In neurosurgical practice, brain tumors are divided into primary and secondary. Primary ones include those that are formed in brain tissue, nearby lymph nodes, cranial nerves, and blood vessels. Secondary (daughter) are the result of metastasis of cancer cells from other organs.
The choice of therapy depends on the histological type and location of the tumor. The main methods of treatment include scalpel or laser operations, chemotherapy and radiotherapy. Very often all these methods are combined with each other.
Surgical intervention
Brain surgery is a complex, time-consuming process, the consequences of which are unpredictable and determined by the location of the tumor. Any complications, such as bleeding, infections, damage to blood vessels and nerve fibers, swelling, can lead to negative cognitive and motor changes:
- paresis - loss of muscle strength with impaired coordination and gait, tremors of the limbs;
- apraxia - the inability to perform habitual or consistent movements necessary to carry out goal-directed tasks;
- agnosia – the inability to identify objects through the senses due to disorders of information perception: auditory, visual, gustatory, olfactory, tactile, spatial;
- hemianopsia – loss of visual fields;
- aphasia – complete or partial loss of speech;
- dysarthria – distorted and difficult pronunciation of certain sounds and words;
- alexia – difficulties in recognizing letters and understanding the meaning of what is read;
- agraphia – loss of writing skills, coordination of letters, prepositions, syllables, even with preserved intelligence;
- deterioration of memory, attention, thinking.
Mental dysfunction may also occur for another reason. During the period of tumor growth, the brain was subjected to compression of certain sections responsible for certain functions, to which it managed to adapt. But as a result of the removal of the neoplasm, the tissues find themselves in an unusual position for them, and this also becomes the basis for disruptions in cerebral activity.
Priority is given to the surgical method when the malignant tumor has clear boundaries. Contraindications for surgery are:
- multiple foci of the tumor process;
- severe chronic diseases in the acute stage;
- metastatic lesions of surrounding tissues;
- cachexia – extreme exhaustion.
Increasing headaches in the postoperative period are rare and should be reported to medical staff immediately, as they signal intracranial edema. In such a situation, drips with analgesics are prescribed and steroids are added.
Types of tumors
Neoplasms that form in the brain can be:
- Benign – tumor tissue does not contain cancer cells. Neoplasia of this type is characterized by clear edges and slow growth. They are much easier to treat surgically, but can become malignant, that is, turn into cancer;
- Malignant tumors contain abnormal cells that can divide uncontrollably and metastasize to other organs. In this case, the disease is difficult to control; in the later stages, surgery is impossible. Treatment in this case is difficult, has a high cost and, as a rule, poor prognosis.
Brain glioma
Glioma
This type of tumor is diagnosed more often, accounting for approximately 60% of all types of cancer that form in the brain. The tumor is formed from glial cells. In most cases, this is a primary neoplasm, most often formed in the area of the chiasmata or ventricles, but it can also affect the brain stem; pathogenesis rarely extends to the bones of the skull, however, in rare cases this is possible. The size of gliomas is usually up to 14 cm. Metastases are rare, growth is usually slow, but due to penetration into adjacent tissues, the boundaries of the lesion are difficult to distinguish.
Three varieties are known
- astrocytoma – diagnosed more often than others (it accounts for about 50% of gliomas);
- oligodendroglioma – up to 10% of cases;
- ependymoma – less than 7%.
According to the World Health Organization classification, there are 4 stages of glioma:
- The first stage is benign. It is characterized by slow growth. Example: giant cell astrocytoma.
- Second stage. Features: borderline malignancy with slow tissue growth, easily progresses to stages 3 and 4. In this case, only one symptom of cancer is identified - cellular atypia.
- Third and fourth stage. In this case, the tumor has all the signs of cancer, for example, necrotic changes in glioblastoma multiforme.
