The human brain not only works continuously throughout a person’s life, but also ages along with him. Under the influence of years, a person’s lifestyle and other factors, various destructive processes begin in him. Some of them can seriously affect life in general. For example, one of the unpleasant options is brain atrophy.
It represents changes leading to tissue depletion and loss of organ function. As a rule, when they talk about brain atrophy, they mean that the processes of necrosis of nerve cells have begun, and there is also a rupture of neural connections within groups that are connected either by chemical characteristics or functionally. Against the background of atrophy, the volume of brain tissue begins to decrease. Sometimes this situation is popularly called brain shrinkage.
Related article: Scientists have refuted this. Doesn't higher education affect the youth of the brain? As cells die, serious complications begin to appear. For example, cognitive abilities suffer, that is, a person begins to speak and think worse, he has problems with orientation in space, understanding and logic deteriorate, and abilities such as reasoning, calculation, and learning suffer. Movement problems may also develop. It is worth understanding that the death of neurons does not occur overnight—situations are not uncommon when several decades pass between the onset of the destructive process and the appearance of large damaged areas in the brain.
Destruction in the human brain can be focal, that is, when one fragment is affected, or it can become generalized, when degenerative processes are noted in all areas. Moreover, acute focal atrophy is usually regarded by specialists as a sign of illness or injury. There are also congenital manifestations, which, as a rule, give the first symptoms in childhood.
Brain atrophy: causes, symptoms, diagnosis
Atrophic changes in the cerebral cortex lead to the destruction of neural connections and a decrease in the activity of functional centers.
The condition leads to disruption of intracerebral metabolism, dementia, and the formation of a number of mental diseases (Alzheimer's, amyotrophic lateral sclerosis, dementia). Clinical symptoms depend on the type, stage, and degree of the disease. The multisystem form is accompanied by diffuse death of neurons and gradual loss of body functions.
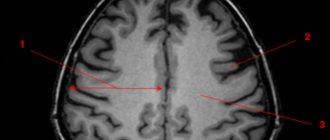
Brain atrophy on MRI
What is meant by neuronal death?
In general, atrophic changes in the brain are not considered a disease. Atrophy can appear not only as a result of the progression of the disease, but can itself become the cause of the development of the disease.
More precisely, brain atrophy is a pathological activity that smoothes the tissue of the cerebral cortex, reduces size, weight, and kills brain neural networks. Consequently, it affects the intellectual activity and other functions of a person.
This pathology is most common in people of old age. Everyone knows that people aged 70-80 years begin to suffer from dementia, partial memory loss and similar problems. But it cannot be said that this cannot happen to a young man or even a newborn child.
Such changes lead to changes in a person’s character and life. From here we will draw a conclusion. The death of brain neurons means:
- deterioration or complete loss of memory;
- speech disorders;
- motor impairment;
- decreased intelligence.
Causes of brain atrophy
After age 50, the risk of neurodegenerative conditions increases. Provoking factors increase the likelihood of the occurrence of a nosological form:
- Decreased kidney function (failure);
- Long-term increase in intracranial pressure (hydrocephalus);
- Frequent use of alcohol, drugs;
- Infectious damage to the cerebral cortex (retroviruses, poliomyelitis, encephalitis);
- Traumatic brain injury;
- Vascular diseases (thrombosis, atherosclerosis, aneurysm);
- Metabolic conditions;
- Mental illnesses - Alzheimer's, Itsenko-Cushing's syndrome, Parkinson's, Whipple, Gellervorden-Spatz.
Increases the likelihood of nosology - metabolic disorders, birth injuries, sexually transmitted infections, lack of B vitamins, folic acid.
The main causes of atrophy of the cerebral cortex
Scientific studies show a high probability of damage to cortical and subcortical structures in people 50-55 years old due to genetic predisposition. Cortical atrophy develops in patients suffering from hereditary Huntington's chorea.
Other reasons:
- Traumatic brain injuries accompanied by hematoma, neuronal death, and cyst formation;
- Chronic alcoholism, drug addiction, and the use of certain medications reduce the thickness of the cerebral hemispheres and subcortical sphere. Long-term alcohol intoxication disrupts intracellular metabolism and ensures the gradual death of neurons;
- Chronic cerebral (brain) ischemia is caused by vascular diseases (atherosclerosis, hypertension). Lack of oxygen contributes to irreversible tissue death;
- Congenital hydrocephalus in newborns leads to increased intracranial pressure and atrophy of the brain matter;
- More than seventy percent of cases of the disease in people over 55 years of age are due to neurodegenerative diseases - Pick, Lewy, Alzheimer's, Parkinson's. Nosologies form senile dementia.
Less common etiological factors of nosology are hypoxia of newborns, hydrocephalus, multiple congenital cysts in a child.
Causes of cerebral atrophy in newborns
The main etiological factor in reducing the thickness of the hemispheres of newborns is intrauterine hypoxia and problems during childbirth. Damage to the baby's head when passing through the birth canal provokes a traumatic brain injury and contributes to the appearance of hydrocephalus (dropsy).
Causes of atrophic cerebral changes in newborns:
- Damage to the bones of the skull;
- Increased amount of cerebrospinal fluid (hydrocephalus);
- Intrauterine infections (cytomegaly, herpes, meningitis).
There are no effective treatments for neonatal atrophy. Timely detection using MRI allows you to prescribe maintenance therapy and reduce the progression of the disease. Moderate changes are correlated with drug therapy. The child will be able to attend kindergarten and study in a special school.
Classification
Demyelinating disease of the nervous system is classified into different types, which are based on the destruction of the myelin sheath. In this regard, the pathology under consideration is divided accordingly into multiple sclerosis, Marburg disease, Devic disease, progressive multifocal leukoencephalopathy and Guillain-Barré syndrome.
