begins to absorb food in even greater quantities.
Experts have identified so-called atypical kinorexia . This subtype has much in common with the classic form of eating disorder. However, an incomplete picture of the clinical manifestations required for a given mental pathology does not provide grounds for a doctor to determine a final diagnosis. The reason for this is an insufficient number of key symptoms of the disease. For example, after overeating and subsequent forced rejection of food, there is a complete absence of concern about being overweight and the desire to have ideal shapes.
Goosebumps
Diabetes
Iron deficiency
67792 09 December
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. The feeling of crawling on the skin: causes of occurrence, what diseases it occurs with, diagnosis and methods of treatment.
The human nervous system, with the help of reflex impulses, influences organs and tissues, helping the body adapt to changing environmental conditions. A reflex is understood as a response mediated by the nervous system to any stimulus (external or internal).
Throughout life, a person acquires some reflexes and loses others. However, there is a group of reflexes with which we are born and live. These include the so-called goosebumps, or pilomotor reflex.
The pilomotor reflex is an involuntary contraction of the smooth muscle structures at the base of the hair follicle, as a result of which the hairs rise to cover the surface of the skin.
Evolutionarily in animals, this reflex contributes to at least two things. Firstly, creating an additional air layer between the animal’s skin and the environment, which makes it possible to retain heat and protect against hypothermia. Secondly, with the help of the pilomotor reflex, the animal takes on a more intimidating appearance, which helps in intimidating enemies.
In humans, the pilomotor reflex has lost its former significance. However, goosebumps, or goosebumps as they are also called, have occurred to everyone more than once. The feeling of goose bumps on the skin is a type of paresthesia.
Paresthesia is understood as an unusual, pretentious feeling created by tactile receptors in the absence of their actual irritation. Other types of paresthesia include an unexplained feeling of tingling, burning, etc.
Types of goosebumps
The feeling of goosebumps on the skin can cover the entire surface of the body or occur only in a certain area, i.e. be localized. In some cases, it may be transitory, situationally determined and therefore not bring much discomfort. In others, paresthesias are long-lasting and persistent, then they can reduce the quality of life and become a cause for concern and see a doctor.
Possible causes of goosebumps
The occurrence of goosebumps is based on a reflex response of the nervous system. The reflex can be triggered both by stimulation of receptors - peripheral nerve endings (for example, cold receptors under the influence of cold air or cold water), and by stimulation of structures located in the central nervous system, for example in the brain.
This is typical for the appearance of goosebumps on the skin when a feeling of aesthetic or other pleasure or fear arises.
With inadequate stimulation of certain nervous structures, a person also develops piloerection (raising of hairs), which is characteristic of various diseases accompanied by damage to the nervous system. Peripheral nerves are most often affected, and, as a rule, the pathological process spreads from the smallest branches of nerves upward, capturing larger and larger nerve structures. Therefore, the appearance of paresthesia may be the first symptom of the disease.
What diseases can cause the feeling of crawling on the skin?
First of all, it is worth highlighting a group of diseases accompanied by primary damage to nerve fibers (neuropathy). These include:
- diabetic polyneuropathy
, which occurs with an uncontrolled persistent rise in blood glucose levels; - polyneuropathy
caused by a lack of vitamins and nutrients in the body, for example iron, vitamins B, C; - toxic polyneuropathy
, which occurs under the influence of toxins entering the body from the outside or being metabolic products; - alcoholic polyneuropathy
- damage to peripheral nerves by metabolic products of ethyl alcohol, is a special case of toxic neuropathy; - autoimmune diseases
, accompanied by nerve damage due to abnormal activation of immune system cells against the body's own tissues; - demyelinating diseases
, for example, multiple sclerosis, characterized by the destruction of nerve sheaths; - post-traumatic neuropathy
, which occurs due to mechanical effects on nerve fibers; - neuropathy associated with degenerative changes in the spine
, leading to compression of the nerves and disruption of their functioning; - hereditary degenerative diseases
of the nervous system, for example, Charcot-Marie-Tooth disease, one of the symptoms of which is various paresthesias.
The cause of the unpleasant sensation in the form of goosebumps crawling on the skin may be a pathological focus in the brain
(gliosis, tumors, etc.).
