Neuralgia refers to severe shooting pain that occurs due to a damaged or irritated nerve. Neuralgia can affect any part of the body, causing mild to severe pain. Certain medications and surgical procedures can effectively treat neuralgia.
Severe neuralgia can affect a person's ability to perform everyday tasks and can affect their quality of life.
Neuralgia has many possible causes, including:
- infections such as shingles, Lyme disease, or HIV
- pressure on bone nerves, blood vessels or tumors
- other medical conditions such as kidney disease or diabetes
- aging
This article examines the different types of neuralgia, their symptoms, and available treatment options.
general information
There are 12 pairs of intercostal nerves in the human body. They originate from the roots of the thoracic spinal cord and cover the entire chest, adjacent to the peritoneum, muscles, skin and mammary glands. The individual fibers of each nerve are responsible for tissue sensitivity, motor function and regulation of the functioning of all structures. Accordingly, damage or inflammation in any area can radiate pain to a variety of parts of the body.
The sensations can imitate diseases of internal organs: myocardial infarction, angina pectoris, pancreatitis, gastritis, cholecystitis, etc. In some cases, only a doctor can accurately determine the nature of the pain after a full examination. That is why it is important to seek help promptly if chest pain occurs.
Make an appointment
Causes of postherpetic neuralgia
Once a person has had chickenpox, the virus remains in the body for life. With age, the immune system weakens (particularly from taking medications or chemotherapy) and the virus can become more active, resulting in shingles.
Damage to nerve endings during rashes leads to postherpetic neuralgia. When damaged, nerve fibers cannot send signals from the skin to the brain as they normally do. Instead, they transmit amplified signals, and the patient feels excruciating pain that can last for months or even years.
Forms
There is no special classification of the disease. There are several separate forms depending on the mechanism of occurrence:
- radicular: associated with irritation of the spinal cord roots at the point of their exit from the spinal column;
- reflex: associated with overstrain of muscle fibers at the site of the nerve passage.
There is also a classification of neuralgia depending on:
- causes: primary (associated with damage or inflammation of the nerve itself) and secondary (due to other diseases);
- localization: unilateral and bilateral;
- course of the disease: acute and chronic.
Symptoms of neuralgia on the right and left
Any neuralgia, including intercostal neuralgia, is primarily pain. Painful sensations can be of a different nature (aching, dull, sharp, piercing, burning) and have different intensity. Sometimes the pain is so severe that it forces a person to take a forced position and sharply limit physical activity. Intercostal neuralgia, which has pronounced symptoms, is described by patients as a lumbago or electric current discharge running from the spine to the sternum.
Thoracalgia often begins gradually, with a tingling sensation in the intercostal spaces, then acquires pronounced intensity. Less often it occurs suddenly. The pain can radiate to the scapula, epigastric area, heart, arm and lower back. Sometimes it takes on an encircling character. It intensifies with changes in body position, movements, coughing and deep breathing.
As a rule, painful attacks are constantly repeated, lasting from a few seconds to 2-3 minutes. Therefore, treatment of acute intercostal neuralgia on the right and left, first of all, always begins with the elimination of pain.
In addition to thoracalgia, a person may be bothered by characteristic local signs caused by the influence of sympathetic, sensory and motor nerve fibers. Intercostal neuralgia, depending on the damage to a particular nerve, will have characteristic symptoms on the right, left or both sides of the chest:
- impaired sensitivity, crawling sensation, numbness, tingling;
- muscle twitching;
- increased sweating;
- change in skin color.
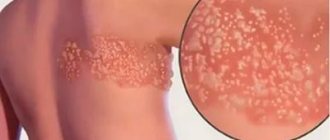
If chest neuralgia appears against the background of a herpes infection, it may be accompanied by skin rashes. The latter appear 2-4 days after the onset of thoracalgia. Elements of the rash are located on the skin of the intercostal space in the form of small pink spots, which then turn into vesicles and then into crusts. Subsequently, traces of pigmentation may remain on the skin.
Causes
The list of main causes of intercostal neuralgia includes:
- degenerative-dystrophic diseases of the spine: osteochondrosis, arthrosis, hernias and protrusions of discs, etc.;
- uneven or excessive load on the spine and back muscles (due to carrying heavy objects, poor posture, etc.);
- spinal column deformities (primarily scoliosis);
- diseases of the nervous system, in particular multiple sclerosis;
- infectious lesions: tuberculosis, herpes zoster, influenza;
- injuries of the spine and chest, surgical interventions in this area;
- tumors in the ribs, sternum, spinal column;
- taking certain medications;
- increased load on the respiratory muscles and abdominal muscles;
- increased intra-abdominal pressure, including during pregnancy.
In addition, intercostal neuralgia can occur secondary to other diseases, for example, pleurisy, pathology of the digestive system, kidney disease, thyrotoxicosis, and immunodeficiency states. Adolescents during the period of active skeletal growth may also experience similar symptoms.
