General information
Neuroblastoma is an embryonal malignant tumor that is formed from immature cells (sympathogonia), which are the precursors of the sympathetic nervous system.
The manifestation of the disease is typical in childhood, mainly in young children and accounts for about 80% in the age group of children under 5 years. About 40% of cases of neuroblastoma occur in the first year of a child’s life, and as they grow older, the number of cases decreases. The average age of children at diagnosis is 22 months. The ratio of boys to girls is 1.2:1. The predominance of tumors of the sympathetic nervous system in children is primarily due to the peculiarities of its development, since the process of formation of sympathetic ganglia in the prenatal period does not end, and their cellular structure becomes similar to adults only by the age of 5 years. Accordingly, high tension/intensity of growth and development of the sympathetic nervous system creates conditions for tumor proliferation.
Neuroblastoma can be detected in any anatomical region along the sympathetic nerve chain. The most common neuroblastoma is the retroperitoneal space (45% of cases), in the adrenal glands (about 30% of cases), in the mediastinum 10-15% and the pelvis - about 3%. It develops much less frequently in the lungs, thymus, kidney, and even less often in other anatomical areas, for example, esthesioneuroblastoma (intranasal neuroblastoma). At the same time, at the time of diagnosis, about 50% of cases of the disease show signs of metastasis, mainly to regional/distant lymph nodes, bones, skin, bone marrow, liver, and less often to the central nervous system and lungs. Metastasis can occur both hematogenously and lymphogenously.
According to histological data, there are, in fact, neuroblastoma and a histologically relatively benign variant of the tumor - ganglioneuroblastoma , as well as a benign variant of the tumor - ganglioneuroma . That is, ganglioneuroblastoma, as a variant of the neoplasm, occupies an intermediate position between undifferentiated neuroblastoma and differentiated ganglioneuroma.
Biological features of neuroblastoma
Neuroblastoma is characterized by a number of specific biological characteristics of its behavior that are not characteristic of other malignant tumors:
- The ability of a tumor to undergo spontaneous regression. There are well-known examples in clinical practice when involution of the malignant process occurred in infants with severe clinical symptoms (stage 4 neuroblastoma). At the same time, in children under one year old with the first stage, tumor regression does not occur. And to date, any marker that causes a change in the progression from progression to regression has not been identified.
- The ability of neuroblastoma to differentiate (“maturation”). A cultural study revealed that during the cultivation process, the cell culture from an aggressively growing tumor acquired the characteristics of differentiating nervous tissue. And this process can be induced by various agents ( papaverine , some cytostatics, retinoic acid ) in vitro. But at the same time, to date there is no data on the induction of the differentiation process in vivo.
- The ability of neuroblastoma to aggressively develop rapidly and rapidly metastasize. It is generally accepted that the leading factors (markers) of progression are genetic disorders (deletion of 1 pair of chromosomes).
Currently, neuroblastoma is the most common and “problematic” tumor in childhood oncology with unpredictable biological behavior, most with unknown risk factors involved in etiopathogenesis, the difficulty of establishing a diagnosis in the early stages of the disease and the lack of effective treatment in advanced stages.
Treatment of neuroblastoma
Taking into account various scenarios for the development of disease outcome (from spontaneous regression to death from progression), risk-adapted principles are proposed in the treatment of neuroblastoma. Patients are stratified according to risk factors before treatment (usually clinical and molecular genetic data) and based on tumor response during treatment (response-adapted). When identifying risk groups before starting treatment, the following prognostic criteria are used: stage of the disease, age at diagnosis, results of molecular genetic data - MYCN amplification and deletion of the short arm of 1p (Fig. 8).
Rice. 8. Stratification of patients into risk groups according to the presence of unfavorable prognosis factors
Neoadjuvant (preoperative) polychemotherapy
- The need for polychemotherapy is determined by the stage of the disease and the presence or absence of unfavorable clinical and biological factors (n-myc amplification, short arm 1p deletions).
- Polychemotherapy allows you to reduce the size of the primary tumor to make surgery safer and more radical.
- The basic drugs for the treatment of neuroblastoma are vincristine, cyclophosphamide, anthracyclines, ifosfamide, platinum drugs, etoposide.
Features of surgical treatment
- For localized stages of the disease, treatment may be limited to complete removal of the tumor.
- In stages III-IV of the disease, the surgical stage is carried out after preoperative (neoadjuvant) polychemotherapy, which is aimed at reducing the size of the tumor with the aim of subsequent radical removal of the tumor.
- In cases where complete tumor removal is impossible, treatment is supplemented with radiation therapy in the postoperative period.