A range of mental illnesses
One of its symptoms is the appearance of paresthesia.
In patients with epilepsy
Paresthesias often appear as part of the “aura”, i.e. subjective sensations foreshadowing the imminent development of an epileptic attack.
Other reasons for the appearance of goosebumps include, for example, poor circulation
in one or another part of the body, leading to oxygen starvation of tissues.
Which doctors should you contact if you experience a crawling sensation?
Traditionally, the diagnosis and treatment of paresthesia, a type of which is the feeling of crawling on the skin, is dealt with, because this phenomenon is directly related to the functioning of the nervous system. However, if the cause of nerve damage is a somatic disease, i.e. disease of internal organs, then in addition to a neurologist, such a patient is seen by a vascular surgeon and other specialists, depending on the underlying disease.
Diagnosis and examinations for goosebumps
The causes of paresthesia are extremely diverse, therefore, when you come to your appointment, you need to be prepared for the fact that the doctor will be interested in how long ago the crawling sensation appeared, changes in diet, lifestyle, taking medications and supplements, past infectious diseases, travel to other countries, and etc. After a comprehensive clinical study, the most likely cause of the feeling of crawling on the skin will be determined, and depending on it, the patient will be referred for additional laboratory and instrumental studies.
- General blood test with leukocyte formula to exclude anemia, infectious and inflammatory processes, etc.
Manifestations and signs
The symptoms of kinorexia are determined by pathologically altered eating behavior and additional physiological indicators. The psychosomatics of such a deviation may not be expressed clearly enough, so it is important to pay attention to the auxiliary signs of the disease.
Bulimics are very similar to anorexics, but they are much more difficult to detect. While the latter can be easily identified by their unhealthy thinness, the weight of people with bulimia is close to normal. In addition, they are very ashamed of their addiction, so they try to hide it in various ways. For example, at social events they may simply not touch food, so as not to provoke a food breakdown.
The main signs of this eating disorder are:
- the first signal about the presence of a food pathology is excessive preoccupation with appearance, control of one’s weight;
- a sick person consumes an excessive amount of food at one time. These are mainly foods high in fat, starch, and sweets. A bulimic may leave in the middle of a meal to go to the toilet in order to get rid of what he has eaten. To muffle the sounds of vomiting, a person can specially create the noise of flowing water (turn on the tap, flush water in the drain tank);
- people who have eating pathologies prefer to eat alone and avoid public events;
- the patient's relatives may often notice the disappearance of large amounts of food. However, in order to hide his pathology, the bulimic tries to replace the missing products as quickly as possible even before their significant shortage is discovered;
- among pharmacological drugs such people may have a large number of laxatives;
- during a medical examination, the doctor notes an extreme degree of dehydration or disruption of the normal functioning of the gastrointestinal tract;
- bulimia leads to the destruction of teeth and gums, which can be noticed by the dentist;
- people who suffer from bulimia often complain of pain in the stomach, heartburn, swelling of the extremities, regular dizziness, ruptured capillaries on the face, swelling, women - failure of the cyclicity of menstruation
Additional physiological symptoms:
- haste when eating food, poor chewing;
- isolation in matters related to food;
- frequent attacks of irresistible hunger;
- dynamics of body weight in a positive or negative direction;
- inflammatory processes in the throat area, specific injuries on the fingers and hands that occur due to forced vomiting;
- disorders of the heart, kidneys, and liver.
Doctors state that bouts of overeating are episodic. Most often, the provocateur of such an attack of gluttony is psychosocial stress. Overeating ends in compensatory behavior: a person consciously provokes vomiting, uses special drugs that cleanse the body, significantly increases physical activity, and resorts to fasting.
A mandatory aspect for making a diagnosis of “bulimia nervosa,” in addition to uncontrolled consumption of food, is the patient’s concern about his body weight and his appearance. Most often, bulimics are dissatisfied with their weight and consider it excessive. Paradoxically, obesity or excess weight with bulimia is observed in rare cases.