Material and methods
In order to study the therapeutic potential of the original drug meloxicam (movalis) for acute LBP, the CARAMBOL study (Clinical Analysis of the Results of Analgesia with Meloxicam and its Safety in Acute Lumbargia) was conducted. The work was observational in nature and did not involve interference with the usual treatment process or the prescription of new medications or therapeutic methods. The duration of use of NSAIDs to relieve NBS was determined by the attending physician, based on clinical recommendations and personal experience. The prescription of other drugs was not limited: muscle relaxants, B vitamins and proton pump inhibitors (PPIs).
The study included 2078 patients with NBS, mean age 46.3±13.4 years, 56.6% women. In 34.8% of patients, a real episode of LBP occurred for the first time, in 65.2% it occurred repeatedly. Over the previous year, patients experienced from 2 to 12 (on average 2.61±1.35) cases of NBS: 2 episodes - in 59.3%, 3 - in 27.5%, 4 - in 10.5%, 5 or more - in 2.7% of patients.
Inclusion criteria
into the study: age 18 years and older, the fact of visiting a doctor in connection with acute severe pain in the lower back (duration no more than 2 weeks, severity of 4 points or more on a numerical rating scale - NRS), presence of indications for prescribing meloxicam, according to in the opinion of the attending physician, the patient’s consent to participate.
Non-inclusion criteria:
contraindications for the use of NSAIDs, the presence of symptoms of severe threatening pathology (“red flags”), as well as severe functional impairment, which makes it difficult to re-observe patients.
Data obtained during 2 visits of patients were analyzed: at the 1st visit, a standard clinical examination and survey were carried out before prescribing therapy; at the 2nd visit, the result of therapy was assessed after 14 days.
The severity of LBP was assessed using a 10-point NRS according to the following criteria: 0 points—no pain, 10—maximum severe pain. General health was also assessed using the NRS, where: 0 points - no deterioration, 10 - the most pronounced deterioration in health. On average, the severity of pain at the time of treatment was 6.69±1.65 points, deterioration in health was 5.68±2.09 points. Severe pain (7 points or more) was recorded in 57.0% of patients.
When interviewing patients who had previously had episodes of NBS, they found out the fact of using NSAIDs and an assessment of their effect. As it turned out, the vast majority (70.2%) of patients had already received drugs from this group. The effectiveness of NSAIDs in history was rated by patients as good in 28.0% of cases, as moderate in 54.6% and low in 17.4%.
Many patients had a history of adverse reactions (ARs) when using NSAIDs: dyspepsia (gastralgia, nausea, feeling of heaviness in the epigastrium, etc.) - in 44.7% of patients, development of stomach and/or duodenal ulcers - in 2.7% %, bleeding from the gastrointestinal tract (GIT) - in 0.4%, increased blood pressure (BP) - in 14.1%, edema - in 6.2%, allergic reactions - in 3.4%.
In addition, a number of features of the clinical manifestations of acute NBS were analyzed. When surveying patients, the following symptoms were identified: persistence of pain at rest - in 37.2% of patients, pain at night - in 19.0%, feeling of stiffness in the morning or after being at rest - in 60.7%, pain radiating to the leg - in 28.2%, signs of lumbar ischialgia (intense pain in the leg, accompanied by sensory disturbances) - in 9.6%.
All patients were prescribed original meloxicam (Movalis) at a dose of 15 mg/day. In the majority of patients (86.1%), it was used in a stepwise manner: the first 3-5 days in the form of intramuscular (IM) injections, with a further transition to the oral form. In 13.9% of patients, only oral meloxicam was used. By decision of the attending physicians, 52.3% of patients also received muscle relaxants (tolperisone - 31.7%, tizanidine - 18.7%, baclofen - 1.7%), 17.4% - B vitamins (mainly for i.m. introduction). To prevent the development of NSAID gastropathy, 21.6% of patients were prescribed PPIs, mainly omeprazole.
The result of treatment was determined by the frequency of complete cessation of pain and the dynamics of its severity (if it did not go away completely), as well as the general well-being of patients over 2 weeks of observation. In addition to this, patients were asked to rate the result of therapy on a 5-point scale, where: 1 point meant deterioration of the condition, 5 - excellent result. The frequency and nature of ADRs recorded during the observation period were also studied.
The obtained quantitative data are presented as the mean value and standard error of the mean value ( M± m
).
Statistical differences in quantitative parameters were determined using t
-test; the distribution of rank variables was determined using the odds ratio (OR) and Fisher's exact test. Indicator O.Sh. is given in the paper along with the corresponding 95% confidence interval (CI).
Symptoms
The main symptom of intercostal neuralgia is severe pain in the chest along the nerve. As a rule, it occurs suddenly and resembles an electric shock, gradually spreading along the ribs. The nature of the sensations can be different: shooting, pulsating, constant, burning or dull.
Deep breathing, turning the head or body, bending, pressing or simply touching the chest causes a pronounced increase in pain. In addition, characteristic signs of neuralgia are:
- persistence of pain at night;
- the ability to determine the epicenter of pain;
- redness or paleness of the skin in the affected area;
- a feeling of tingling, crawling or, conversely, numbness along the affected nerve;
- slight muscle twitching in the affected area.
As a rule, during an attack of neuralgia, a person tries to lie or sit motionless in a position in which the pain becomes slightly less.
If the cause of the pain syndrome is herpes zoster, first redness appears on the skin along the affected nerve, then numerous blisters that burst, forming crusts. After recovery, increased pigmentation remains in this area for some time.
