Alexandra Korostyshevskaya, Andrey Savelov, Irina Prikhodko, Yana Isaeva, Vasily Yarnykh “Science at First Hand” No. 3(88), 2020
Since childhood, we have heard that nerve cells do not recover. And although the question of the possibility of the formation of new neurons in the adult brain is still open, there is already evidence that the process of neurogenesis in humans continues into old age. Any disturbances in the development of nerve cells can lead to serious, sometimes irreversible pathologies. One of these disorders is defects in the protective insulating sheath (myelin) of nerve cell processes, which can form in a person even before birth. They are almost impossible to diagnose using traditional imaging methods.
About the authors
| Alexandra Mikhailovna Korostyshevskaya — Doctor of Medical Sciences, leading researcher at the laboratory of MRI technologies, head of the diagnostic department of the Institute “International Tomography Center” of the Siberian Branch of the Russian Academy of Sciences. Author and co-author of more than 70 scientific papers. |
| Andrey Alexandrovich Savelov — Candidate of Physical and Mathematical Sciences, senior researcher at the laboratory of MRI technologies at the Institute of International Tomography Center of the Siberian Branch of the Russian Academy of Sciences. Author and co-author of more than 90 scientific papers. |
| Irina Yurievna Prikhodko - software engineer at the laboratory of MRI technologies at the Institute of International Tomography Center of the Siberian Branch of the Russian Academy of Sciences. Author and co-author of 3 scientific papers. |
| Yana Olegovna Isaeva - student at the Institute of Medicine and Psychology named after. V. Zelman Novosibirsk State University. |
| Vasily Leonidovich Yarnykh — Candidate of Chemical Sciences, head of the laboratory of the Department of Radiology, professor at the University of Washington (Seattle, USA) and Tomsk State University. Author and co-author of more than 70 scientific papers, including 5 patents. |
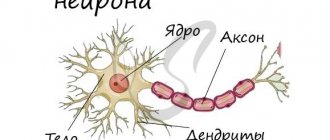
The average human brain contains about 100 billion neurons that receive, store, process and transmit information using electrical and chemical signals. Interaction between a neuron and other nerve cells and organs occurs through short ( dendrites)
) and long (
axon
) processes.
Each axon, like a wire, is covered with an insulating material - the myelin sheath.
, which provides a higher speed of nerve impulses and protects nerve fibers from damage. In addition, this shell has a supporting function, and also, according to the latest data, serves as a kind of “refueling station” for the axon, which needs a large amount of energy.
The axon is the main “cable” of a neuron, covered with a myelin sheath. It vaguely resembles a power line with a chain of insulators. The purpose of the shell, which is formed by special service cells (oligodendrocytes or Schwann cells), is to ensure the transmission of electrical impulses without loss and at maximum speed. © Servier Medical Art. Left
- axons of mouse sciatic nerves (
red
), wrapped in Schwann cells (
green
, nuclei -
blue
).
Photo by A. Alvarez-Prats and T. Balla. © Eunice Kennedy Shriver / National Institute of Child Health and Human Development
/ NIH
All damage to the myelin sheath or defects that occur during its formation lead to serious, sometimes incurable diseases. Among them, the most famous is multiple sclerosis.
is a chronic autoimmune disease that primarily affects young people.
Myelin is also destroyed during strokes
, which occur not only in adults (primarily, as is commonly believed, in older people), but also in children, including the unborn.
Intrauterine stroke most often occurs after the 28th week of pregnancy, and in children - a month after birth. Stroke in a fetus leads to the development of brain defects, and in children it can cause cerebral palsy
at an early age.
At the same time, today we judge the “quality” of myelination of the brain of a particular person only by indirect clinical symptoms or magnetic resonance imaging
(MRI), which can usually detect myelin defects at a late, often irreversible stage.
In the brain, the myelin sheath is created by oligodendrocytes, in the peripheral nervous system - by Schwann cells. Each oligodendrocyte forms several “legs” that repeatedly “wrap” around part of an axon ( bottom
).