Brain astrocytoma
Removal of a large GRADE II WHO astrocytoma of the right temporal lobe (before surgery)
This malignant neoplasm of varying degrees of aggressiveness is diagnosed quite often. The beginning is given by degenerated glial cells - astrocytes (hence the name - astrocytoma). There are:
- Common astrocytomas: protoplasmic, fibrillary and hemisrocytic.
- Special astrocytomas: cerebellar, piloid, microcystic and subependymal.
Astrocytomas are distinguished by the stage of malignancy:
- The first stage (benign tumor) includes piloid or pilocytic astrocytoma of the brain.
- Second stage of malignancy: fibrillary tumor is also an ordinary neoplasia, second degree of malignancy.
- The third stage is already cancer. It includes anaplastic astrocytoma of the brain.
- The most life-threatening are glioblastomas (giant cell glioblastoma and gliosarcoma), which are classified as stage 4 and are characterized by rapid growth and the ability to metastasize.
In addition to the ones mentioned, there are other types of astrocytomas, for example, ependymoma (develops from ventricular cells), oligodendroglioma (forebrain) - grow quite slowly without the formation of metastases, and glioma of the brain stem.
Meningioma of the brain
Removal of a large middle cranial fossa meningioma before surgery
Pathogenesis begins with pathogenic cells in the superficial membrane that surround the brain tissue. The neoplasm is oval in shape, grows slowly, and is therefore considered benign. Meningiomas are diagnosed in 15% of cases (of all brain tumors). The risk of degeneration into cancer is about 3-4%. The clinical signs that appear are caused by increased intracranial pressure and tissue compression. With malignancy (degeneration of somatic cells into carcinogenic ones), meningiomas become aggressive. Usually more than one lesion forms and may spread to the spinal cord. After surgical treatment, there is a high probability of relapses. As a rule, pathology is diagnosed by chance, because symptoms appear only when the lesion reaches a large size. There are no early signs of the disease.
Note. Meningiomas often form in females.
Other types of brain tumors
There are quite a lot of types of neoplasms. Here are some of those that are diagnosed relatively often (besides those mentioned above):
- medulloblastoma is a brain cancer that originates from the structures of the cerebellum;
- germinoma - formed from germ cells, most often it is detected in the first half of a person’s life;
- Craniopharyngeoma - develops in the pituitary gland at the base of the brain;
- Shawnoma – formed from degenerated Schwann cells;
- tumors in the pineal gland area.
Chemotherapy
Chemotherapy drugs can have a neurotoxic effect on the central nervous system, resulting in cognitive impairment. The effect of cytostatics is expressed in the cessation of the processes of growth, development, and the mechanism of cell division, unfortunately, not only malignant, but also normal. Antitumor agents are administered in various ways:
- orally – through the mouth;
- parenterally - by administering intramuscular, intravenous, intra-arterial injections;
- directly into the tumor itself or surrounding tissues;
- in the cavities remaining after removal;
- into the epidural space (cerebrospinal fluid).
Since all these drugs are substances with high biological activity and lack of selectivity, the bone marrow, mucous membranes of the digestive system, and hair follicles are affected. The severity and frequency of adverse events depend on the type of cytostatic, dosage used, administration regimen, and general condition of the patient. The most common side effects:
- inhibition of hematopoiesis (leukopenia, thrombocytopenia, anemia);
- symptoms of intoxication – nausea, vomiting, diarrhea;
- stomatitis;
- alopecia – loss of hair on all parts of the body;
- allergic reactions - rash, skin itching, erythema;
- development of cardiomyopathy;
- neurotoxicity;
- hepatotoxicity;
- nephrotoxicity;
- thrombophlebitis and phlebosclerosis;
- local irritating effect with necrosis and ulceration up to exposure of tendons and muscles;
- flu-like syndrome - chills, fever, weakness, headache and muscle pain.
The selection of a specific drug depends on the sensitivity of living cancer cells taken from the human body to it. Resistance is determined through testing, which makes it possible to avoid taking ineffective drugs and not waste time.