Differences from myocardial infarction
Chest pain, especially on the left, can be a consequence not only of intercostal neuralgia, but also of more serious problems. The most dangerous is myocardial infarction. This condition requires emergency medical attention. The characteristic differences in pain are:
- occurrence against the background of physical, less often psycho-emotional stress;
- spread to the left arm, shoulder, left half of the neck and lower jaw;
- no changes when turning the body, bending, pressing on the sore area;
- decreased intensity when taking nitroglycerin and its analogues.
A heart attack is often accompanied by cold, sticky sweat, pale skin, dizziness, and fear of death.
It is important to remember that the signs of a cardiovascular accident and intercostal neuralgia are not always so radically different. An accurate diagnosis can only be made by a doctor.
Treatment of intercostal neuralgia during pregnancy
During pregnancy, the presence of neuralgia is considered a fairly serious problem. It requires proper attention, which will help avoid complications for the expectant mother and baby.
All treatment that will be given to a pregnant woman for neuralgia must be prescribed by the attending physician. Self-therapy is extremely undesirable, as it can greatly harm the woman and the child in the womb.
Many patients prefer not to take medications. They limit themselves to vitamins and mineral complexes, use ointments and warm compresses, observe bed rest and perform simple physical exercises.
Gymnastics for neuralgic pain in pregnant women is very effective. Physical exercise does not allow blood to stagnate in the joints and parts of the spine.
If the pain becomes unbearable, novocaine blockades are prescribed with caution.
Diagnostics
Intercostal neuralgia, regardless of the severity of the pain syndrome and its location, requires a full diagnosis. The following examinations will help distinguish it from other pathologies:
- questioning and medical history: identifying the nature of the sensations, the conditions of their occurrence, the duration of the attack, concomitant diseases;
- examination and palpation: the doctor evaluates the appearance of the skin, checks the reaction to movements, pressing, turning, bending, assesses the severity of reflexes;
- laboratory diagnostics: general and biochemical blood tests, general urine tests: allows to identify signs of damage to the heart muscle (tests for troponins, CPK), inflammation, renal pathology, gastrointestinal diseases, etc.; the exact set of tests depends on the location of the source of pain;
- ECG, ultrasound of the heart: allow you to identify or exclude cardiovascular pathology;
- X-ray, CT or MRI of the thoracic spine: helps to identify osteochondrosis, osteoporosis, tumors, hernias and protrusions of intervertebral discs, etc.;
- Chest x-ray: allows you to assess the condition of the lung tissue and identify signs of tumors;
- Ultrasound of the kidneys, abdominal organs (excludes relevant pathology);
- FGDS to exclude pathologies of the esophagus, stomach, duodenum;
- myelography, contrast discography, electrospondylography to assess the condition of the spine, intervertebral discs, spinal cord and its roots.
If necessary, consultations with narrow specialists and additional examinations are prescribed.
Make an appointment
Diagnostic methods
You need to see a general practitioner. After examination and exclusion of other pathologies, the therapist refers to a neurologist who determines the symptoms and treats intercostal neuralgia. The doctor examines the images, prescribes tests and medical examinations.
Instrumental diagnostic methods of examination:
- Radiography. Allows you to examine the bone structure. Makes it possible to determine the presence of non-traumatic or traumatic disorders. X-rays are taken in direct, oblique and lateral projections.
- CT scan. Examines bone and muscle structure in combination. More often used to detect pathological changes in bone structures.
- Myelography. A contrast agent is injected into the spinal canal. This is the main method for diagnosing soft tissue structures (nerve roots and spinal cord).
- Contrasting discography. During the procedure, a contrast agent is injected into the intervertebral disc.
- Magnetic resonance imaging. Allows you to obtain images of organs and tissues. Detects pathological changes in soft tissue structures: nerve tissue, muscles, ligaments, hernias and degenerative changes in intervertebral hernias.
- Electrospondylography. Using the computer diagnostic method, it is possible to assess the condition of the spinal column, identify the disease at an early stage, determine the extent of damage and monitor the course of the disease.
Treatment
Intercostal neuralgia requires complex and often long-term treatment, including medication, physiotherapy, massage, etc.
Drug therapy
In the acute phase of the disease, therapy is aimed at relieving pain and improving the patient's condition. Depending on the specific clinical situation, the following are prescribed:
- non-steroidal anti-inflammatory drugs (NSAIDs): products based on diclofenac, nimesulide, ibuprofen, meloxicam and their derivatives; used in tablet, injection and local (creams, ointments, patches) form;
- analgesics: analgin and products based on it; like NSAIDs, they relieve pain;
- muscle relaxants to eliminate muscle spasms: mydocalm, etc.;
- group vitamins: milgamma, neuromultivitis, etc.; necessary to restore normal functioning of nerve fibers;
- sedatives to reduce the psycho-emotional component of pain and improve sleep.
If necessary, the following may additionally be prescribed:
- anticonvulsants: inhibit the passage of pain impulses;
- antidepressants to relieve tension;
- antihistamines and diuretics: relieve tissue swelling, especially relevant for pinched nerve roots;
- antiviral drugs for herpes zoster;
- glucocorticosteroids for persistent pain and severe inflammation that cannot be relieved by milder means.