Patients with kinorexia are more open when contacting a specialist. Doctors believe that the reason for this is the personal concern of such individuals about what is happening, as well as feelings of guilt and shame about this. A clinician who is sympathetic to the patient has the opportunity to obtain from him the most frank information that reflects what is really happening to the person.
In a healthy body healthy mind. Psychosomatics - what is it?
Be sick? Do you feel general weakness? Or maybe you are starting to have headaches? These and a number of other diverse manifestations may indicate real diseases well known to medicine. However, it also happens that none of the modern diagnostic methods helped to find the cause of the symptoms.
When physical ailments cannot be explained traditionally, but are the body’s response to the experience of negative emotions, psychosomatics can be suspected. What is a psychosomatic disorder - a fashionable diagnosis or a fact confirmed by science?
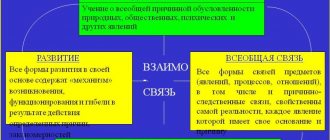
From antiquity to the present day
Interest in the close connection between the somatic (bodily) and mental (spiritual) spheres arose back in the time of Hippocrates. In the works of Avicenna one can find a substantiation of the hypothesis of the occurrence of illnesses due to the influence of negative emotions. The concept of “psychosomatics” is mentioned in the scientific literature of the early 19th century, and active interest among scientists in this group of diseases has been noted since the middle of the 20th century.
According to statistics, the number of cases of psychosomatic diseases increases every year, which makes their study relevant.
What is the cause of psychosomatic disorders ?
You can’t fall asleep before an exciting event, your face turns red during a public speech, your palms sweat during a conflict—this is a natural reaction of the body in crisis situations. But if the stress is strong, the events are psychologically traumatic, diseases of the internal organs may develop for no apparent objective reason.
In modern conditions, a person often has to restrain his emotions, especially negative ones (anger, aggression, irritation), displacing them into the subconscious. Suppressed emotions, in turn, cause changes in the functioning of internal organs, chronic stress weakens the immune system, and a person begins to get sick often.
What is the reason for this reaction of the organs? It's all about hormones, or rather some of them. The impact of stress on the body triggers the intense production of dopamine, adrenaline, norepinephrine, which accelerate physiological processes (breathing, heartbeat). Receiving a signal of stress, the brain instructs the adrenal glands to produce the hormone cortisol, which is responsible for the flow of blood to the muscles, providing a protective “flight or fight” function. The supply of sufficient oxygen to muscles and organs working in extreme conditions is achieved by increasing blood flow and increasing blood pressure as a result of vasospasm.
When a person is safe, an outburst of emotions must occur to normalize the activity of the cardiovascular and other body systems. But if such a discharge does not occur, then hormonal imbalance and vascular spasm persist, and this can lead, for example, to arterial hypertension.
How to recognize psychosomatics?
Often patients do not see the relationship between their own experiences and their physical condition, therefore, before identifying the psychosomatic nature of the illness, they undergo repeated consultations with various specialists, examinations, and sometimes receive treatment.
You can suspect psychosomatics when:
- the disease developed against the background of an acute or chronic traumatic situation;
- exacerbations of the disease depend on the influence of psychogenic factors;
- there are no other obvious reasons for the development of pathology - infection, intoxication, family history, etc.
Symptoms of psychosomatic disorders are varied. Patients may complain of:
- causeless headaches;
- dizziness;
- heaviness in the body and limbs;
- pain in the heart, muscles; heaviness in the back;
- numbness and tingling in different parts of the body;
- impotence, weakness, increased fatigue;
- dyspepsia (nausea, vomiting, stool disorders);
- chills, “hot flashes”;
- difficulty swallowing;
- suffocation and others.
Classification of psychosomatic disorders
Psychosomatic disorders occur in both adults and children.
An attempt to systematize them led to the identification of three main groups:
1. Conversion symptoms. A person feels real signs of neurological disorders, and according to the results of medical examinations, he is completely healthy. The patient may complain that he cannot see, cannot hear, or cannot move.
2. Functional syndromes. They are accompanied by functional disorders in the functioning of various organs and systems - cardiovascular, respiratory, digestive, endocrine, musculoskeletal, but their main prerequisite is stress.
