Make an appointment by phone: +7 (343) 355-56-57
+7
- About the disease
- Cost of services
- Sign up
- About the disease
- Prices
- Sign up
Electromyography (
electroneuromyography
, EMG, ENMG) is a diagnostic method for assessing the condition of the neuromuscular system. EMG is based on recording and qualitative-quantitative study of various types of electrical activity of muscles and peripheral nerves.
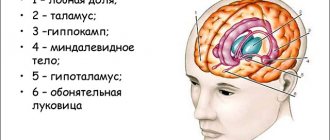
What is the "peripheral nervous system"?
But it is also impossible to imagine the functioning of our body without the peripheral nervous system. Electroneuromyography is used to examine it .
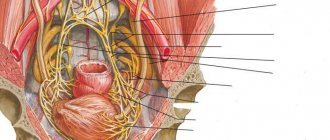
Peripheral nerves originate in the spinal cord and the nerve ganglia located next to it in the form of “roots”. According to their functions, peripheral nerves are divided into motor (responsible for the work of muscles), sensory (providing sensitivity) and autonomic (which are responsible for the work of internal organs).
The nerve roots, leaving the spinal cord, break up into paired plexuses (cervical, brachial, lumbar and sacral), which, in turn, break up into the peripheral nerves themselves. Sensory nerves receive information from receptors (for each “type” of sensations - pain, temperature, touch, pressure, etc. - there are different types of receptors), motor neurons are connected to muscle fibers through neuromuscular synapses. With the help of special synapses, autonomic nerves also contact the cells of internal organs.
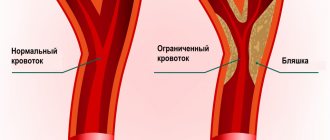
Very simply, a typical peripheral nerve can be thought of as an electrical cable consisting of many small wires united by a single sheath. “Electricity”, that is, the nerve impulse, is transmitted in the nerve through the membrane, and not through the inside of the “wires”. The “wire” is called an axon and is a process of the nerve cell (neuron) itself, located in the spinal cord (the length of the axon innervating the foot muscle can reach a meter or more). The “sheath” of the wire is the substance myelin, which ensures the transmission of nerve impulses along the axon.
Electroneuromyography (ENMG)
- Cost: 8,400 rub.
- Duration: 30-40 minutes
- Hospitalization: outpatient
More details
I deliberately focused on describing the structure of the peripheral nervous system so that ENMG (electroneuromyography) would not seem to you in the future to be some strange, mysterious, “shamanic” method. So, in our body there is an intricacy of cables that conduct current; cables consist of wires that have a sheath. Failure of this system is possible at any level (from a cell in the spinal cord to the neuromuscular synapse) and can occur due to damage to the wire itself and its sheath. The purpose of ENMG is to find the location of the damage and determine its nature.
Of course, electroneuromyography is not a magical and universal diagnostic method (just as none of the other more widely known techniques, such as MRI, is). Not all nerves and muscles can be studied, and not all areas can be tested. But with a competent approach on the part of the doctor prescribing or performing ENMG, this method can provide a lot of useful information.
So what is stimulation ENMG?
The standard method for studying motor and sensory fibers of peripheral nerves looks simple on the surface. Electrodes are applied over the surface of the muscle or on the area of skin innervated by the nerve being studied (most often they look like a small patch or sticker), and the electrodes are connected to equipment (electroneuromyograph). In areas where the nerve is not very deep, using a special stimulator (vaguely reminiscent of the plug of any electrical appliance), the nerve is irritated by electric current discharges. The current is weak and absolutely safe, although the sensations may be unpleasant. As a result of electrical stimulation, a muscle contracts or a response occurs in the skin (in the case of studying sensory fibers). This response, or muscle contraction, is recorded by electrode stickers. The data obtained is analyzed by a doctor.