Physiotherapy and exercise therapy
Physiotherapeutic procedures are prescribed after the acute pain subsides. Help speed up recovery:
- UHF;
- reflexology;
- magnetic therapy;
- electrophoresis;
- laser treatment;
- paraffin applications;
- mud therapy.
These procedures help improve blood circulation and metabolism in the affected area and accelerate the regeneration of nerve tissue.
Physical therapy exercises are prescribed after complete recovery. The main goal of gymnastics is to unload the back muscles. The complex is developed individually. The first classes should be carried out under the supervision of a specialist; in the future, home exercises are allowed.
Other treatments
Since very often the cause of intercostal neuralgia is pathology of the spine and spinal cord, the following are often used as additional methods of influence:
- acupuncture;
- manual therapy;
- therapeutic massage, including the use of warming agents;
- Shiatsu massage (acupressure);
- osteopathy;
- underwater traction and other techniques.
Like all medical procedures, these techniques are used only in a clinical setting and are carried out by specialists with medical education and the appropriate certificate.
Modern approach to the treatment of trigeminal neuralgia
Trigeminal neuralgia (TN) (synonyms: tic douloureux, or Fothergill's disease) is one of the most common facial pain (prosopalgia) and is one of the most persistent pain syndromes in clinical neurology [1]. TN is a typical example of neuropathic pain (NP) of a paroxysmal nature and is considered the most painful type of prosopalgia. TN most often has a chronic or recurrent course, is accompanied by a large number of comorbid disorders, is much more difficult to treat than many other types of chronic pain and leads to temporary or permanent disability, which makes it a major economic and social problem [2]. Chronic NP has a significant negative impact on the quality of life of patients, causing sleep disturbances, increased anxiety, depression, and decreased daily activity [3]. The high intensity and persistence of TN, its special, often painful nature, and resistance to traditional methods of pain relief give this problem exceptional relevance. Trigeminal neuralgia is a disease characterized by the occurrence of paroxysmal, usually unilateral, short-term, acute, sharp, intense, electric shock-like pain in the area of innervation of one or more branches of the trigeminal nerve [4, 5]. Most often, the lesion occurs in the zone of the II and/or III branch and extremely rarely - in the I branch n. trigeminus [6].
According to WHO, the prevalence of TN is up to 30–50 patients per 100,000 population, and the incidence is 2–4 people per 100,000 population. TN is more common in women than in men, debuts in the fifth decade of life and in 60% of cases has a right-sided localization [7, 8].
According to the International Classification of Headache Disorders (2nd edition), proposed by the International Headache Society (2003), TN is divided into classical, caused by compression of the trigeminal root by tortuous or pathologically altered vessels, without signs of obvious neurological deficit, and symptomatic, caused by proven structural damage to the trigeminal nerve, different from vascular compression [9].
The most common cause of TN is compression of the proximal part of the trigeminal root within a few millimeters of the entrance of the root into the pons (the so-called “root entry zone”). In approximately 80% of cases, compression occurs by an arterial vessel (most often a pathologically tortuous loop of the superior cerebellar artery). This explains the fact that TN occurs in old and senile age and practically does not occur in children. In other cases, such compression is caused by an aneurysm of the basilar artery, space-occupying processes in the posterior cranial fossa, tumors of the cerebellopontine angle and multiple sclerosis plaques [1, 8, 10, 11].
At the extracranial level, the main factors leading to the occurrence of TN are: tunnel syndrome - compression in the bone canal through which the nerve passes (usually in the infraorbital foramen and mandible), associated with its congenital narrowness, the addition of vascular diseases in old age, as well as as a result of a chronic inflammatory process in adjacent areas (caries, sinusitis); local odontogenic or rhinogenic inflammatory processes. The development of TN can be provoked by infectious processes, neuroendocrine and allergic diseases, demyelination of the trigeminal nerve root in multiple sclerosis [7, 12].
Depending on the impact of the pathological process on the corresponding part of the trigeminal system, TN is divided into predominantly central and peripheral genesis. In the occurrence of TN of central origin, neuroendocrine, immunological and vascular factors play an important role, which lead to impaired reactivity of cortical-subcortical structures and the formation of a focus of pathological activity in the central nervous system. In the pathogenesis of peripheral TN, a large role is played by the compression factor, infections, injuries, allergic reactions, and odontogenic processes [7, 8, 12].
Despite the large number of literature reviews and meta-analyses that have appeared in recent years on the problem of treating NB [13], which includes TN, there is no consensus among researchers regarding the basic principles of drug therapy for this disease [14]. Treatment of neuropathic pain is still insufficiently effective: less than half of patients experience significant improvement as a result of pharmacological treatment [15, 16].
The problem of treating trigeminal neuralgia today remains not fully resolved, which is associated with the heterogeneity of this disease in terms of etiology, pathogenetic mechanisms and symptoms, as well as the low effectiveness of conventional analgesics and the development of pharmacoresistant forms of TN that require surgical treatment. In modern conditions, treatment tactics for this disease include medicinal and surgical methods.