Multiple sclerosis
Multiple sclerosis is characterized as a severe chronic and immunodegenerative disease of the central nervous system, prone to progression. In most cases, the disease occurs at a young age and almost always leads to disability. This demyelinating disease of the central nervous system is assigned code G35 according to ICD-10.
Currently, the causes of the development of multiple sclerosis are not fully understood. Most scientists are inclined to the multifactorial theory of the development of this disease, when genetic predisposition and external factors are combined. The latter include:
- infectious diseases;
- state of chronic intoxication;
- taking certain medications;
- change of place of residence with a sharp change in climate;
- lack of fiber and high-calorie diet.
The progression of multiple sclerosis is characterized by the development of the following symptoms:
- sensory disturbances (goosebumps, numbness, tingling, burning, itching);
- visual impairment (impaired color rendering, decreased visual acuity, blurred picture);
- trembling of the limbs or torso;
- headache;
- speech disorders and difficulty swallowing;
- muscle spasms;
- gait changes;
- cognitive impairment;
- heat intolerance;
- dizziness;
- chronic fatigue;
- libido disturbance;
- anxiety and depression;
- stool instability;
- insomnia;
- autonomic disorders.
Treatment of multiple sclerosis is carried out using methods such as:
- plasmapheresis;
- taking cytostatics;
- prescription of immunosuppressants;
- use of immunomodulators;
- taking beta interferons;
- hormonal therapy.
- symptomatic therapy with the prescription of antioxidants, nootropic drugs and vitamins.
During the period of remission, patients are prescribed sanatorium treatment, massage, and physical therapy. In this case, all thermal procedures should be excluded. To alleviate the symptoms of the disease, medications are prescribed: those that reduce muscle tone, eliminate tremors, normalize urination, stabilize the emotional background, and anticonvulsants.
Marburg disease
Hemorrhagic fever or Marburg disease is an acute infectious pathology caused by the Marburg virus. It enters the body through damaged skin and mucous membranes of the eyes and mouth.
The symptoms of the disease depend on the stage of the pathological process. The incubation period lasts from 2 to 16 days. The disease has an acute onset and is characterized by an increase in body temperature to high levels. Along with fever, chills may appear. Signs of intoxication increase, such as weakness, headache, pain in muscles and joints, intoxication and dehydration. 2-3 days after this, gastrointestinal dysfunction and hemorrhagic syndrome appear.
All symptoms intensify by the end of the first week. Bleeding from the nose, gastrointestinal tract, and genital tract may also be observed. By the beginning of week 2, all signs of intoxication reach their maximum. In this case, convulsions and loss of consciousness are possible. According to the blood test, specific changes occur: thrombocytopenia, poikilocytosis, anisocytosis, granularity of erythrocytes.
If a person is suspected of having Marburg disease, he is urgently hospitalized in the infectious diseases department and must be kept in an isolated box. The recovery period may take up to 21-28 days.
Devic's disease
Neuromyelitis optica or Devic's disease has a chronic pattern similar to multiple sclerosis. This is an autoimmune disease, the causes of which are still unclear. One of the reasons for its development is an increase in the permeability of the barrier between the meninges and the vessel.
Some autoimmune diseases can trigger the progression of Devic's disease:
- rheumatoid arthritis;
- systemic lupus erythematosus;
- Sjögren's syndrome;
- dermatomyositis;
- thrombocytopenic purpura.
The disease has specific symptoms. Clinical manifestations are caused by disruption of conductive impulses. In addition, the optic nerve and spinal cord tissue are affected. In most cases, the disease manifests itself as visual impairment:
- a veil before the eyes;
- pain in the eye sockets;
- blurred vision.
As the disease progresses and there is no adequate treatment, the patient runs the risk of completely losing his vision. In some cases, regression of symptoms with partial restoration of eye function is possible. Sometimes it happens that myelitis precedes neuritis.
Neuromyelitis optica has two course options: a progressive increase in symptoms with simultaneous damage to the central nervous system. In rare cases, a monophasic course of the disease occurs. It is characterized by steady progress and worsening symptoms. In this case, the risk of death is increased. With the right treatment, the pathological process slows down, but complete recovery is not guaranteed.
The second option, the most common, is characterized by an alternating change of remission and exacerbation and is designated by the concept of “recurrent course.” It is also accompanied by visual disturbances and spinal cord dysfunction. During the period of remission, a person feels healthy.
To identify Devic's disease, a set of measures is carried out. In addition to standard diagnostic procedures, lumbar puncture with cerebrospinal fluid analysis, ophthalmoscopy and MRI of the spine and brain are performed.
Progressive multifocal leukoencephalopathy
People with immune deficiency may experience progressive multifocal multifocal leukoencephalopathy. This is an infectious disease caused by the penetration of the JC virus, which belongs to the Polyomavirus family, into the body. A feature of the pathology is that asymmetric and multifocal brain damage occurs. The virus affects the membranes of nerve endings, which are made of myelin. Therefore, this disease belongs to the group of demyelinating pathologies.
Almost 85% of patients with this diagnosis are AIDS or HIV infected. The risk group includes patients with malignant tumors.
Main symptoms of the disease:
- mood swings;
- visual disturbances;
- paresthesia and paralysis;
- memory impairment.
Guillain-Barre syndrome
An acute inflammatory disease characterized by “demyelinating polyradiculoneuropathy.” It is based on autoimmune processes. The disease manifests itself as sensory disturbances, muscle weakness and pain. It is characterized by hypotension and disorder of tendon reflexes. Respiratory failure may also occur.