Adjuvant (postoperative) polychemotherapy
Drug treatment should be started 5-7 days after surgery. In the absence of indications for 2nd line polychemotherapy, treatment regimens use the same basic drugs as for neoadjuvant therapy.
Radiation therapy
- Radiation therapy is used to destroy any tumor cells that cannot be removed by surgery and/or that were not destroyed by previous therapies.
- If the operation is non-radical and involves the presence of an active residual tumor, the residual tumor tissue, the lymph nodes involved in the process, and the areas of communication of the tumor with surrounding organs and tissues are irradiated.
- Irradiation is carried out daily, starting from the 5-7th day after surgery.
- According to indications, irradiation of metastatic foci is carried out (for therapeutic, sometimes for analgesic purposes).
If there are unfavorable prognostic factors, in particular the detection of a MYCN oncogene mutation in the tumor, high-dose chemotherapy with autologous hematopoietic stem cell transplantation is recommended.
For patients with a high risk of relapse (advanced stages of the disease with the presence of unfavorable molecular genetic markers), “maintenance” differential therapy with 13-cis-retinoic acid and passive immunotherapy with anti-GD2 monoclonal antibodies is recommended.
Immunotherapy
Immunotherapy is a new treatment for neuroblastoma that is used to destroy cancer cells. Disialoganglioside GD2 is an antigen molecule expressed by neuroblastoma cells, making it an ideal target for antibody immunotherapy: the antibody acts against this molecule. Immune system cells may contribute to the death of neuroblastoma cells.
At the National Medical Research Center of Oncology named after. N.N. Petrov performs all stages of treatment, including minimally invasive operations (laparoscopic and thoracoscopic), tandem transplantation and passive immunotherapy.
By intensifying therapy in children with high-risk neuroblastoma (with the inclusion of tandem high-dose polychemotherapy in consolidation and passive immunotherapy in post-consolidation), it was possible to increase survival results by 20%.
Classification
There are different classifications of neuroblastoma based on tumor size/extension, one of which is summarized below:
- The first stage is characterized by the presence of a single node not exceeding 5 cm with the absence of metastases.
- The second stage is characterized by the presence of a single node, the size of which can vary between 5-10 cm, metastases , and the lymph nodes are not affected.
- The third stage - the size of the node does not exceed 10 cm, damage to the lymph nodes is noted, there are no metastases to distant organs, or the size of the tumor exceeds 10 cm without metastases .
- Fourth (A) stage - a tumor of any size is determined, lymph nodes are involved in the process and the presence of distant metastases.
- Fourth (B) stage – multiple tumor nodes with synchronous growth or a large single neoplasm, metastases to adjacent and distant organs are determined.
Types and localizations of neoplasms
Depending on the degree of differentiation, neuroblastomas are divided into:
- Ganglioneuroma is a benign tumor of ganglion cells, considered a mature form of neuroblastoma. There is a possibility of neuroblastoma maturing into ganglioneuroma, which does not metastasize.
- Ganglioneuroblastoma is an intermediate form between the other two. In its various sections there are both benign and malignant cells.
- An undifferentiated form of the tumor , the most malignant of all. Consists of round cells with dark spotted nuclei. Calcifications and hemorrhages may be found in the tumor.
Where is the possible location of the tumor?
There are 4 main forms of tumor, depending on location:
- Melulloblastoma - this tumor is located deep in the cerebellum and is often not operable. Aggressive, metastases appear quickly, which can lead to rapid death of the patient. Characterized by symptoms of incoordination at an early stage.
- Retinoblastoma is a malignant neoplasm of the retina. Symptoms often include visual impairment and blindness, and metastasize to the brain.
- Neurofibrosarcoma is a neuroblastoma, which is located in the retroperitoneal space, most often metastasizing to the bones and lymph nodes.
- Sympathoblastoma - can be localized in the chest cavity and adrenal glands. If the adrenal glands become enlarged, it can lead to paralysis.
Causes
To date, the causes of neuroblastoma are unclear. Failure of the process of cell differentiation can probably occur under the influence of endogenous/exogenous factors, while exogenous causes of neuroblastoma in children do not seem to play a significant role. Mutations acquired under the influence of unfavorable factors are considered to be the leading cause of the development of neuroblastoma. A correlation has been established between the development of neuroblastoma and congenital immune /developmental anomalies. The hereditary nature of neuroblastoma of the autosomal dominant type is detected only in 1-2% of cases.