The main directions of drug therapy are: eliminating the cause of TN, if it is known (treatment of diseased teeth, inflammatory processes in adjacent areas, etc.), and carrying out symptomatic treatment (relief of pain).
Pathogenetic treatment of patients with TN includes the use of drugs with neurometabolic, neurotrophic, antioxidant, and antihypoxic effects. In recent years, the high effectiveness of the use of metabolic drugs in the complex treatment of NB has been discovered [8, 17]. In the treatment of patients with TN, the high effectiveness of the metabolic drug Actovegin, a deproteinized derivative from the blood of young calves, has been shown. The main effect of this drug is to stabilize the energy potential of cells by increasing intracellular transport and utilization of glucose and oxygen. Actovegin also has an antihypoxic effect, being an indirect antioxidant. In addition, the effect of Actovegin is manifested by indirect vasoactive and rheological effects by increasing capillary blood flow, reducing peripheral vascular resistance and improving the perfusion of organs and tissues [17]. Such a wide spectrum of pharmacological action of Actovegin allows its use in the treatment of TN. During an attack, it is advisable to use Actovegin intravenously in a slow stream or drip for 10 days at a dose of 400–600 mg/day. In the interictal period, the drug is prescribed orally at a dose of 200 mg 3 times a day for 1–3 months [8]. The pathogenetic treatment of patients with TN includes the use of high doses of B vitamins as part of multicomponent preparations, which is due to their multimodal neurotropic effect (impact on metabolism, metabolism of mediators, transmission of excitation in the nervous system), as well as the ability to significantly improve nerve regeneration. In addition, B vitamins have analgesic activity. Such drugs, in particular, include Milgamma, Neuromultivit, Neurobion, containing a balanced combination of thiamine (B1), pyridoxine (B6), cyanocobalamin (B12). Vitamin B1 eliminates acidosis, which reduces the pain threshold; activates ion channels in neuronal membranes, improves endoneurial blood flow, increases the energy supply of neurons and supports axoplasmic transport of proteins. These effects of thiamine promote nerve fiber regeneration [18–20]. Vitamin B6, by activating the synthesis of the myelin sheath of nerve fiber and transport proteins in axons, accelerates the process of regeneration of peripheral nerves, thereby exhibiting a neurotropic effect. Restoration of the synthesis of a number of mediators (serotonin, norepinephrine, dopamine, gamma-aminobutyric acid (GABA) and activation of descending inhibitory serotonergic pathways included in the antinociceptive system leads to a decrease in pain sensitivity (antinociceptive effect of pyridoxine) [18, 21]. Vitamin B12 is involved in processes of regeneration of nervous tissue, activating the synthesis of lipoproteins necessary for the construction of cell membranes and the myelin sheath; reduces the release of excitatory neurotransmitters (glutamate); has an antianemic, hematopoietic and metabolic effect [18, 22]. For rapid relief of pain and pathogenetic neurotropic effects in TN, it is advisable use of the parenteral form of the drug Neurobion - a combined preparation of B vitamins containing the optimal amount of vitamin B12 in both ampoule and tablet form. Neurobion is used in a dose of 3 ml per day intramuscularly 2-3 times a week - 10 injections (for severe pain syndrome can be used daily in the same dosage for 10–15 days). Then, to enhance and prolong the therapeutic effect and prevent relapse of the disease, Neurobion is prescribed in tablet form at a dosage of 1 tablet orally 3 times a day for 1–2 months [8].
Anticonvulsants are also the drugs of choice for the treatment of TN, and carbamazepine was one of the first drugs officially registered for the treatment of this condition [24].
In the early 90s of the last century, a new generation of antiepileptic drugs appeared, and now anticonvulsants are usually divided into first and second generation drugs.
First generation anticonvulsants include phenytoin, phenobarbital, primidone, ethosuximide, carbamazepine, valproic acid, diazepam, lorazepam, clonazepam. First-generation drugs are practically not considered as the first line of treatment for NB (with the exception of carbamazepine for TN) due to the insufficient level of analgesic effect and the high risk of adverse reactions. The most common side effects of first-generation anticonvulsants include: central nervous system reactions (drowsiness, dizziness, ataxia, sedation or increased excitability, diplopia, dysarthria, cognitive impairment, memory and mood impairment), hematological disorders (agranulocytosis, aplastic anemia, thrombocytopenia, leukopenia), hepatotoxicity, decreased bone mineral density, skin rashes, gingival hyperplasia, gastrointestinal symptoms (vomiting, anorexia). Second generation anticonvulsants include pregabalin (Lyrica), gabapentin (Neurontin, Gabagamma, Tebantin), lamotrigine (Lamictal), oxcarbazepine (Trileptal), topiramate (Topamax), levetiracetam (Keppra), tiagabine (Gabitril), zonisamide (Zonegran), vigabatrin (Sabril), felbamate (Taloxa). These drugs have more favorable pharmacokinetic characteristics and safety profiles, as well as a low risk of drug interactions compared to first-generation anticonvulsants [24, 25].
The main mechanisms of action of 1st and 2nd generation anticonvulsants are presented in table [26].