All patients with this diagnosis should be admitted to the intensive care unit. Since there is a risk of developing respiratory failure and a ventilator may be required, the department must have intensive care.
Subatrophy of the brain - the first stage of senile dementia
Before clinical symptoms appear, subatrophic changes develop. There are no external symptoms. The condition is accompanied by a partial decrease in the function of a segment of the hemispheres.
Morphological types of subatrophy:
- Frontal;
- Frontotemporal;
- Parieto-occipital.
The first type is characterized by a decrease in mental activity, loss of speech and motor functions.
Damage to the frontotemporal areas leads to a decrease in a person’s hearing ability, communication functions are lost (difficulty communicating with other people), and the functioning of the cardiovascular system is disrupted.
Subatrophy reduces the volume of gray and white matter. Disturbances in conduction and motor function and fine motor activity occur.
Features of cortical atrophy
The death of cortical cells begins in the frontal lobes, where the functional centers for controlling movement and speech are located. Gradually, atrophy spreads to surrounding structures. In older people, the pathology leads to senile dementia.
Diffuse cortical changes are accompanied by microcirculation disorders and progressive clinical symptoms. Fine motor skills of the upper limbs and coordination of movements are impaired. The pathological complex leads to Alzheimer's disease and senile dementia.
MRI of cortical atrophy shows a decrease in the size of the frontal lobes. If there are changes on both sides, the functioning of the internal organs controlled by the frontal lobes is disrupted.
Congenital cortical atrophy of newborns is localized on one side. Symptoms are mild. With the help of rehabilitation procedures, it is possible to socialize the child.
Symptoms
Demyelination always manifests itself as a neurological deficit. This sign indicates the beginning of the process of myelin destruction. The immune system is also involved. Brain tissue - spinal and brain - atrophies, and expansion of the ventricles is observed.
Manifestations of demyelination depend on the type of disease, causative factors and location of the lesion. Symptoms may be absent when the damage to the brain substance is minor, up to 20%. This is due to a compensatory function: healthy brain tissue performs the tasks of the affected areas. Neurological symptoms rarely appear - only when more than 50% of the nervous tissue is damaged.
The following are common signs of demyelinating brain diseases:
- paralysis;
- limited muscle mobility;
- tonic spasms of the limbs;
- dysfunction of the intestines and bladder;
- pseudobulbar syndrome (impaired pronunciation of sounds, difficulty swallowing, change in voice);
- impaired fine motor skills of the hands;
- skin numbness and tingling;
- visual dysfunction (decreased visual acuity, blurred images, fluctuations in the eyeballs, color distortions).
Neuropsychological disorders characteristic of the pathology in question are caused by memory deterioration and a decrease in mental activity, as well as changes in behavior and personal qualities. This is manifested by the development of neuroses, depression, dementia of organic origin, emotional swings, severe weakness and decreased performance.
Clinical symptoms of multiple system atrophy
Diffuse neurodegeneration is accompanied by problems in the reproductive and urinary areas. Necrosis of many parts of the brain is simultaneously accompanied by a variety of clinical symptoms:
- Muscle tremors in Parkinsonism;
- Impaired gait and mobility coordination;
- Loss of erection;
- Vegetative-vascular disorders.
Before the advent of magnetic resonance imaging, early diagnosis of the disease was problematic. Only nuclear magnetic resonance verifies a decrease in the thickness of the brain parenchyma.
Clinical symptoms of brain atrophy
The manifestations of pathology are largely determined by the causes and provoking factors. Most older people have dementia, frontal lobe syndrome, and internal multiple organ pathology.
How does frontal lobe syndrome manifest?
- Lack of appetite;
- Loss of memory, intellectual activity;
- Frequent emotional breakdowns;
- Lack of communication with surrounding people;
- Irritability;
- Lack of self-criticism.
Psychoorganic syndrome is accompanied by cerebroasthenic disorders, affective disorders, and amnesia.
The patient lacks an adequate assessment of surrounding events and self-criticism. Primitive thinking appears, a one-sided representation of the essence of the detail. Speech reserve decreases, paramnesia appears.
Concomitant affective disorders lead to depressive syndrome and inadequate mental state. Tearfulness, touchiness, irritability, unreasonable aggression are typical manifestations of pathology.
Alzheimer's disease
This is a progressive disease with increasing impairment of memory, thinking, intelligence, speech, praxis and recognition, ultimately leading to dementia.
Data on the prevalence of the disease are conflicting. According to some reports, it is 4–5% among people over 60 years of age. The main clinical forms of the disease are Alzheimer's disease itself (with onset mainly in presenile age) and senile dementia of the Alzheimer's type (with onset mainly in old age). An atypical form of the disease with a predominance of frontal lobe atrophy and Alzheimer's type dementia within Down syndrome are also distinguished. Here is a description of the main forms of the disease. 1. Alzheimer's disease . In approximately 80% of cases, it begins at the age of 45–65 years, less often - at the age of about 40 or after 65 years. The duration of the disease is on average 8–10 years, possibly protracted (more than 20 years) and catastrophic (from 2 to 4 years). There are three stages of the disease.
| | Read about diagnosing and treating Alzheimer's disease |
The initial stage includes the stage of “doubtful” dementia and the stage of “mild” dementia. The first stage is manifested by mild disturbances in memory, thinking, speech, praxis, and personality, which are noticeable mainly to the patients themselves and which they manage to hide or compensate for for some time. At the stage of mild dementia, impairments become more serious. Memory for current events decreases, chronological and spatial types of memory suffer.
Violations of various thinking operations are revealed. Disorders of speech, praxis, recognition, and psychopathic personality changes are detected. The severity of the disorders is such that patients can no longer cope independently with professional responsibilities and other types of social activities, such as shopping, paying bills, receiving guests, writing texts, etc.