As a result, one oligodendrocyte is connected to several neurons. © Servier Medical Art. At the top
- oligodedrocytes in culture (
red
, nuclei -
lilac
). © jakeyoung64
Not everyone knows that myelin is many layers of cell membrane, “wound” many times around the axon. Myelin is formed by flat outgrowths of “service” glial cells, in which there is practically no cytoplasm. The myelin sheath is not continuous, but discrete, with gaps (nodes of Ranvier). Therefore, the axon has faster saltatory conduction: the speed of signal transmission along fibers with and without myelin can differ hundreds of times. As for the molecular composition of the “insulator,” it, like all cell membranes, consists primarily of lipids and proteins.
Neural insulation defects
Fetal brain development is a complex process in which rapid changes in the morphology and microstructure of nervous tissue occur. In some areas of the brain, the process of myelin formation begins as early as 18–20 weeks of pregnancy, and continues until approximately the age of ten.
It is myelination disorders that often underlie delays in the physical and mental development of a child, and also cause the formation of a number of neurological and psychiatric pathologies. In addition to diseases such as stroke, delays in fetal brain development with impaired myelination are sometimes observed in multiple pregnancies. At the same time, desynchronization in the development of the brain of twins is quite difficult to assess “by eye”.
But how to identify myelin defects during fetal development? Currently, obstetricians and gynecologists use only biometric indicators (for example, brain size), but these are highly variable and do not provide a complete picture. In pediatrics, even in the presence of obvious functional abnormalities in the child’s brain activity, traditional MRI or neurosonography
(ultrasound examinations of the brain of newborns) often do not show structural abnormalities.
Therefore, the search for accurate quantitative criteria for assessing myelin formation during pregnancy is an urgent task, which also needs to be solved using non-invasive diagnostic methods that have already been tested in obstetrics. Specialists from the Novosibirsk International Tomography Center SB RAS proposed using for these purposes a new method of quantitative neuroimaging, already adapted for prenatal ( prenatal)
) research.
Neuroregeneration News
“Nerve cells don’t regenerate,” we’ve been told for decades, but now even schoolchildren know that this is not true. It is already known that in the brain of every adult there is at least one area where new nerve cells are constantly being born: this is the hippocampus area. It is responsible for processing memories and spatial orientation. By the way, this is why the anterior part of the hippocampus becomes more developed in taxi drivers.
And in the last few months, several scientific works have appeared, the results of which show that the body can independently restore even seemingly irretrievably lost nerve cells and connections.
Restore myelin in multiple sclerosis
Scientists at the University of California, San Francisco, have successfully conducted a series of experiments to restore lost myelin in mice with multiple sclerosis.
The basis of a disease such as multiple sclerosis is an “attack” of the membranes of neurons by one’s own immune cells. Because of this, the ability of neurons to transmit nerve impulses is lost. The myelin layer, which covers the long processes of neurons, in this case acts as “wires” along which the nerve impulse “runs.” Its destruction slows down the passage of the impulse by 5–10 times and leads to blindness, sensory impairment, paralysis, cognitive disorders and other neurological problems.
Experts used a mouse model of multiple sclerosis. In this case, healthy mice were injected with a protein contained in the myelin sheath, thus initiating an autoimmune response of the body, i.e., causing the immune system to “take up arms” against its own tissues.
Read also: Neuroscience
The new experiment built on previous research in which the same group of scientists found the beneficial effects of a histamine blocker called clemastine. The researchers combined clemastine with a protein that causes multiple sclerosis in mice and showed that these animals showed significantly fewer symptoms of the disease because the myelin sheath of the axons of neurons in the spinal cord and brain was restored.
Restore the optic nerve
The complexity of lesions of the visual apparatus inevitably entails the difficulty of restoring function. It is especially difficult when disease or injury affects the neurons connecting the retina to the optic nerves, or the optic nerves themselves.
A study recently published in Nature Neuroscience breaks new ground in optic nerve repair. A team of scientists from the University of Utah, Harvard University, Stanford University and the University of California at San Diego received interesting experimental results. They injured the optic nerves of mice by compressing them. The control group did not receive any therapy, as a result of which, after three weeks, retinal cell death was observed in these mice. Another group was shown alternating black-and-white images that stimulated the retina, which caused minor nerve regeneration.