The first anticonvulsant successfully used to treat TN was phenytoin (Difenin) [27]. Diphenin, a derivative of hydantoin, similar in chemical structure to barbituric acid, is contraindicated in severe diseases of the kidneys, liver, and heart failure.
According to the recommendations of the European Federation of Neurological Societies (2009), pharmacotherapy for TN is based primarily on the use of carbamazepine (Finlepsin, Tegretol) proposed by S. Blum in 1962 (200–1200 mg/day), which is the drug of first choice (level of evidence A) [27, 28]. The analgesic effect of this drug is mainly due to its ability to reduce the permeability to sodium of the membranes of neurons involved in nociceptive reactions. The following treatment regimen with carbamazepine is usually prescribed. In the first two days, the daily dose is 200 mg (1/2 tablet in the morning and evening), then within two days the daily dose is increased to 400 mg (morning and evening), and after that - to 600 mg (1 tablet in the morning, at lunchtime and in the evening). If the effect is insufficient, then the total amount of the drug per day can be increased to 800–1000 mg. In some patients with TN (about 15% of the population), carbamazepine does not have an analgesic effect, so in such cases another anticonvulsant, phenytoin, is used.
Three placebo-controlled studies conducted about 40 years ago, which included a total of 150 patients with TN, showed the effectiveness of carbamazepine on both the frequency and intensity of paroxysms [24]. A number of authors have shown that carbamazepine can reduce pain symptoms in approximately 70% of cases. [29]. However, the use of carbamazepine is limited by pharmacokinetic factors and occasional severe side effects (for example, Stevens-Johnson syndrome), especially in elderly patients.
Oxcarbazepine (Trileptal) is structurally similar to carbamazepine, but is much better tolerated by patients and has far fewer side effects. Typically, oxcarbazepine is used at the beginning of treatment for TN at a dose of 600–1800 mg/day (Evidence Level B) [30].
As additional therapy for TN, the effectiveness of lamotrigine (Lamictal) at a dose of 400 mg/day [31] and baclofen at a dose of 40–80 mg/day [32], which are second-line drugs, has been shown (level of evidence: C). Small open studies (class IV) indicate the effectiveness of clonazepam, valproate, and phenytoin [33, 34]. This therapy is most effective in the classical form of TN. For TN of peripheral origin, it is preferable to include non-narcotic analgesics in treatment regimens, and in the case of the development of chronic pain syndrome (more than three months), the prescription of antidepressants (amitriptyline) is indicated [7, 12].
Gabapentin (Neurontin) is the first drug in the world to be registered for the treatment of all types of neuropathic pain. Many studies have shown the effectiveness of gabapentin in patients with TN who do not respond to treatment with other drugs (carbamazepine, phenytoin, valproate, amitriptyline); in most cases, complete relief of pain was observed [35]. The therapeutic dose ranges from 1800 to 3600 mg/day. The drug is taken 3 times a day according to the following regimen: 1st week - 900 mg/day, 2nd week - 1800 mg/day, 3rd week - 2400 mg/day, 4th week - 3600 mg/day.
The results of an open-label, prospective, 12-month study of 53 patients with TN were recently published, evaluating the effectiveness of pregabalin (Lyrica) at a dose of 150–600 mg/day. Treatment with pregabalin resulted in pain relief or at least a 50% reduction in pain intensity in 25% and 49% of patients, respectively [36]. In another multicenter, prospective, 12-week study of 65 patients refractory to prior analgesic therapy, treatment with pregabalin at a mean dose of 196 mg/day (monotherapy subgroup) and 234 mg/day (polytherapy subgroup) resulted in a ≥50% reduction in pain intensity in on average in 60% of patients, and also reduced the severity of anxiety, depression and sleep disorders [37]. When treating TN, the initial dose of pregabalin can be 150 mg/day in 2 divided doses. Depending on the effect and tolerability, the dose can be increased to 300 mg/day after 3–7 days. If necessary, you can increase the dose to the maximum (600 mg/day) after a 7-day interval.
The use of levetiracetam (Keppra) in the treatment of TN was first reported in 2004 by KR Edwards et al. [38]. The mechanism of action of levetiracetam is unknown; There is evidence obtained from animal experiments that it is a selective blocker of N-type calcium channels [39]. The properties of this drug are particularly suitable for the treatment of TN patients with severe pain who require a rapid response to therapy. The pharmacokinetics of levetiracetam are linear and predictable; Plasma concentrations increase proportionally to the dose within the clinically reasonable range of 500 to 5000 mg [40]. Unlike other anticonvulsants, especially carbamazepine, the hepatic cytochrome P450 system is not involved in the metabolism of levetiracetam and the drug is excreted through the kidneys [41]. In addition, this drug is characterized by a favorable therapeutic index and has a small number of adverse side effects (which is the main problem when using drugs to treat TN) [42]. Commonly reported side effects of levetiracetam are asthenia, dizziness, drowsiness, headache and depression. A 10-week, prospective, open-label study showed that higher doses of levetiracetam, ranging from 3000–5000 mg/day (50–60 mg/kg/day), were required for the treatment of TN compared with the treatment of epilepsy, but did not caused significant side effects. This circumstance indicates the prospect of using this drug for the treatment of TN [43].
One domestic study reported positive results with a combination of carbamazepine and gabapentin [44].