Patients cope with self-care, although they need outside control and encouragement. Affective and delusional disorders are often observed at this stage. These are subdepressions, sometimes chronic and combined with anxiety, hysteriform and hypochondriacal manifestations; episodic or protracted delusional ideas of damage, theft, less often - ideas of relationship, persecution or jealousy. Some patients show increased exhaustion and headaches; the duration of the initial stage ranges from 4–8 to 15–20 years. At the same time, in some patients, memory impairments predominate, while in another, larger group, focal impairments (aphasia, etc.) prevail.
At the stage of moderate dementia, impairments in the cognitive sphere and higher cortical functions reach a degree where patients can no longer cope with professional and social responsibilities. They need help even with everyday life and self-care. Neurological disorders appear, such as muscle stiffness, akinesia, hyperkinesis, and seizures. A critical attitude towards the disease nevertheless remains. Along with deficient ones, productive disorders are sometimes observed: episodes of hallucinatory confusion, a state of psychomotor agitation, often not associated with a deterioration in the somatic condition. The aphato-apracto-agnostic syndrome (three A syndrome) characteristic of this stage is finally formed, the weakening of memory takes on the character of progressive amnesia. Confabulation and ecmnesia often do not occur.
The stage of severe dementia is characterized by the breakdown of memory, thinking and intelligence, as well as higher cortical functions. Patients need help even with basic self-care. Basically, only in Alzheimer's disease are such profound disturbances, to the point of insanity, observed, as well as fetal position, contractures, multiple violent motor phenomena, violent laughter and crying, and epileptic seizures. At the same time, there are pronounced somatic changes: weight loss, extreme decrepitness, bulimia, endocrine disorders.
2. Senile dementia of the Alzheimer's type. In approximately 80% of cases, it begins between the ages of 65 and 85 years. The duration of the disease ranges from 4 to 15 years or more. In the initial stage of the disease, significant memory impairment for current events develops, often with a revival of memories of the distant past. Thinking operations suffer, as well as intelligence (creativity, planning, forecasting, etc.). Personality changes are characteristic: egocentrism, narrowing of interests, emotional impoverishment, conflict, opposition and suggestibility. Moral decline and disinhibition of drives are also observed.
The suspicion inherent in patients later develops into a tendency to develop delusions. However, half of the patients experience psychotic episodes with low-level delusions. Subdepressive states are also observed, especially gloomy depression. In the second stage of the disease, memory impairment takes on the character of progressive amnesia. There may be scanty confabulations, as well as states of amnestic disorientation with a “shift of the situation into the past.” At the stage of moderate dementia, disorders of higher cortical functions also become clear. At the stage of severe dementia, a complete breakdown of mnestic-intellectual functions is observed, and serious neurological disorders are also detected.
The etiology of Alzheimer's disease has not been established. The role of genetic factors in the development of familial forms of the disease can apparently be considered proven. However, this role remains unclear in sporadic forms, which account for about 90% of all cases of the disease. Aging is essential.
The leading place in the treatment of patients is occupied by replacement therapy aimed at overcoming neurotransmitter deficiency. To compensate for cholinergic deficiency, tacrine, amiridine, exelon, memantine, Aricept, and reminyl may be recommended. To eliminate the deficiency of other neurotransmitter systems, other drugs are recommended, in particular Yumex and Citalopram. To increase the survival of neurons, nootropics are prescribed, especially Cerebrolysin, as well as vasoactive drugs, in particular sermion or nicergoline. Anti-inflammatory treatment such as indomethacin may be helpful. Therapy for psychotic disorders is carried out with the help of antidepressants, antipsychotics, and tranquilizers. The prognosis of the disease is unfavorable.
Types and classification of brain atrophy
According to the degree of danger, there are two types of atrophic changes in the brain:
- Physiological;
- Pathological.
The first type is natural. Throughout human development, the death of the umbilical arteries and ductus arteriosus (in newborns) initially accompanies it. After puberty, the tissue of the thymus gland is lost.
In old age, degenerative changes in the genital area occur. In elderly people, cortical destruction and involution of the frontal part appear. The condition is physiological.
Types of pathological atrophy:
- Dysfunctional – develops with a decrease in the functional activity of the brain;
- Compression – provoked by increased pressure on brain tissue (hydrocephalus, hematoma, copious accumulation of blood);
- Ischemic (dyscirculatory) occurs due to narrowing of the lumen of the arteries due to atherosclerosis, blood clots, and increased neurogenic activity. Generalized cerebral hypoxia is accompanied not only by mental dementia and sclerotic intracerebral changes;
- Neurotic (neurogenic) is formed due to a decrease in the flow of nerve impulses to the internal organ. The condition is formed due to gradual hemorrhages, the presence of intracerebral tumors, atrophy of the optic or trigeminal nerve. Occurs during chronic intoxication, exposure to physical factors, radiation therapy, long-term treatment with non-steroidal anti-inflammatory drugs;
- Dishormonal - occurs against the background of endocrine imbalance in the ovaries, testes, thyroid gland, mammary glands.
Morphological types of brain atrophy:
- Smooth – the surface of the brain is smoothed;
- lumpy - uneven distribution of areas of necrosis forms a special structure;
- Mixed.
Classification according to the extent of damage:
- Focal - only isolated areas of atrophic damage to the cerebral cortex can be traced;
- Diffuse - spreads over the entire surface of the parenchyma;
- Partial – necrosis of a limited part of the brain;
- Complete – atrophic changes in white and gray matter, degeneration of the trigeminal and optic nerves.
The nature of morphological changes in the brain is revealed by magnetic resonance scanning. Scanning should be done after the first clinical symptoms appear.