These tumors are characterized by: unique/specific molecular genetic characteristics, which is manifested cytogenetically by the addition of genetic material in the form of homogeneously colored areas/in the form of a comma or loss of heterozygosity of the short arm of the first chromosome (in the form of a 1 p deletion). Changes of this kind significantly correlate with advanced stages of tumor development and poor prognosis. Also extremely important is the fact of changes in DNA ploidy in tumor cells, and therefore hyperploidy with a triploid DNA index is distinguished, which is characterized by a favorable course and tetraploid forms with an unfavorable course. Determining the expression of receptors for autonomic NS growth factors (neurotrophins) is also of great importance. At the same time, a high probability of a favorable prognosis is characteristic of the expression of the trk A receptor, while high expression of trk B correlates with an unfavorable outcome.
Risk factors for neuroblastoma
A risk factor is something that increases the likelihood of developing a tumor.
Lifestyle factors are major factors in adult cancer. Examples include an unhealthy diet (low intake of fruits and vegetables), physical inactivity, smoking and drinking alcohol. Risk factors associated with children's lifestyle do not affect the occurrence of malignant tumors.
The likelihood of neuroblastoma occurring around the world is almost the same. This suggests that environmental factors, such as pollution, are not the cause of the development of this tumor.
The only known risk factor for neuroblastoma is heredity. It is believed that some people may very rarely inherit the risk of developing neuroblastoma. Only in 1-2% of cases is the familial form of neuroblastoma diagnosed, i.e. the occurrence of a tumor in a child in whose family there were cases of this disease.
The average age of patients at the time of diagnosis of familial cases of neuroblastoma is 9 months. This is less than the age of patients with sporadic (non-inherited) cases of tumor. In addition, children with familial neuroblastoma may develop two or more similar tumors in different organs, such as both adrenal glands.
It is important to distinguish neuroblastomas, which develop simultaneously in different organs, from metastatic neuroblastoma, when the tumor arises in one organ and then spreads throughout the body. If neuroblastoma occurs in several places, then a familial form of the disease can be assumed. Neuroblastoma metastases can occur in both familial and sporadic cases of the tumor.
Symptoms
The initial symptoms of neuroblastoma are not specific and can manifest with various symptoms, which is determined by the primary location of the tumor, the presence/localization of metastases, as well as the amount/volume of vasoactive substances produced by the tumor and metabolic disorders. As the tumor grows, symptoms increase. The main symptoms of neuroblastoma in children include pain, fever and weight loss. In some cases, diarrhea , which is due to the production of vozointestinal peptides by the tumor.
For a long time, a number of patients may be asymptomatic or exhibit “minor tumor signs” in the form of decreased appetite, unusual lethargy, weight loss, low-grade fever, pallor of the skin, periodic abdominal pain, sleep disturbances, diarrhea/constipation and vomiting for no apparent reason, pain in the limbs.
As the tumor, located on the neck, in the abdominal/pelvic cavities, and in the chest, grows, adjacent structures are compressed, which forms the corresponding symptom complex. When the tumor is localized in the neck/head area, the first symptoms are often: the appearance of Horner's syndrome (ptosis, miosis, hyperemia and anhidrosis on the affected side) and palpable tumor nodes . With retrobulbar localization in children (stage 4) of the disease, the symptom of “glasses” with exophthalmos is characteristic. When neuroblastoma is located in the posterior mediastinum, respiratory disorders, obsessive cough, dysphagia, frequent regurgitation, and later - deformation of the chest wall are characteristic. Developing in the chest, the tumor causes dysphagia , breathing problems, and compression of the veins. When the tumor is localized in the pelvis, urination/defecation disorders may occur.
Symptoms of retroperitoneal neuroblastoma most often manifest as decreased appetite and abdominal pain not associated with eating. Palpation reveals a dense, immobile, tuberous tumor in the epigastrium/left hypochondrium, extending into the midline. The clinical picture of a tumor in the retroperitoneal space is complemented by severe general symptoms in the form of weakness, weight loss, the appearance of joint/ bone pain , fever , and anemia .
With paravertebral localization without/or with penetration into the spinal canal, neurological symptoms (flaccid paralysis of the limbs/impaired urination) are characteristic. Metastases to the skin are characterized by a dense consistency and bluish-purple color.
Symptoms caused by metastases to a particular anatomical zone also vary significantly. In newborns, the first sign of metastasis is a rapid enlargement of the liver, often accompanied by bone marrow damage/the formation of bluish nodules on the skin. In older children, the process of metastasis may be accompanied by enlarged lymph nodes and bone pain. of leukemia (hemorrhages on the skin/mucous membranes and anemia) appear less frequently
How common are neuroblastomas?