3. Psychosomatosis. These are true psychosomatic diseases, accompanied by pathological changes in organs. Among them:
- bronchial asthma;
- ulcerative colitis;
- essential arterial hypertension (hypertension);
- neurodermatitis;
- rheumatoid arthritis;
- diabetes;
- duodenal ulcer and others.
How to help patients with psychosomatics
The effectiveness of treatment of psychosomatic disorders depends on identifying and eliminating the causes of their development. For this purpose, psychotherapeutic techniques are used. Medications for psychosomatic disorders are prescribed in the presence of concomitant emotional and behavioral problems. Sports, art therapy, hippotherapy, massage, and yoga have a positive effect on a person’s emotional health. The patient’s immediate environment can also help restore psychological balance.
If you want to avoid the development of psychosomatic disorders, learn to resist stress, build constructive interpersonal relationships, manage emotions and give them vent in a socially acceptable form.
Causes
The basis of the disease is a complex of causes that are biopsychosocial in nature. The consciousness of modern man is influenced by many factors: social, biological, cultural. By promoting certain ideals of beauty, the media programs the population to conform to them. The general situation is aggravated by public opinion and advertising campaigns.
This eating disorder, like any other mental disorder, has both biological and psychological background.
Biological factors in the occurrence of the disease include disruption of the normal functioning of the brain. These include organic damage in the area of the brain center responsible for human nutritional activity, as well as disruption of metabolic processes occurring in the body. Bulimia can also be triggered by traumatic brain injury, brain tumors, or hormonal imbalance that results in disruption of the normal functioning of the pituitary gland or hypothalamus.
The causes of psychological illness are more varied, but they are more difficult to detect. These include:
- emotional stress over a long period of time;
- neuroses of various types;
- low self-esteem;
- depressive states;
- increased anxiety or obsessive mental disorders;
- tendency to heredity.
Bulimia nervosa can develop against the background of excessive enthusiasm for all kinds of diets. Limiting oneself for a long time in favorite foods, after finishing such a “poor” diet, a person literally pounces on food.
Children and adolescents from wealthy families are most susceptible to kinorexia. The high demands that parents place on them lead to the child’s loss of personal self-esteem and its underestimation. Gradually, the still unformed personality begins to “eat up” the lack of warmth and affection from loved ones. At the same time, as already mentioned, an important role is played by the media, which promote standard beauty.
The child, realizing that he eats too much and can no longer refuse it, feverishly begins to look for ways to consume an incommensurate amount of food, but at the same time not lose weight.
It is characteristic that in those countries where excessive “boning” is not considered a standard of beauty, bulimia, as a mental pathology, is very rare.
Treatment
Treatment of PPPG should begin with explaining to the patient his diagnosis and the reasons for the formation of this condition.
This provides the confidence necessary to introduce treatment options such as physical therapy, medication, psychotherapy and various types of vestibular rehabilitation. Cognitive behavioral therapy (CBT) has proven itself well [4, 15]. Therapy is based on the collaboration between therapist and patient. The basis of treatment is the process of conceptualization - understanding the situation of a particular patient (personal beliefs and behavioral patterns). The therapist looks for different ways to achieve cognitive changes—modifications in the patient's system of thinking and behavior—that will help prompt lasting emotional and behavioral changes. The key to success is the active participation of the patient, who will not only work during the sessions, but also do homework. The patient and the therapist explore under what circumstances the problem manifests itself: that is, CBT teaches patients to identify, evaluate, and respond to their dysfunctional thoughts and beliefs. The goal is to make a list of moments and situations that cause anxiety/dizziness, etc. Then the therapist and patient outline a work program. It may include tasks that need to be completed in places or circumstances that cause anxiety/dizziness (riding an elevator, eating in a public place, etc.). These exercises allow you to reinforce new skills and gradually change behavior. A person learns to be less rigid and categorical, to see different facets of a problem situation [4]. Guided self-monitoring, which enables patients to recognize excessive postural control at the physical, emotional, and psychological levels, is the first step toward overcoming maladaptive cognitive-behavioral mechanisms. Desensitization exercises can be used to increase tolerance to existing imbalances. Identifying and assessing emotional and cognitive reactions to dizziness can help reduce fear, agitation, and catastrophic thoughts. Over time, patients can train the ability to respond to dizziness with calm.