It is known that age-related changes manifest themselves in all organs and systems of the human body. In this case, the processes occurring during the aging period of the nervous system are of particular importance, which is the subject of this review, which summarizes the main facts in this area.
Aging of the central nervous system (CNS) is accompanied by atrophic processes expressed to varying degrees. The mass of the brain slowly but steadily decreases. The cerebral cortex, and subsequently the cerebellum, becomes thinner. According to V.V. Frolkis, the weight of the brain of a person aged 60 to 75 years decreases by 6%, and unevenly in different parts. The cerebral cortex decreases by 4%, the greatest changes (12-15%) occur in the frontal lobe. Gender differences in the degree of brain atrophy with aging have been noted. The weight of the brain of women is approximately 110-115 g less than that of men. Between 40 and 90 years, brain weight decreases in men by 2.85 g per year, and in women by 2.92 g [1]. The dura mater becomes thicker, becomes sclerotic, and fuses with the bones of the skull. The pia mater also noticeably thickens, the convolutions become thinner, the furrows widen and deepen. The arachnoid membrane progressively hyperplasias and sclerosis with age. According to H. Brody [2] and H. Chugani et al. [3], and brain weight decreases by 6-7% by the age of 80, the cerebellum loses up to 25% of Purkinje cells with age, the thalamic nuclei - up to 18%; changes most often occur in the prefrontal and medial temporal regions. According to E. Kensinger et al. [4], atrophy of both white and gray matter is observed in the prefrontal region. The decrease in gray matter volume is caused by a decrease in the number of neurons due to their degeneration. Axonal pathological changes and delayed neurotransmission are noted in the white matter. At the same time, R. Cabeza et al. [5] found that the decrease in interhemispheric asymmetry observed in older adults is most pronounced in the prefrontal cortex. It is still unclear whether bilateral alignment is a reflection of compensatory activation of one of the hemispheres or whether it is the result of pathological changes.
Another area of the brain where age-related changes are most pronounced is the hippocampus [6]. Considering the role of the hippocampus in memory formation, it becomes clear that functional and structural changes in this area during aging cause difficulties in remembering the context in which information was received [7, 8].
Thus, most human brain researchers point to predominant neuronal loss in the cortex, hippocampus, and cerebellum. In most subcortical formations, the cellular composition remains unchanged until old age [1]. At the same time, phylogenetically “newer” brain structures associated with cognitive function are more susceptible to age-related neuronal loss than phylogenetically “older” ones (brain stem).
During the aging process, the neurons themselves and their processes decrease in size, and lipofuscin and fat vacuoles accumulate in them. Myelin fibers become thinner. Electron microscopic examination reveals senile chromatolysis of neurons, their sclerotic changes and transformation into “shadow cells”. Not only signs of damage and degeneration of neurons (homogenization of the cytoplasm, displacement and pyknosis of nuclei, cytolysis, tigrolysis) of varying severity are revealed, but also signs of hypertrophy of intracellular structures, which indicates adaptive processes in conditions of age-related neuronal degeneration [9, 10]. Due to the death of neurons, one of the typical morphological signs of the aging brain occurs - cell rarefaction. The voids in areas of complete disappearance of neurons contain granular basophilic material and vacuoles, and they are also replaced by glial elements [11, 12].
With aging of the brain in the cerebral cortex, mainly in the frontal lobes, as well as in the hippocampus and subcortical ganglia, the number of glial elements increases and senile (senile) plaques are detected. They are located next to the vessels of the microvasculature of the cortex and represent accumulations of argyrophilic structureless material containing amyloid and surrounded by interweavings of thickened axons and macro- and microglial cells with little cytoplasm [13, 14].
With aging, synaptic density decreases. However, synapse loss does not occur equally in all parts of the central nervous system. Thus, in the frontal lobe, a decrease in the number of synapses with age has been reliably proven, while in the temporal lobe, age-related changes are not observed. Changes in the state of synapses are observed not only in the cortex, but also in subcortical structures. For example, age-related impairments in spatial memory have been attributed to decreased specificity, efficiency, and plasticity of synaptic transmission in the hippocampus. With aging, the ability to form new synapses decreases. Reduction of synaptic plasticity in old age can contribute to memory loss, deterioration of motor activity and the development of other disorders. At the same time, interneuron contacts in various areas of the central nervous system deteriorate, neurons seem to undergo deafferentation, and therefore their response to environmental signals, nervous and hormonal stimuli is disrupted, i.e., the synaptic mechanisms of brain activity are damaged [1].
As age increases, the state of the brain's neurotransmitter systems changes significantly. One of the most characteristic phenomena of aging is the degeneration of the dopaminergic system of the brain, which is directly related to the development of diseases such as parkinsonism in old age. Disturbances in the activity of the cholinergic neurotransmitter system of the brain play a major role in disorders of memory, perception and other cognitive processes that occur in Alzheimer's disease [15].
Aging is also accompanied by changes in the activity and content in human brain tissue of enzymes related to the synthesis and destruction of tyrosine hydroxylase, DOPA decarboxylase in the substantia nigra, caudate nucleus and putamen; choline acetylase and acetylcholinesterase - in the cortex, striatum, hippocampus and cerebellum, and therefore, the synthesis of acetylcholine in these structures is reduced. On the contrary, the content of monoamine oxidase increases in the midbrain. Disturbances in the exchange of neurotransmitters in dopaminergic neurons of the brain entail a decrease in it in the basal ganglia, caudate nucleus and putamen, which causes a disturbance in motor activity. A decrease in the content of serotonin and norepinephrine, a decrease in the content and rate of dopamine metabolism in the hypothalamus is associated with the development of depression in the elderly [16].