Since the 1970s, antidepressants have been used to treat TN [45]. Currently, the effectiveness of the use of tricyclic antidepressants (TCAs) in the treatment of TN has been proven [46].
Until now, the selection of analgesic therapy for NB is more an art than a science, since the choice of drugs is carried out mainly empirically. There are often situations when the use of one drug is not effective enough and there is a need for a combination of drugs. Prescribing “rational polypharmacotherapy” (simultaneous use of drugs with neurotropic, neurometabolic and analgesic mechanisms of action) allows increasing the effectiveness of treatment with lower dosages of drugs and fewer side effects [47].
For patients suffering from unbearable pain for a long time, and if conservative therapy is ineffective in the case of classical TN, surgical treatment is recommended. The following approaches are currently used:
1) surgical microvascular decompression [48]; 2) stereotactic radiation therapy, gamma knife [49]; 3) percutaneous balloon microcompression [50]; 4) percutaneous glycerol rhizolysis [51]; 5) percutaneous radiofrequency treatment of the Gasserian node [52].
The most effective method of surgical treatment of TN is the P. Janetta method, which consists of placing a special gasket between the trigeminal nerve and the irritating vessel; in the long-term period, the effectiveness of treatment is 80% [53–55].
In conclusion, we note that the treatment of TN should be multidisciplinary in nature, and the choice of various treatment methods and the risks of possible complications should be discussed with the patient.
Literature
- Karlov V. A. Neurology of the face. M.: Medicine, 1991. 288 p.
- O'Connor AB Neuropathic pain: quality-of-life impact, costs and cost effectiveness of therapy // Pharmacoeconomics. 2009. Vol. 27, No. 2. P. 95–112.
- Jensen MP, Chodroff MJ, Dworkin RH The impact of neuropathic pain on health-related quality of life: review and implications // Neurology. 2007. Vol. 68. P. 1178–1182.
- Pain syndromes in neurological practice. Ed. A. M. Veina. M.: MEDpress-inform, 2001. 368 p.
- Love S., Coakham HB Trigeminal neuralgia: pathology and pathogenesis // Brain. 2001. Vol. 124, No. 12. P. 2347–2360.
- Turbina L. G., Gordeev S. A., Zusman A. A. Trigeminal neuralgia. Epidemiology, pathogenesis, clinic, diagnosis, treatment // Collection of works of the Moscow Regional Association of Neurologists “World Stroke Day in the Moscow Region October 29, 2009”: Collection. articles. M., 2009. pp. 65–70.
- Gritsai N. N., Kobzistaya N. A. Classical trigeminal neuralgia and odontogenic pain syndrome // News of medicine and formation. 2009. No. 299. pp. 23–25.
- Tovazhnyanskaya E. L. Trigeminal neuralgia: modern aspects of complex therapy // International. neurol. magazine 2010. No. 3 (33). pp. 141–145.
- International classification of headaches. 2nd edition. M.: GlaxoSmithKline Trading, 2003. 380 p.
- Kress B., Schindler M., Rasche D. MRI volumetry for the preoperative diagnosis of trigeminal neuralgia // Eur. Radiol. 2005. Vol. 15. P. 1344–1348.
- Rasche D., Kress B., Stippich C. et al. Volumetric measurement of the pontomesencephalic cistern in patients with trigeminal neuralgia and healthy controls // Neurosurgery. 2006. Vol. 59. P. 614–620.
- Stepanchenko A.V. Typical trigeminal neuralgia. M.: Publishing house. Group "VHM", 1994. 39 p.
- Saarto T., Wiffen PJ Antidepressants for neuropathic pain // Cochrane Database Syst. Rev. 2007. Vol. 4:CD005454.
- Chong MS, Bajwa ZH Diagnosis and treatment of neuropathic pain // J. Pain Symptom Manage. 2003. Bd. 25. (Suppl. 5). S. 4–11.
- Dworkin RH, Backonja M, Rowbotham MC et al. Advances in neuropathic pain: diagnosis, mechanism, and treatment recommendation // Arch. Neurol. 2003. Vol. 60. P. 1524–1534.
- Finnerup NB, Otto M, McQuay HJ et al. Algorithm for neuropathic pain treatment: an evidence based proposal // Pain. 2005. Vol. 118, No. 3. P. 289–305.
- Ametov A. S., Dadaeva E. E., Strokov I. A. et al. Actovegin in the treatment of diseases of the central and peripheral nervous system // Rus. honey. magazine 2007. T. 15, No. 24. pp. 1824–1827.
- Lutsky I. S., Lyutikova L. V., Lutsky E. I. B vitamins in neurological practice // International. neurol. magazine 2008. No. 2. pp. 89–93.
- Ba A. Metabolic and structural role of thiamine in nervous tissues // Cell. Mol. Neurobiol. 2008. Vol. 28. P. 923–931.
- Gibson GE, Blass JT Thiamin-dependent processes and treatment strategies in neurodegeneration // Antioxid. Redox Signal. 2007. Vol. 9. P. 1605–1619.
- Wilson RG, Davis RE Clinical chemistry of vitamin B6 // Adv. Clin. Chem. 1983. Vol. 23. P. 1–68.