Vestibular rehabilitation is an umbrella term for a range of physical interventions that aim to compensate and restore the systems that control balance. In PPPD and similar conditions, the main focus of the work is on the principle of desensitizing the balance control systems that operate on "high alert" through habituation exercises and relaxation techniques. A wide range of exercises can be used in vestibular rehabilitation, including both general ones, such as walking programs (gradually increasing the number of steps, speed and duration of walking), and more specific ones that increase dizziness when performing special head movements that must be performed relatively slowly [4]. ].
There are differences in the selection of vestibular rehabilitation methods for patients with PPPG compared to patients with structural vestibular disorders. Exercises with patients with PPPG should be started more carefully and the motor pattern should be expanded more slowly. However, patients should be instructed to begin exercise gradually and increase it slowly but steadily. An exercise program that is too aggressive can worsen symptoms, causing patients to “take a few steps back” before they can achieve any results. Monitoring the implementation of the rehabilitation program for the purpose of timely correction should be carried out by an experienced otoneurologist [4, 16].
To help reduce sensitivity to visual stimuli, there are special exercises, for example, the patient can spin a large striped umbrella in front of his eyes while sitting and then standing for 2 minutes. When treating functional gait disorder, exercises will include distraction techniques (eg, doing simple mental tasks while walking) as well as other types of walking (eg, backward walking, running, crawling) with a gradual return to normal walking. For all of the above, it is recommended to combine supervised treatment with daily unsupervised exercise at home [4, 13].
Selective serotonin reuptake inhibitors and selective serotonin-norepinephrine reuptake inhibitors are well established in the treatment of patients with PPPG. The effectiveness of therapy with drugs of these two classes has been confirmed by several prospective, open-label clinical trials. Randomized controlled trials have not yet been conducted. Dose selection should be done slowly. Effects are typically seen with doses in the lower half of the ranges recommended for treating depression. As with many functional disorders, patients may be particularly sensitive to side effects, leading to treatment interruption in one in five patients during the trial. Clinical response is usually observed after 8-12 weeks and, if a positive result is obtained, treatment should be continued for at least 1 year. Clinical experience with other classes of antidepressants has not been promising. Separately, it is worth noting the recommendation to avoid, if possible, the prescription of vestibular suppressors, such as antihistamines and benzodiazepines [4, 7, 12].
PPPG researchers suggest that long-term benefit likely depends on early treatment. The long course of the disease leads to a higher degree of maladaptation, more severe disability and more ingrained pathological attitudes towards the disease. Patients may suffer from PPPD for many years without being properly diagnosed, so practitioners should be familiar with functional vertigo and be aware of the treatment options described above. The presence of symptoms for a long time does not exclude good treatment results [4, 15].
Functional and psychiatric disorders causing vestibular symptoms (dizziness and/or unsteadiness) are more common than many known structural vestibular disorders. Patient education, vestibular rehabilitation, and medication significantly reduce morbidity and potentially maintain the patient in remission [7].
The authors declare no conflict of interest.
The authors declare no conflicts of interest.
Information about authors
Kunelskaya N.L.
- https://orcid.org/0000-0002-1001-2609; e-mail
Baibakova E.V.
- https://orcid.org/0000-0002-3430-6273; e-mail
Zaoeva Z.O.
- https://orcid.org/0000-0002-2501-0200; e-mail
How to quote:
Kunelskaya N.L., Baibakova E.V., Zaoeva Z.O. Psychogenic dizziness. Journal of Neurology and Psychiatry. S.S. Korsakov.
2019;119(10):89-93. https://doi.org/10.17116/jnevro201911910189
Corresponding author:
Zaoeva Zarina Olegovna — e-mail
Consequences
Many people consider bulimia nervosa to be a minor pathology that can be dealt with on their own without the help of a specialist. This misconception can lead to extremely undesirable results that will affect both psychological and physical levels.
The results of an advanced form of the disease may include the following phenomena:
- depression, a depressed state caused by feelings of shame and guilt for one’s behavior;
- there is a sharp change in life values and priorities;
- Communication with other people deteriorates.