Age-related deterioration of blood supply to the brain through extra- and intracranial vessels is accompanied by changes in small vessels: sclerosis and hyalinosis of the walls, narrowing of the lumen. With aging, cerebral blood flow decreases, the functions of the blood-brain barrier are disrupted, the coupling between cerebral blood flow and glucose metabolism decreases due to the use of ketone bodies as an energy substrate, the levels of tissue respiration and oxidative phosphorylation decrease, as well as intracellular pH in the brain, which characterizes changes in cerebral energy exchange at all levels. Such changes are relatively weakly expressed during normal aging; nevertheless, they increase the sensitivity of the brain to oxidative stress and other damaging factors [17–19].
Age-related changes in the choroid plexus are manifested by sclerosis, the formation of cysts, calcification, and the appearance of psammotic bodies. Calcification processes in them progress with age: computed tomography reveals them in 1 out of 3 50-year-old patients, 3 out of 4 60-year-old patients, and 5 out of 6 80-year-old patients [11].
In the process of aging, there is a gradual decline in higher mental functions - perception, attention, memory, thinking. The speed of information processing, the amount of RAM, the ability to learn and remember new information decrease [20, 21].
Elderly people are characterized by emotional instability, decreased mental performance, increased threshold of unconditioned reflex reactions, difficulties in developing conditioned reflexes, as well as their slower decline compared to young people [22, 23].
As a person gets older, the process of perceiving new information and encoding it for subsequent storage requires more and more time, which is associated with reduced efficiency of neural transmission and sensory deficits that limit a person's ability to quickly and accurately perceive information presented for memorization [24]. , 25]. Older people also have a reduced ability to retrieve information stored in memory. This is partly due to the fact that it is more difficult for them to differentiate the necessary piece of information from the abundant stores of information and knowledge accumulated over many years of life. This process of delimitation (differentiation) can be especially difficult in the case when new information is similar in content to long-learned information. As a result, older adults perform much worse than younger adults on tests of free recall in which they are asked to recall learned information with minimal prompting. However, this difference is minimized when older subjects are given enough cues and cues to narrow the focus of their memory search for the desired information, or when they are asked to choose the correct answer from a small number of options [26–28].
It is believed that older people have better memory for events that happened in the distant past than for recent events. This is mainly due to the fact that long-standing events either have a special personal meaning for a person, or are so special in content that they could not be “erased” from memory by later events during life [29, 30]. Older people access these memories many times throughout their lives, which makes them more accessible for retrieval than everyday events, much of which are forgotten over time. It should be borne in mind that it is much more difficult to identify the errors of subjects in the reproduction of long-standing events compared to current events, when recall errors are obvious. Thus, short-term memory weakens significantly with age and is often impaired in older people. Age-related differences in long-term memory are much less pronounced and are thought to be a consequence of the use of ineffective encoding strategies or deficits in retrieval function [31, 32]. Semantic memory is not impaired at a later age. Progressive memory loss in some people is observed between 50 and 60 years of age, which is likely the result of degenerative changes in neurons, lipofuscin deposition, and the formation of senile plaques in brain tissue [27].
Speech is preserved relatively well during aging [3]. Older people aged 60–70 years use a more diverse range of grammatical forms in their speech compared to older age groups. Speech fluency in older people is no different from that of younger people. However, there are changes in the processes of understanding someone else's speech due to sensory deficits and a slowdown in the speed of information processing. In terms of written language, certain changes are also observed with age. Comprehension and perception slow down, making it more difficult for older people to grasp the meaning of what they read.
Another feature of neurodynamic disorders is a decrease in the ability to concentrate attention for a long time, so older people are often distracted by extraneous stimuli when performing certain tasks, this is especially pronounced when it is necessary to remember information against a background of “noise” [33]. They also have difficulty working with multiple sources of information. The latter may be associated with a decrease in the ability to switch attention, that is, with a certain intellectual rigidity.
Due to morphological changes in the brain, its bioelectrical activity also changes slowly and progressively. Starting from the age of 50 years, a restructuring of the spectrum of EEG rhythms is observed, expressed in a decrease in the amplitude and relative amount of the alpha rhythm and theta waves and an increase in the power of the beta rhythm [34, 35]. As for slow wave activity, the results obtained here are contradictory. According to some studies [36, 37], there is an increase in the power of slow rhythms and less often [38-40] no changes and a decrease in the power of slow rhythms were detected. A number of authors note that the dominant frequency after 60-70 years tends to decrease, and according to visual analysis of the EEG, theta and delta waves predominate. It is believed that the EEG slowdown is associated with ischemia, which leads to a progressive increase in the number of borderline normal and pathologically altered EEGs [41]. There is evidence that significant deviations in the background EEG in people over 70 years of age may be caused by dysfunctions in the normal regulation of sleep and wakefulness. By 90-100 years, the frequency of the dominant rhythm continues to decrease, the representation of slow activity increases, and its asymmetry appears in the temporal leads. Quantitative analysis shows a decrease in the power of the dominant rhythm and a decrease in its differences in different zones compared to 60-year-old healthy people. Theta rhythm is associated with memory and emotional regulation [42, 43]. Since memory impairment is one of the most significant manifestations of brain aging, this largely explains the decrease in the power of the theta rhythm [44, 45]. A decrease in alpha rhythm power was also noted. Alpha 1 rhythm is associated with attention and task difficulty, while alpha 2 is a neurophysiological correlate of complex semantic memory [46]. At the same time, the reactivity of the alpha rhythm to activating loads decreases, and the power of beta activity during functional loads increases [47]. N.V. Wolf and A.A. Glukhikh [34] found in their studies an increase in the power of high-frequency beta-2 and gamma rhythms in all leads compared to a young group, and these differences were most pronounced in the frontal parts of the hemispheres. In older people, there is also a decrease in the ability to assimilate imposed rhythms; the range of rhythm assimilation is narrowed and shifts towards low frequencies.