Decrement test
Examination and analysis of the condition of most large nerves of the extremities usually does not cause difficulties. Assessing the condition of the plexuses and nerve roots is more complex, because, as discussed above, they are formed from many peripheral nerves, and it becomes necessary to examine almost each of them.
To diagnose diseases of the neuromuscular synapse, the method of rhythmic stimulation or “ decrement test ” is used. When performing a decrement test, the nerve is stimulated several times (usually five) at a high frequency of stimuli (about 1 per second), the muscle is forced to contract five times in a row in five seconds. If the synapse functions normally, then all five times the impulse from the nerve causes the muscle to contract with the same force. If the synapse is damaged, the muscle contracts weaker each time. Of course, this is a very simplified explanation of the essence of rhythmic stimulation ( decrement test ).
How useful is NCS/EMG?
NCS/EMG is an additional option for physical examination and often adds information to the clinical assessment: it helps to determine the nature and extent of the pathological process, assess its activity and dynamics, and adjust treatment. A test is not always required for every nerve or muscle disorder. The need for a test, as well as a referral for a test, is issued by the attending physician. The referral must indicate the level of examination, preliminary diagnosis and other information necessary for the correct execution of the examination.
Needle ENMG
To study muscles, and this is necessary if there is a suspected pathology of the motor neuron of the spinal cord, for muscle diseases, or to determine the degree of muscle damage in neurological pathology, needle electromyography . A thin needle-electrode is inserted into the muscle being studied (reminiscent of an intramuscular injection). The electrical activity of the muscle is recorded at rest and under moderate tension. Needle ENMG is a more complex method from the point of view of interpretation and often takes more time and requires more qualifications from the doctor.
Contraindications
There are no absolute contraindications.
However, if you have a built-in pacemaker or an implantable cardioverter-defibrillator, you must provide a referral with permission from the attending physician (cardiologist-arrhythmologist or cardiac surgeon) before the procedure. Pregnant women must provide permission for the procedure from a gynecologist.
At the New Hospital, you can consult a cardiologist-arrhythmologist or a cardiac surgeon, and if necessary, the device will be configured for safe electromyography.
EMG does not exert a radiation load on the body, so the procedure is used 2-3 months after the start of therapy.
The data received from the study is deciphered by the doctor in the diagnostic room and handed over to you. The final diagnosis is made by the attending physician.
You can make an appointment for a consultation and diagnostics by phone. (343) 355-56-57
Electroneuromyography capabilities
So, when used correctly, electroneuromyography allows:
- diagnose nerve and muscle diseases in the early stages, when no abnormalities are yet observed during clinical examination;
- establish the level of nerve damage;
- conduct a differential diagnosis between peripheral nerve damage and radiculopathy (damage to the nerve root), and plexopathy (damage to the plexus);
- assess the severity of damage to the peripheral nervous system and muscles;
- evaluate the results of treatment and the degree of recovery, the nature of the disease;
- help in the differential diagnosis of the causes of urination and/or potency disorders.
Side effects of NCS/EMG
There are rarely any side effects from the NCS procedure. Although there is some discomfort (noticeable for some) during the test, there are often no complications afterwards. Your doctor may avoid stimulating too close to your torso if you have a pacemaker or similar device.
Needle EMG may cause minor bruising of the skin and muscles. Usually this doesn't matter. With any such procedure (such as drawing blood), there is a small risk of infection. Once the procedure is completed, patients usually return home the same day. You should be able to drive yourself home as sedatives are not usually used.
Indications for research
Why is ENMG rarely prescribed by doctors? Perhaps there are few indications for ordering a study?
Below is a list of symptoms, syndromes, conditions and diseases for which electroneuromyography may be prescribed.
Symptoms:
- muscle weakness and/or increased fatigue;
- involuntary contractions, twitching, muscle cramps;
- atrophy (“weight loss”) of muscles;
- decreased or changed sensation in the limbs and/or face;
- pain in the arms/legs, accompanied by “lumbago”;
- neck and/or back pain;
- impaired potency and urination.