The physical consequences manifest themselves as follows:
- a violation of the body's water balance, which occurs with regular use of laxatives or provoked vomiting. These actions also lead to a deficiency of microelements necessary for humans - potassium, calcium, sodium chlorine, etc. As a result, a person begins to feel weak, shortness of breath appears, an accelerated heartbeat (tachycardia), and kidney function is disrupted;
- the general hormonal background changes, natural metabolic processes are disrupted;
- high probability of gastritis, stomach ulcers;
- The mucous membrane of the mouth becomes inflamed, inflammation and ulcers appear in its cavity. Tooth enamel, which is regularly exposed to vomit with an aggressive, acidic environment, is gradually destroyed, which leads to tooth loss;
- the condition of the skin, hair, and nails gradually deteriorates;
- weakening of muscle and bone tissue, which occurs due to a gradual change in the biological rhythms of the body.
Psychosomatics of dizziness
It's hard to believe, but dizziness often occurs due to psychological problems.
They are often caused by: - information overload; - problems of choice; - fears; — dispersing one’s forces on several different things at once.
Let's look at each of these circumstances in more detail.
The fact that information overload , I think, is not a revelation to anyone. Probably, many of the readers can remember situations when, during “dense” preparation for exams or when mastering large amounts of new information, they felt slightly dizzy.
It’s not for nothing that people say: “there is so much new information that your head is spinning,” “your head is swelling from these scientific works,” etc.
I’ll tell you a secret that sometimes such “information” dizziness happened to me too - at those moments when, in preparation for writing another book, I had to “shovel through” a huge amount of scientific literature, for some unknown reason overloaded with complex pseudoscientific terms.
The situation gets even worse if information overload is combined with an attempt to keep a large amount of diverse information in your head.
Let's say, if you simultaneously begin to seriously study the Chinese language, musical notation, higher mathematics and, for example, biology, then after a week you will almost certainly encounter difficulties in further assimilation of new information.
Then you will feel how your level of criticality and clarity of thinking has decreased. Even later, you will most likely get dizzy (is this why many of our teenagers look “stupid” because in schools they are drilled into their heads with 5-10 diverse subjects at the same time, without taking into account the difference in the abilities of students?)
It’s another matter if you teach the same disciplines in cycles, as they do in senior years at institutes.
For example, devote 3 months exclusively to the Chinese language, then another 3 to musical notation, etc. Then a slight “fogginess” of the head will appear only in the first weeks of studying a new subject, since at this time the brain “automatically tunes” to a completely new one, unusual and incomprehensible information.
Disease history
Anton Egorovich headed a company selling computer components. Things were going well. But one day an excellent opportunity arose to expand the business and increase the company’s income by 5-6 times. However, this required covering related areas of trade and studying new regulations, customs and legal documents.
It is clear that assistants were required to carry out these large-scale tasks. It was beyond the power of one person to master the entire volume of completely diverse information. But Anton Yegorovich was a stubborn man, and also distrustful. He did not consider it necessary to initiate anyone into the affairs of the company, much less discuss with anyone issues related to its management.
Therefore, Anton Egorovich decided to do without assistants and, out of habit, shouldered all organizational matters on his shoulders. But, despite all his efforts, the man was never able to “digest” the huge amount of new information necessary to expand his business.
As he immersed himself in the topic, Anton Yegorovich’s head, in his own words, became more and more “woolly.”
The man began to stagger from side to side and became dizzy. At this stage, Anton Yegorovich realized that he could not do without medical help, and turned to me.
A course of manual therapy combined with the use of drugs that improve cerebral circulation helped bring the man back to his senses. But to prevent the situation from repeating itself, Anton Yegorovich needed to reduce his mental load.
Fortunately, he listened to my advice - to hire assistants or gradually “climb only one peak”, without being scattered on everything at once.
Having carefully weighed everything, Anton Yegorovich found a compromise solution: he involved his wife and his 20-year-old son in managing the company. Since then, Anton Egorovich has not contacted me about dizziness.
***
The method of overloading and dispersing consciousness is often used by gypsies during “gypsy hypnosis sessions.”