Cost of treatment
| Name of service | price, rub. | Unit measurements |
| Consultation with an oncologist and radiotherapist | 1 500 | PC. |
| Consultation with a pediatric oncologist | 0 | PC. |
| Repeated consultation with specialists | 500 | PC. |
| Primary topometry on a specialized computed tomograph | 15 000 | procedure |
| Repeated topometry on a specialized computed tomograph | 7 000 | procedure |
| Primary dosimetric planning of radiation therapy (tomotherapy) | 20 000 | PC. |
| Repeated dosimetric planning of radiation therapy (tomotherapy) | 7 000 | PC. |
| Radiation therapy (tomotherapy), including IMGRT (*) | 315 000 | well |
| Radiation therapy (tomotherapy) stereotactic radiofrequency surgery (*) | 315 000 | well |
| Accompanying drug therapy: intravenous administration in the treatment room (excluding the cost of medications) | 1 000 | procedure |
| Accompanying drug therapy: intramuscular administration in the treatment room (excluding the cost of medications) | 200 | procedure |
| Topometric marking | 750 | procedure |
| Conducting a study of the radiation therapy plan using absolute dosimetry on a specialized phantom “Cheese Phantom Accuray” | 15 000 | procedure |
| Carrying out the quality assurance (QA) procedure for the radiation therapy plan on the specialized phantom “PTW Octavius” | 30 000 | procedure |
The type of radiation therapy and the number of sessions of the course are determined by the medical commission individually for each patient based on the location, nosology of the tumor and taking into account the medical history.
Free online consultation
Sign up
Radiation therapy
At the end of its implementation, undesirable reactions may also occur due to the effect of gamma rays on nearby tissues, damage and decay of destructive cells. They develop 1-2 weeks after treatment, manifesting themselves in the form of:
- reduction of leukocytes, platelets, red blood cells;
- general intoxication – nausea and vomiting;
- dryness, peeling, itching of the skin of the head and neck, red spots, blistering rashes;
- hemorrhages, ulcers, soft tissue burns;
- hearing loss due to swelling of the auditory canal;
- diplopia (double vision);
- hair loss;
- loss of appetite;
- feelings of fatigue and malaise;
- impaired coordination and seizures.
This treatment is used both individually and in the postoperative period to remove residual structures growing into surrounding tissues.
One of the methods of radiation therapy is stereotactic radiosurgery, the principle of which consists in a single irradiation of pathological foci with high doses using the Gamma Knife and CyberKnife devices. It is an alternative to traditional operations and allows manipulations to be performed without general anesthesia, tissue excision and craniotomy. It is characterized by high accuracy and low risk of complications. The big disadvantage of the technique is the delay in the result, so in cases of acute symptoms it is not used.
Causes of brain tumors in adults and children
According to official statistics, about 6% of all neoplasms are tumors in the skull. In childhood, they are less common; in older people, the risk of developing benign or malignant tumors is higher, and treatment is more difficult. Although there is still no exact data on why cells change structure and begin to grow uncontrollably. A relationship has been identified between the development of tumor processes and the following factors:
- some genetic diseases, oncology in relatives;
- exposure to toxins, carcinogens, ionizing radiation;
- immunodeficiency states;
- traumatic brain injuries;
- intrauterine disorders of the development of fetal brain tissue.
Contraindications after surgery
Despite the great successes of modern medicine in creating new protocols and equipment, treating pathology is a rather complex process that requires physical and mental effort. Rehabilitation after removal of a brain tumor under the guidance of professionals will help you overcome the consequences of the disease and return to your previous lifestyle. And it begins with a number of prohibitions under which the following are unacceptable:
- drinking alcohol for a long period;
- visits to the sauna, bathhouse;
- air travel for three months;
- active sports throughout the year, which pose a risk of head injury (hockey, football, boxing);
- exposure to the sun and solarium;
- jogging. It is better to replace them with brisk walking;
- sankur and mud therapy.
How is the operation performed?
Neurosurgical operations to remove malignant tumors are complex and high-tech. It is important for the doctor to remove the tumor completely, without damaging functionally significant areas of the brain.