Here is an incomplete list of diseases for which it may be advisable to conduct electroneuromyography :
- ALS (amyotrophic lateral sclerosis, motor neuron disease)
- Diabetic polyneuropathy
- Lambert-Eaton myasthenic syndrome
- Myasthenia gravis
- Myelodysplasia of the spinal cord
- Myositis and polymyositis
- Myopathies
- Trigeminal neuritis
- Mononeuropathy
- Sciatic nerve neuropathy
- Bell's palsy (facial nerve neuropathy)
- Plexit
- Plexopathy
- Polymyalgia
- Polyneuritis
- Radiculopathy due to intervertebral disc herniation
- Guillain-Barre syndrome
- Carpal tunnel syndrome (carpal syndrome)
- Cubital syndrome
- Tolosa-Hunt syndrome
- SMA (spinal muscular atrophy)
- Trigeminal neuralgia
- Tunnel syndromes
- Fibular syndrome
- Chronic inflammatory demyelinating polyneuropathy (CIDP)
- Diabetes mellitus and diabetic polyneuropathy
- Myelitis, encephalomyelitis
- Deficiency of vitamins B, E, C
- Hypothyroidism, hyperthyroidism
- Systemic lupus erythematosus
- Vasculitis
- Multiple sclerosis
- Chronic pelvic pain
- Neurogenic bladder
As you can see, the list is not small, and most importantly, it includes not only purely neurological diseases. Diseases of internal organs often cause complications in the form of damage to the nervous system. For example, atrophic gastritis can lead to B vitamin deficiency, thereby triggering polyneuropathy or spinal cord damage. Well, the most famous example is damage to the nerves of the legs due to diabetes mellitus (diabetic polyneuropathy).
It seems that the main reason for the low use of ENMG and EMG is the difficulty in interpreting the results by doctors. The fact is that the maximum amount of information can be obtained only when the doctor performing ENMG is well versed in neurological diseases and symptoms, and the attending physician knows about all the nuances and features of electromyography. Otherwise, the diagnostician may not conduct the study in full, and the treating doctor may misinterpret the result, which will lead to an erroneous diagnosis.
Thus, in any case, the diagnostician must also be a neurologist; ideally, the examination should be performed by the attending neurologist himself, or ENMG should be carried out in the institution where the patient is being treated (in this case, there is feedback between the doctor and the diagnostician).
Which is correct - ENMG or EMG?
And finally, a little about the confusion in terminology. Two names for the study are often used: “electroneuromyography” (i.e. ENMG) and “ electromyography ” (EMG). As mentioned above, there is stimulation electromyography and needle electromyography. It is the needle one that is sometimes called “EMG” or “electromyography”, and the stimulation one – “electroneuromyography” or “ENMG”. Ultimately, there is no difference as such, because it is the combination of stimulation and needle methods that allows a comprehensive study of the pathological process. In addition, if a doctor refers you for examination, then it would be more correct on his part to either indicate which nerves and muscles he wants to examine and for what purpose, or (if the doctor conducting ENMG is a neurologist) leave the definition of the necessary The scope of the examination is at the discretion of the diagnostician.
In two parts of this article, we briefly reviewed the functional diagnostics of the central and peripheral nervous system. More precisely, with only two methods - evoked potentials and electroneuromyography. But, of course, there are many more such methods - this is known to many electroencephalography (EEG), and various types of long-term EEG monitoring, polysomnography, cardiorespiratory screening and many others. We'll talk about them another time.
Electromyography of the upper and lower extremities
We offer electromyography of the upper and lower extremities, mainly for polyneuropathy of various origins, damage and compression of nerves. ENMG in these cases helps to determine the cause and location of damage, compression or inflammation of the nerves of the arms and legs. Depending on the task of electroneuromyography, we can offer you myography of only the upper or lower extremities or a joint study of the upper and lower girdles (i.e. myography of the upper and lower extremities in one study); the price for electromyography of each belt in this case will be lower.
Stimulation electromyography of the lower extremities