The scientists also noted that injection into the eye of a viral vector carrying the gene responsible for the production of the cRheb1 protein (stimulates the so-called mammalian target of rapamycin (mTOR) signaling pathway, which regulates cell growth), increased the efficiency of restoration.
Careful analysis showed that the combination of these methods led to the regeneration of axons of retinal ganglion cells, and, most remarkably, this regeneration was very specific. The axons grew to the correct visual targets, as if returning to their usual places, and there was no dysfunction, as often happens when a nerve is restored.
This study clearly demonstrates how great the reserve for nerve tissue repair is, even in adults.
And just nerve cells
Of course, the worst thing that can happen to the brain is a stroke. Oxidative stress, caused either by cerebral hemorrhage or, conversely, ischemia, a lack of blood supply, leads to massive and rapid death of neurons. Unfortunately, no one has yet succeeded in restoring nerve cells in the cerebral cortex after a stroke.
However, it became possible to “fluff” the connections in the surviving neurons. Recent experiments conducted at the University of California, Los Angeles School of Medicine have shown how to make nerve cells recover more quickly after a stroke.
This became possible thanks to growth and differentiation factor 10 - GDF10 (growth and differentiation factor 10). Its introduction into nerve tissue promotes the growth of nerve connections, as a result of which the brain “comes to its senses” more quickly after a stroke. Healthy neurons spread new shoots (“octopuses”) deep into the tissue and re-establish lost contacts.
So, we see that scientists, in collaboration with doctors, are gradually searching for various ways through which it is possible to “spur” the restoration of the nerve cells themselves, or to obtain new neurons to replace the dead, or to force the nervous tissue itself to repair the damage. And we just have to wait until these studies move from laboratory experiments to clinical trials.
Alexey Paevsky
Photo istockphoto.com
On a regular tomograph
Any pathology of the fetal brain that doctors suspect during an ultrasound examination of a pregnant woman is usually an indication for an MRI; Similar studies have been carried out at the ITC SB RAS for more than ten years. MRI results can confirm, clarify, refute, or even change the preliminary diagnosis and, accordingly, pregnancy management tactics.
The fact is that the amount of myelin and the size of individual brain structures in the embryo are so small that any measurements are very complex and time-consuming. In addition, the fetus is constantly moving, which makes it very difficult to obtain high-quality images and reliable quantitative data. Therefore, we need technology that allows us to obtain images quickly and with high resolution even on small objects.
This is exactly what the method for fast mapping of the macromolecular proton fraction
(MPF) is a biophysical parameter that describes the proportion of protons in tissue macromolecules involved in the formation of the MRI signal, whereas the signal source is usually protons contained in water (Yarnykh, 2012; Yarnykh et al., 2015).
The macromolecular proton fraction (MPF) method is based on the magnetization transfer effect, when protons of free water “exchange” magnetization with protons of low-mobility macromolecules, such as proteins. The speed of this process affects the magnitude of the detected MRI signal and depends on the area of interaction between the macromolecular fraction and water
The method is based on a specialized procedure for mathematical processing of MRI images, which makes it possible to isolate signal components associated with the MPF of cell membranes. And in the brain of humans and animals, the main part of them is contained in myelin. MPF maps are reconstructed based on initial data, which can be obtained on almost any clinical tomograph.
To reconstruct the MPF maps, four source images obtained by various traditional MRI methods are used. The correctness of this approach was confirmed by the results of its testing on laboratory animals at Tomsk State University: in mice that were injected with a solution that causes myelin destruction, the results of MPF mapping coincided with the data of histological examination of tissues (Khodanovich et al., 2017).
Anatomy of myelin in the structure of a nerve
The main cell of the nervous system is the neuron.
The body of the neuron is called the soma. There is a core inside it. The body of the neuron is surrounded by short processes called dendrites. They are responsible for communication with other neurons. One long process, the axon, extends from the soma. It carries impulses from the neuron to other cells. Most often, at the end it connects with the dendrites of other nerve cells. The entire surface of the axon is covered by the myelin sheath, which is a process of the Schwann cell, devoid of cytoplasm. Essentially, it is several layers of cell membrane wrapped around the axon.