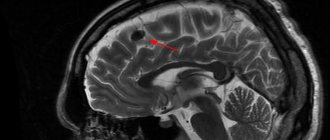
The procedures that determine the success of the operation often begin before it even begins. Doctors conduct a thorough examination of the patient, especially if the tumor is deep. They determine the boundaries of the tumor using PET or functional MRI. Then it is necessary to identify functionally significant areas in order to bypass them by dissecting the brain tissue. For this purpose, functional mapping and electrophysiological studies are used. If necessary, studies can be performed directly during surgery.
The operation is performed under stereotactic control. Stereotaxis allows the doctor to perfectly navigate inside the patient's skull. The classic version involves the use of a rigid frame, which is fixed with screws to the periosteum. In recent years, frameless stereotaxis systems have become widespread.
The most important task of the neurosurgeon, which determines the success of the operation, is to completely remove the tumor. But to do this, it must be distinguished from healthy tissue. They look almost the same. To find the boundaries of the tumor, fluorescent diagnostics and laser spectroscopy are used. The doctor uses a substance that is absorbed by abnormal cells and causes them to glow.
A German study involving 350 patients showed that without fluorescent diagnostics, glioblastoma can be completely removed in only 1 out of 3 patients, and in 2/3 of cases with its use. The probability of no tumor recurrence within 6 months after surgery increases by 2 times.
Our expert in this field:
Malakhov Igor Yurievich
Neurosurgeon
Doctor of the highest qualification category
Experience: More than 27 years
Call the doctor
Call the doctor
What is included in rehabilitation
Recovery takes quite a long time, and in order to restore previous brain functions, you need to start neurorehabilitation as early as possible. For this purpose, specialists from many fields and various equipment are involved. A multidisciplinary team of doctors, teachers, and nursing staff develops an individual program adapted to each patient. Drug neurological therapy is combined with the services of a defectologist, neuropsychologist, and speech therapist. Among the methods used:
- physiotherapy using inductothermy, laser therapy, UHF, electrophoresis, magnetic therapy to stimulate metabolism, relieve pain, accelerate regeneration, etc.;
- Exercise therapy with special simulators aimed at increasing the mobility of the limbs, fine motor skills of the hands, reducing swelling and stiffness in them. Exercises will help restore body balance, the ability to sit, stand and walk;
- kinesiotherapy and acupuncture - influencing bioactive points to stimulate all kinds of biological processes;
- psychotherapeutic assistance - relieving signs of depression, overcoming fears and complexes, acquiring a positive attitude;
- therapeutic massage – improving blood supply, elasticity and muscle tone, increasing immunity;
- occupational therapy – training in self-care, personal hygiene, acquisition of housekeeping skills, use of household appliances without outside participation;
- diet therapy – balanced nutrition optimized for the patient’s characteristics.
In some situations, you will need support from chemotherapists and radiologists and diagnostic monitoring.
Today, cancer treatment has reached a new level. The developed unique technique, the degree of effectiveness of which has been proven by more than twenty years of practice, gives hope to many patients. The action of a unique technique used in our clinic by Dr. Borisov, called Selective Chronophototherapy (SPT), which is based on photodynamic therapy, is capable of activating a cascade of biochemical and cellular reactions to regulate the level of immune status indicators, demonstrates excellent results both when used independently and in combination with other methods. This significantly reduces the risk of relapse of cancer and the severity of side effects from cytostatic agents, while enhancing their effect on the affected cells.
Dr. Borisov’s gentle technique can be used repeatedly; a course of treatment is recommended. The number of procedures is regulated by the treatment regimen and achievement of the desired result.
We recommend taking VIALIFE capsules or VIALIFE solution, because they contain the highest possible concentration of chlorophyll, which:
- strengthens the immune system;
- enhances cell regeneration;
- saturates tissues with oxygen;
- has antioxidant, anti-inflammatory, detoxifying effects.