By chatting up the “client”, “loading” him with a non-stop flowing stream of verbal information, abruptly switching the “client’s” attention from one topic to another, the gypsies put the person being treated into a trance state, turn off his consciousness and deprive him of the opportunity to critically comprehend what is happening. After which they force the person to pay out all his money.
The same method of influencing the psyche is now also used in various sects. But if the gypsies, having defrauded a person, immediately disappear with the “loot,” then the leaders of religious sects keep their charges in a state of intoxication for months or even years.
In addition, sectarians skillfully manipulate the consciousness and subconscious of their clients, forcing them to memorize various mantras or obscure “prayer formulas.” And they finally deprive their students of critical thinking, manipulating feelings of fear and guilt: in most religious sects all doubts and dissent are prohibited. The leader of any sect will claim that only his religion or idea is true, and all others are wrong and sinful.
After such statements by the leader, any of his wards fall into a stupor and are afraid to even for a second doubt the words of their “shepherd”. This is probably why among the participants in such religious “get-togethers” there are many who are forced to consult doctors about dizziness and a feeling of lightheadedness or “stuffiness” in the head.
***
Problems of choice in situations where a person has to make a difficult choice between someone or something, but he cannot make this choice for a long time and therefore is in a “suspended” state, can also lead to dizziness.
Disease history
One of my married patients, Alina, fell in love with a work colleague. He reciprocated Alina's feelings. Their love was not momentary - it developed for quite a long time and gradually grew into a persistent need to be together not only during the day at work, but also at night.
Alina felt that she needed to leave her husband and establish a new life with her lover. However, as often happens, a number of circumstances (an established life, pity for her husband) and some doubts prevented her from taking a decisive step.
The hesitation “to leave - not to leave”, “to open up to my husband - not to open up” lasted about a year. And for about 8 months of this period, Alina suffered from dizziness and a feeling of “lightheadedness.”
Even manual therapy for the girl’s displaced upper cervical segment of the spine brought her relief for a maximum of 2-3 weeks. Then the dizziness returned.
Clarity and clarity of perception returned to Alina only when she thoroughly weighed everything and nevertheless made the final choice in favor of her beloved. Together with making a decision, the girl, in her words, “everything fell into place and became clearer in her head.” Almost immediately after this, her dizziness stopped.
***
Frankly speaking, I don’t know how fears affect the occurrence of dizziness. But, observing patients, I can definitely say that many of those who have been in a state of depression and fear for a long time also experience persistent dizziness.
Disease history
At the reception there is a girl Inna, 26 years old. Suffers from severe dizziness combined with attacks of nausea, fainting and a feeling of “lightheadedness”.
The girl fell ill about six months ago. It all started when cold air from the air conditioner blew through her neck at work in the summer. The next day, Inna’s neck muscles became inflamed, that is, classic cervical myositis developed.
Typically, cervical myositis is perfectly treated with anti-inflammatory drugs. They were assigned to their girl. Under the influence of the medications, the pain and inflammation clearly began to fade away and would have passed without a trace in a maximum of 2 weeks.
But to her misfortune, Inna, on the advice of doctors, decided to take a tomographic image of the cervical spine. This image revealed a protrusion (bulging) of the intervertebral disc measuring 3 mm.
In fact, bulging discs of such small sizes can be found in almost every healthy person. Especially at the time of exacerbation (with myositis) - this is simply a reaction of the body and intervertebral discs to a spasm of inflamed muscles.
However, some doctors, instead of calmly telling the patient about this well-known fact, on the contrary, try to intimidate him and “spin” him for money. Which is what happened in this particular case.
After looking at the tomographic images, the doctor advised Inna to undergo a neurosurgical operation “to remove a hernia of the spine” (as he called it) and offered his services as an intermediary between the girl and the paid neurosurgical department. “Otherwise,” the doctor said, “your arms and legs may fail.”
The doctor's statement left Inna in a state of shock. And although she was smart enough to refuse the operation, from that day on Inna was seized by terrible panic.
Even after her neck stopped hurting a long time ago, the girl kept thinking about her “hernia in the neck.” All day long, Inna searched for literature on spinal hernias. And the more books she read about this disease, the more she “twisted” herself and expected some kind of terrible outcome.