Neuroblastoma is the most common tumor in infants and is the fourth most common malignant tumor in older children, after acute leukemia, central nervous system tumors, and malignant lymphomas.
Every year, 6-8 children per 1 million children under 15 years of age (average age 2 years) become ill with neuroblastoma in Russia.
Approximately 650 new cases of neuroblastoma are diagnosed each year in the United States, a number that has remained stable for many years. Neuroblastoma occurs slightly more often in boys than in girls. For every 6 cases of tumors in boys, there are 5 cases in girls.
The average age of patients at the time of diagnosis is 17 months. One third of cases are diagnosed in children under 1 year of age. Almost 90% of neuroblastomas are detected before 5 years of age. Only 2% of tumors are detected after the age of 10 years and in adult patients. In rare cases, neuroblastoma can be detected by ultrasound before the baby is born.
In 7 out of 10 cases, neuroblastoma already has metastases at the time of diagnosis.
Tests and diagnostics
The diagnosis is made on the basis of a physical examination of the child, complaints, as well as:
- Laboratory data (blood test) to determine the level of neuron-specific enolase in the blood. Possible leukopenia/leukocytosis, accelerated ESR, thrombocytosis.
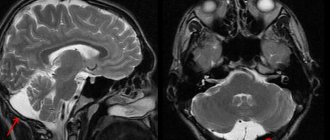
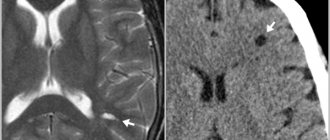
- Instrumental examinations: ultrasound tomography of the retroperitoneal space, CT, MRI of various areas and other diagnostic procedures. Carrying out aspiration puncture of the bone marrow with a cytological examination of the obtained material from 3 points, scintigraphy with metaiodobenzylguanidine/radioactive technetium.
A specific marker of neuroblastoma is a change in the genome of tumor cells (amplification of the N-myc proto-oncogene), which is determined by the FISH reaction or other methods. The presence of a genetic abnormality has prognostic significance and largely determines the choice of treatment tactics.
Forecast
The survival prognosis for neuroblastoma is determined by a number of factors: the age of the child, the stage of the disease, and the morphohistological structure of the tumor. Accordingly, with modern neuroblastoma treatment programs, the overall 3-year survival rate of patients is:
- at stages 1 and 2 of the disease varies between 95-99%,
- at stage 3 this figure is 80-98%;
- survival rate for stage 4 ranges from 60-76%.
At the same time, the prognosis is more favorable for children under 1 year of age. Regarding tumor location, the maximum number of unfavorable outcomes is observed when neuroblastoma is localized in the retroperitoneal space, and the minimum number is observed when localized in the mediastinum.
What is the survival rate of patients?
The prognosis and survival of patients with neuroblastoma depends on the following factors: age (the most significant), stage of the disease, ferritin level in the blood, morphological structure of the tumor.
Children under one year of age have the most favorable prognosis. When diagnosing a disease for:
- stage I : more than 90% of patients cross the 5-year survival threshold;
- stages IIA and B: 70-80%;
- stage III: 40-70%;
- stage IV : if the patient is older than 1 year - 20%;
- stage IVS : there is a slightly more favorable prognosis associated with the possibility of spontaneous regression of the tumor - 75%.
There is no specific tumor prevention. The influence of any factors on the likelihood of this type of cancer has not been proven, so there are no ways to prevent it.
To improve your survival prognosis, it makes sense to visit the clinic regularly, get tested periodically, and monitor for symptoms that may indicate the presence of a tumor.
List of sources
- Epidemiology and biology of neuroblastoma (literature review) Fedyakova Yu.S. // Children's Oncology No. 3-4 2009; With. 32-35.
- Oncology. National leadership. Ed. Chissova V.I., Davydova M.I. M.: GEOTAR-Media. 2008; pp.956-962.
- Boyarshinov V.K. Treatment of stage IV neuroblastoma: Abstract. dis. Ph.D. honey. Sci. - M., - 2006 - P.9-19.
- Cherstvoy E.D., G.I. Kravtsova, A.V. Furmanchuk: Tumors of the sympathetic nervous system. In the book: Tumors and tumor-like processes in children // Minsk: Askar, -2002. P.125-137.
- Shorikov E.V., Popova T.P., Lemesheva O.V., Semenikhina E.R., Tsaur G.A., Savelyev L.I. Retrospective analysis of the effectiveness of program treatment of patients with neuroblastoma // Children's Oncology, -2008.- No. 2 P. 83-88.