Diagnostics
Since brain tumors do not have specific symptoms, the doctor will have the task of excluding other diseases and space-occupying processes in the skull, and also finding out whether it is a primary tumor or metastases from other organs.
Magnetic resonance imaging (MRI) is the most informative in this regard. Using this method, it is possible to carry out differential diagnosis quite reliably and even clarify the nature of the primary neoplasm. Contrast-enhanced MRI can accurately determine the location and number of metastatic tumors and is significantly superior to computed tomography (CT), which is more sensitive in assessing hemorrhage and bone changes. MRI is effective in detecting metastases in 70-80%, while CT is effective in only 50% of patients.
In addition to MRI, the mandatory scope of examination also includes:
- electroencephalography, to exclude convulsive activity; X-ray of the chest organs, ultrasound of the abdominal cavity and pelvis, bone scintigraphy - to search for the primary tumor (for metastases to the brain);
- blood tests to assess the general condition of the body and the functioning of the liver and kidneys;
- if a primary lesion is detected, it is assessed using CT or MRI;
- if there are metastases to the brain, but the primary focus cannot be found using the methods listed above, then CT of the abdominal cavity and pelvis, CT of the chest, MRI or positron emission tomography (PET) of the whole body, and endoscopic examinations of the digestive organs are used.
The final diagnosis is made based on the results of histological examination of the tumor. To do this, its cells are studied under a microscope and their structure is compared with the structure of normal cells. Tumor tissue can be obtained in different ways:
- Open biopsy. If the tumor is located superficially and is accessible to surgical intervention, then craniotomy is performed, the tumor is removed and sent for analysis.
- A puncture biopsy is performed if the risk of the operation outweighs the possible benefit from it. In this case, tissue sampling is carried out with a thin needle.
- Stereotactic biopsy is indicated for tumors that are difficult to access or have contraindications for open surgery. It is a puncture biopsy, which is carried out under the control of complex neuronavigation systems.
Modern navigation systems during stereotactic biopsy allow you to control the movement of the needle with an accuracy of tenths of a millimeter.
Rehabilitation goals
The objectives of the program include preventing metastasis and relapse of cancer, reviving lost functions, and activating thought processes. Fortunately, the human brain has great potential for recovery if its structures are not permanently damaged. For example, a violation of the part of the cortex responsible for speech is compensated by training fine motor skills. At the time of brain regeneration, growth factors are produced, which not only recreate damaged fragments, but also stimulate the growth of new ones. Therefore, the main mission of neurorehabilitation is to provide the brain with external stimuli and appropriate medical support.
Cognitive rehabilitation is aimed at renewing conversation skills, long-term and short-term memory, and the ability to concentrate and maintain attention. For this, nootropic drugs are used in conjunction with gaming techniques (putting words together from puzzles, writing diaries). If complete restoration of functions is impossible, every effort must be made to adapt the person to the limitations that have arisen, which will make his life much easier.
Physical activity
In the first postoperative days, light breathing exercises are performed to prevent hospital-acquired pneumonia, blood clots and other complications associated with physical inactivity. After the patient is transferred from intensive care and the condition is stabilized, attention is paid to restoring lost movements. If there are no contraindications, you are allowed to stand on your feet and try to walk. Then additional devices are added - weights, balls. Exercises should be performed without pain or fatigue.
It is important to constantly emphasize and praise patients in order to motivate them to achieve new successes, since most of them are prone to denial and depression. Positive dynamics will make it possible to understand that life is not over and a return to the previous existence is quite achievable.
Doctors at Doctor Borisov's Clinic provide assistance to people with disabilities of varying degrees of complexity. This is a difficult period both for those undergoing surgery and for their family members. But you need to be prepared for the fact that it will take a lot of time for a complete recovery or it will be impossible to achieve the previous level of condition. Our specialists try to do everything to get the most positive results. We invite you to a free initial consultation, where we can get acquainted with your problem and together find ways to solve it.