Then Inna began visiting doctors. Some were competent and decent, tried to calm Inna down and assured her that she could forget about such a tiny hernia. But Inna did not believe them. Others further intimidated the girl and siphoned money out of her for “exclusive treatment,” thereby increasing the panic.
Eventually, Inna’s panicked state transformed into illness: dizziness and a feeling of lightheadedness appeared. It was with these symptoms that Inna came to see me.
After talking with Inna for about 20 minutes, I more or less understood what the root of the problem was. But it also became clear to me that it was useless to convince the girl. With all her thoughts and emotions, she was already “hooked” on the disease. And then I decided to play along with Inna a little.
With a confident look, I told the girl that now we would treat her hernia (although I was 70% sure that by that time there was no trace left of the protrusion - after all, the inflammation and spasm of the neck muscles had long disappeared).
Having laid the patient on the couch, I performed several manipulations on her cervical spine, aimed primarily at eliminating dizziness. But he explained to the girl that “I’m pulling out the hernia with my hands.” Then he rubbed the usual warming ointment into his neck, but presented it as “an ointment for resolving a hernia.”
And although I was tormented by my conscience, since I usually do not resort to such tricks and always try to be honest with my patients, in this case the “strategy” was justified. Moreover, in the end this little trick bore fruit.
Immediately after my manipulations, Inna felt much better physically and, more importantly, much more confident psychologically.
In the second session, we consolidated the success with the help of manipulations aimed at the upper cervical segment of the spine and the elimination of dizziness. And after I was convinced that the patient’s neck was fine, I sent Inna to do a repeat tomography of the cervical spine.
Tomographic images confirmed what your humble servant already knew - there was no trace left of the protrusion (bulging) of the intervertebral disc.
For Inna, such a conclusion meant a miracle. But the main thing is that she immediately calmed down. And since the girl was already feeling well physically by that time, no further therapy was required.
* Chapter from the book “The Cause of Your Illness.” All names have been changed for ethical reasons.
* A very effective Brandt-Daroff for positional vertigo can be viewed here »»»
***
More interesting things on our Instagram *
Books by Dr. Evdokimenko in electronic form can be purchased at this link *
***
Attention! When copying or reprinting materials, be sure to indicate the source! All articles, news and book chapters are protected by copyright P.V. Evdokimenko©
Therapy for kinorexia
In order for a doctor to be able to make a final diagnosis of “bulimia nervosa,” the following signs must be present in a comprehensive manner:
- attacks of painful gluttony occur regularly, from 2 times a week for more than 3 months;
- the patient feels a strong craving for food, which can be compared to anxiety;
- fear of obesity, constant dissatisfaction with the state of one’s body;
- using all possible methods to help prevent excess weight.
Experts unanimously state that treatment for bulimia should have a comprehensive approach and be carried out exclusively with the participation of a doctor. The general treatment plan includes the following types of therapy:
- psychotherapy;
- psychocorrection;
- pharmacotherapy.
As a rule, treatment is carried out in an outpatient (home) setting with mandatory regular visits to the doctor. In more complex cases, when the pathology of eating behavior is complicated by concomitant nervous disorders, the doctor recommends inpatient treatment. This measure is especially necessary to relieve the patient’s acute condition.
In order to form a stable remission, in particular when using psychopharmacotherapy, it is recommended to conduct monthly examinations and consultations with a treating specialist.
Treatment for underweight
Treatment involves a set of measures. First of all, it is necessary to identify the cause of underweight and, if possible, eliminate it. Further, enhanced nutrition with a higher content of nutrients is recommended.
If this cannot be achieved with regular meals, special mixtures are prescribed. If it is impossible to take food by mouth, the option of parenteral nutrition or gastrostomy is considered. To prevent vitamin deficiencies, artificial vitamins are used. Sometimes enzyme preparations and hormonal treatment are effective in stimulating appetite.
In medical genetics, the “Microbiome” diagnostic panel is used to determine the genotype of the microflora that populates the integument of the gastrointestinal tract, genitourinary system and respiratory organs. The information obtained will allow us to make recommendations for normalizing the patient’s weight and nutrition.