Schwann cells enveloping the axon are separated by nodes of Ranvier, which lack myelin.
The role of microglia in the destruction of myelin structure
Microglia are macrophages capable of phagocytosis and able to recognize various pathogenic particles - antigens. Thanks to membrane receptors, these glial cells produce enzymes - proteases, as well as cytokines, for example, interleukin 1. It is a mediator of the inflammatory process and immunity.
The myelin sheath, whose functions are to insulate the axial cylinder and improve the conduction of nerve impulses, can be damaged by interleukin. As a result of this, the nerve is “exposed” and the speed of excitation is sharply reduced.
Moreover, cytokines, by activating receptors, provoke excessive transport of calcium ions into the neuron body. Proteases and phospholipases begin to break down the organelles and processes of nerve cells, which leads to apoptosis - the death of this structure.
It is destroyed, breaking up into particles, which are devoured by macrophages. This phenomenon is called excitotoxicity. It causes degeneration of neurons and their endings, leading to diseases such as Alzheimer's disease and Parkinson's disease.
Principles of treatment of shell defects
Diseases associated with the destruction of the pulp membrane are very difficult to treat. Therapy is aimed mainly at relieving symptoms and stopping destruction processes. The earlier the disease is diagnosed, the greater the chances of stopping its progression.
Possibilities of myelin restoration
Thanks to timely treatment, the process of myelin restoration can be started. However, the new myelin sheath will not perform its functions as well. In addition, the disease may enter a chronic stage, and the symptoms will persist, only slightly smoothing out. But even minor remyelination can stop the course of the disease and partially restore lost functions.
Modern drugs aimed at myelin regeneration are more effective, but are very expensive.
Therapy
The following drugs and procedures are used to treat diseases caused by the destruction of the myelin sheath:
- beta interferons (stop the course of the disease, reduce the risk of relapses and disability);
- immunomodulators (affect the activity of the immune system);
- muscle relaxants (help restore motor functions);
- nootropics (restore conductive activity);
- anti-inflammatory (relieve the inflammatory process that caused the destruction of myelin);
- neuroprotectors (prevent damage to brain neurons);
- painkillers and anticonvulsants;
- vitamins and antidepressants;
- cerebrospinal fluid filtration (a procedure aimed at cleansing cerebrospinal fluid).
Functions
The main functions of the myelin sheath are:
- axon isolation;
- acceleration of impulse conduction;
- energy savings by maintaining ion flows;
- nerve fiber support;
- axon nutrition.
How pulses work
Nerve cells are isolated due to their membrane, but are still interconnected. The areas where cells touch are called synapses. It is where the axon of one cell and the soma or dendrite of another meet.
An electrical impulse can be transmitted within a single cell or from neuron to neuron. This is a complex electrochemical process that is based on the movement of ions through the membrane of the nerve cell.
In a calm state, only potassium ions enter the neuron, and sodium ions remain outside. At the moment of excitement they begin to change places. The axon is positively charged from within. Then sodium stops flowing through the membrane, but the outflow of potassium does not stop.
The change in voltage due to the movement of potassium and sodium ions is called the "action potential". It spreads slowly, but the myelin sheath that envelops the axon speeds up this process by preventing the outflow and influx of potassium and sodium ions from the axon body.
Passing through the node of Ranvier, the impulse jumps from one part of the axon to another, which allows it to move faster.
Once the action potential crosses the break in the myelin, the impulse stops and the resting state returns.
This method of energy transfer is characteristic of the central nervous system. As for the autonomic nervous system, it often contains axons covered with little or no myelin. There are no jumps between Schwann cells, and the impulse travels much more slowly.
Lecithin delivery
Lecithin, also known as phophatidylcholine, is a fatty substance made up of choline, fatty acids and other lipid molecules. Lecithin is important for nerve transmission and can serve as a source of choline for myelin production. Dietary sources of lecithin include egg yolks, soybeans, wheat germ and liver. Brussels sprouts, shrimp, peanut butter and chocolate also contain significant levels of lecithin. If you follow a vegetarian diet that excludes dairy or eggs, you risk becoming deficient in lecithin and choline. Taking a vegetarian lecithin supplement can help ensure you're getting enough of these important nutrients.