There is also a steady increase in the latency of the P300 wave of evoked potentials with age (P300 latency lengthens by 1.25 ms per year, and the amplitude decreases at a rate of 0.09 μV per year) and a decrease in the amplitude of visual evoked potentials. When studying auditory evoked potentials, an increase in the latency of N1 and P2 was noted, and their amplitudes change depending on the type of stimulus: the amplitude of N1 increases in response to a speech stimulus compared to a non-speech stimulus [48]. P2 amplitude, according to J. Lister et al. [49], less in older people compared to younger people due to a decrease in the activity of inhibition processes. However, K. Rufener et al. [48] in their study did not find any significant modulation of P2 in the elderly compared to the young. With age, the speed of propagation of excitation along the nerves decreases, and synaptic conduction slows down [50, 51].
According to V.F. Fokina et al. [52, 53], a qualitative analysis of the nature of changes during aging can be presented in relation to two parameters: the average level of constant potentials (ALP) and the interhemispheric difference in the temporal leads. At the same time, it is possible that the picture of cerebral energy exchange will change depending on biological age, social and psychological status, region of residence and other factors.
There is evidence that in the frontal areas, where age-related changes predominate - a decrease in blood flow and glucose hypometabolism, a secondary slight increase in SMR is recorded, reflecting a decrease in cerebral pH. In old age, there is a certain discrepancy between the dynamics of glucose metabolism and changes in ACR: glucose consumption decreases with aging, but the pH in the brain tissue increases, which may be due to a complex of reasons: a decrease in blood flow and energy metabolism, destructive processes [18].
Studies have been conducted on the distribution of SPP in elderly northerners, which have shown that characteristic changes during aging in them include: low values of SPP in the frontal leads, increased values in the central and parietal leads, as well as an increase in individual variability in indicators of interhemispheric differences. There was a smoothing of interhemispheric asymmetry in northern men in the frontal leads, and in northern women in the central leads, and right hemispheric dominance in the central leads in men [54].
Thus, during the aging process, the most significant changes are observed in the medial temporal and prefrontal areas of the brain, which in turn leads to a decrease in cognitive functions: a decrease in the speed of information processing, the amount of working memory, the ability to learn and remember new information. Morphological changes in the brain cause changes in its functional activity, which is reflected in the EEG, in the analysis of evoked potentials, as well as SCP.
The work was carried out within the framework of the project part of the state assignment in the field of scientific activity
of the Ministry of Education and Science of the Russian Federation for 2014-2016,
No. 2025 to the Northern (Arctic) Federal University named after. M.V. Lomonosov.
There is no conflict of interest.
Forms of multiple system atrophy
The danger of multiple lesions of brain structures is determined by a complex of pathological damage from the hemispheres, subcortical formations, cerebellum, spinal trunk, and white matter. Concomitant changes in the optic nerve lead to blindness, and in the trigeminal nerve – disruption of the innervation of the face.
Forms of multiple system atrophy:
- Olivopontocerebellar – damage to the cerebellum with impaired mobility;
- Striatonigral degeneration – muscle tremors with manifestations of Parkinsonism;
- Shy-Drager syndrome – vegetative-vascular dystonia, decreased blood pressure;
- Kugelberg-Welander amyotrophy is brain atrophy with muscle wasting and hyperplasia of connective tissue fibers.
Symptoms are determined by the predominant form of the lesion.
Demyelinating disease of the central nervous system
Demyelinating diseases of the brain and spinal cord are pathological processes that lead to the destruction of the myelin sheath of neurons and disruption of the transmission of impulses between nerve cells of the brain. It is believed that the etiology of diseases is based on the interaction of the body's hereditary predisposition and certain environmental factors. Impaired impulse transmission leads to a pathological state of the central nervous system.
What diseases are these?
There are the following types of demyelinating diseases:
- Multiple sclerosis is a demyelinating disease of the central nervous system. The demyelinating disease multiple sclerosis is the most common pathology. Multiple sclerosis is characterized by a variety of symptoms. The first symptoms appear at the age of 20-30 years, women are more often affected. Multiple sclerosis is diagnosed by the first signs, which were first described by psychiatrist Charcot - involuntary oscillatory eye movements, trembling, scanned speech. Patients also experience urinary retention or very frequent urination, absence of abdominal reflexes, pallor of the temporal halves of the optic discs;
- ADEM, or acute disseminated encephalomyelitis. It begins acutely and is accompanied by severe cerebral disorders and manifestations of infection. The disease often occurs after exposure to a bacterial or viral infection and may develop spontaneously;
- diffuse disseminated sclerosis. It is characterized by damage to the spinal cord and brain and manifests itself in the form of convulsive syndrome, apraxia, and mental disorders. Death occurs within a period of 3 to 6-7 years from the moment the disease is diagnosed;
- Devic's disease, or acute neuromyelitis optica. The disease begins as an acute process, is severe, and progresses, affecting the optic nerves, which causes complete or partial loss of vision. In most cases, death occurs;
- Balo's disease, or concentric sclerosis, periaxial concentric encephalitis. The onset of the disease is acute, accompanied by fever. The pathological process occurs with paralysis, visual disturbances, and epileptic seizures. The course of the disease is rapid - death occurs within a few months;
- leukodystrophies - this group contains diseases that are characterized by damage to the white matter of the brain. Leukodystrophies are hereditary diseases; as a result of a gene defect, the formation of the myelin sheath of the nerves is disrupted;
- Progressive multifocal leukoencephalopathy is characterized by decreased intelligence, epileptic seizures, the development of dementia and other disorders. The patient's life expectancy is no more than 1 year. The disease develops as a result of decreased immunity, activation of the JC virus (human polyomavirus 2), often found in patients with HIV infection, after bone marrow transplantation, in patients with malignant blood diseases (chronic lymphocytic leukemia, Hodgkin's disease);
- diffuse periaxial leukoencephalitis. A hereditary disease that most often affects boys. Causes visual, hearing, speech, and other disorders. Progresses quickly - life expectancy is just over a year;
- Osmotic demyelination syndrome is very rare and develops as a result of electrolyte imbalance and a number of other reasons. A rapid increase in sodium levels leads to the loss of water and various substances from brain cells, causing the destruction of the myelin sheaths of nerve cells in the brain. One of the posterior parts of the brain is affected - the Varoliev bridge, which is most sensitive to myelinolysis;
- myelopathy is a general term for lesions of the spinal cord, the causes of which are varied. This group includes: tabes dorsalis, Canavan disease, and other diseases. Canavan disease is a genetic, neurodegenerative autosomal recessive disease that affects children and causes damage to nerve cells in the brain. The disease is most often diagnosed in Ashkenazi Jews living in Eastern Europe. Tabes dorsalis (locomotor ataxia) is a late form of neurosyphilis. The disease is characterized by damage to the posterior columns of the spinal cord and spinal nerve roots. The disease has three stages of development with a gradual increase in symptoms of damage to nerve cells. Coordination when walking is impaired, the patient easily loses balance, bladder function is often disrupted, pain appears in the lower limb or lower abdomen, and visual acuity decreases. The most severe third stage is characterized by loss of sensitivity of muscles and joints, areflexia of the tendons of the legs, development of astereognosis, the patient cannot move;
- Guillain-Barré syndrome - occurs at any age, refers to a rare pathological condition that is characterized by damage to the peripheral nerves of the body by its own immune system. In severe cases, complete paralysis occurs. In most cases, patients recover completely with adequate treatment;
- neural amyotrophy of Charcot-Marie-Tooth. A chronic hereditary disease, which is characterized by progression, affects the peripheral nervous system. In most cases, the myelin sheath of nerve fibers is destroyed; there are forms of the disease in which pathology of the axial cylinders in the center of the nerve fiber is detected. As a result of damage to the peripheral nerves, tendon reflexes fade and atrophy of the muscles of the lower and then upper extremities occurs. The disease belongs to progressive chronic hereditary polyneuropathies. This group includes: Refsum's disease, Roussy-Lévy syndrome, Dejerine-Sotta hypertrophic neuropathy and other rare diseases.
Genetic diseases
When damage to nerve tissue occurs, the body responds by destroying myelin. Diseases that are accompanied by the destruction of myelin are divided into two groups - myelinoclastics and myelinopathy. Myelinoclasty is the destruction of the membrane under the influence of external factors.
Myelinopathy is a genetically determined destruction of myelin associated with a biochemical defect in the structure of the neuron membrane. At the same time, this distribution into groups is considered conditional - the first manifestations of myelinoclasty may indicate a person’s predisposition to the disease, and the first manifestations of myelinopathy may be associated with damage caused by external factors.
Multiple sclerosis is considered a disease of people with a genetic predisposition to the destruction of the membrane of neurons, metabolic disorders, a deficient immune system and the presence of a slow infection. Genetic demyelinating diseases include: neural amyotrophy of Charcot-Marie-Tooth, hypertrophic neuropathy of Dejerine-Sottas, diffuse periaxial leukoencephalitis, Canavan disease and many other diseases. Genetic demyelinating diseases are less common than autoimmune demyelinating diseases.
The main stages of atrophic brain changes
The disease has five degrees of progression. Based on clinical symptoms, it is possible to verify nosologies starting from the second or third stage.
Degrees of cortical atrophy:
- There are no clinical symptoms, but the pathology progresses rapidly;
- 2nd degree – characterized by a decrease in communication skills, lack of an adequate response to critical remarks, and an increase in the number of conflicts with other people;
- Lack of behavior control, causeless anger;
- Loss of adequate perception of the situation;
- Elimination of the psycho-emotional component of behavioral reactions.
Identifying any symptom requires additional study of the structure of the brain.
Principles of diagnosing atrophy
The initial stage involves taking an anamnesis, examination, and physical examination. The second stage is clinical and instrumental methods (ultrasound, CT, MRI of the brain, scintigraphy, PET/CT). Damage to the optic nerve is confirmed by ophthalmoscopy, tonometry, contrast CT or MRI angiography.
The best way to detect pathology of the soft tissues of the brain is MRI. The procedure must be performed several times (a month apart) to identify atrophy of varying depth and extent.
Magnetic resonance examination reveals the smallest local lesions and helps to correctly determine the degree of disease progression.
Diagnostics and differential diagnostics
Cerebral arthrosis is a disease for which diagnosis may require a detailed history of the patient.
The medical history is studied and the patient is interviewed about his living conditions and well-being.
But to make an accurate diagnosis, professionals send the patient to undergo the following diagnostic tests:
- CT head;
- diffuse optical tomography;
- MEG (measurement and visualization of magnetic fields);
- two-photon or single-photon emission tomography;
- MRI of the head.
And also in rare cases, differential diagnosis is possible. Having a patient's medical history, using a specially created computer program, a diagnosis can be made by exclusion. Based on the facts and symptoms that appear in the patient, the computer reduces the range of all possible diseases to one.
If it is impossible to carry out a complete diagnosis, a partial differential diagnosis can be made.