- Solomon LR Disorders of cobalamin (vitamin B12) metabolism: emerging concept in pathophysiology, diagnosis and treatment // Blood Rev. 2007. Vol. 21. P. 113–130.
- Trigeminal neuralgia. Internet review // Int. neurol. magazine 2010. No. 2 (32). pp. 103–104.
- Wiffen PJ, McQuay HJ, Moore RA Carbamazepine for acute and chronic pain. Cochrane Database Syst. Rev. 2005. Vol. 3:CD005451.
- Richter RW, Portenoy R, Sharma U et al. Relief of diabetic peripheral neuropathy with pregabalin: a randomized placebo-controlled trial // J. Pain. 2005. Vol. 6. P. 253–260.
- Kukushkin M. L. Neurogenic (Neuropathic pain) // International. neurol. magazine 2007. No. 2 (12). pp. 141–145.
- Sindrup SH, Jensen TS Pharmacotherapy of trigeminal neuralgia // Clin. J. Pain. 2002. Vol. 18. P. 22–27.
- Jorns TP, Zakrzewska JM Evidence-based approach to the medical management of trigeminal neuralgia // Br. J. Neurosurg. 2007. Vol. 21. P. 253–61.
- Gronseth G., Cruccu G., Alksne J. et al. Practice parameter: the diagnostic evaluation and treatment of trigeminal neuralgia (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the European Federation of Neurological Societies // Neurology. 2008. Vol. 71. P. 1183–1190.
- Jensen TS Anticonvulsants in neuropathic pain: rationale and clinical evidence // European Journal of Pain. 2002. Vol. 6 (Suppl. A). P. 61–68.
- Zakrzewska JM, Chaudhry Z., Nurmikko TJ et al. Lamotrigine (lamictal) in refractory trigeminal neuralgia: results from a double-blind placebo controlled crossover trial // Pain. 1997. Vol. 73. P. 223–230.
- Fromm GH, Terrence CF Comparison of L-baclofen and racemic baclofen in trigeminal neuralgia // Neurology. 1987. Vol. 37. P. 1725–1728.
- Kamchatov P.V. Neuropathic pain: problems and solutions // NeuroNEWS. 2009. No. 4. pp. 45–47.
- Attal N., Cruccu G., Haanpaa M. et al. EFNS guidelines on pharmacological treatment of neuropathic pain // European Journal of Neurology. 2006. Vol. 13. P. 1153–1169.
- Cheshire W. Defining the role for gabapentin in the treatment of trigeminal neuralgia: a retrospective study // J. Pain. 2002. Vol. 3. P. 137–142.
- Obermann M., Yoon MS, Sensen K. et al. Efficacy of pregabalin in the treatment of trigeminal neuralgia // Cephalalgia. 2008. Vol. 28. P. 174–181.
- Perez C., Navarro A., Saldana MT et al. Patient-reported outcomes in subjects with painful trigeminal neuralgia receiving pregabalin: evidence from medical practice in primary care settings // Cephalalgia. 2009. Vol. 29. P. 781–790.
- Edwards KR, O'Connor JT, Button J. Levetiracetam for the treatment of trigeminal neuralgia // Epilepsia. 2004. Vol. 45 (Suppl. 7). P. 306.
- Lukyanetz EA, Shkryl VM, Kostyuk PG Selective blockade of N-type calcium channels by levetiracetam // Epilepsia. 2002. Vol. 43. P. 9–18.
- Patsalos PN Pharmacokinetic profile of levetiracetam: towards ideal characteristics // Pharmacol. Ther. 2000. Vol. 85. P. 77–85.
- Brockmoller J., Thomsen T., Wittstock M. et al. Pharmacokinetics of levetiracetam in patients with moderate to severe liver cirrhosis (Child-Pugh classes A, B, and C): characterization by dynamic liver function tests // Clin. Pharmacol. Ther. 2005. Vol. 77. P. 529–541.
- Zakrzewska JM Consumer views on management of trigeminal neuralgia // Headache. 2001. Vol. 41. P. 369–376.
- Jorns TP, Johnston A., Zakrzewska JM Pilot study to evaluate the efficacy and tolerability of levetiracetam (Keppra®) in the treatment of patients with trigeminal neuralgia // European Journal of Neurology. 2009. Vol. 16. P. 740–744.
- Stepanchenko A.V., Sharov M.N. Use of gabapentin in the treatment of exacerbations of trigeminal neuralgia // Pain. 2005. T. 3, no. 8. pp. 58–61.
- Braune S. Evidence-based pharmacotherapy of neuropathic pain syndromes // MMW Fortschr. Med. 2004. Vol. 146, No. 50. P. 49–51.
- Cruccu G. Treatment of painful neuropathy // Curr. Opin. Neurol. 2007. Vol. 20, No. 5. P. 531–535.
- Hall GC, Carroll D., Parry D., McQuay HJ Epidemiology and treatment of neuropathic pain: The UK primary care perspective // Pain. 2006. Vol. 122. P. 156–162.
- Janetta P. Trigeminal neuralgia: treatment by microvascular decompression // Neurosurgery/Eds. Wilkins R., Regachary S. New York: McGrawy-Hill, 1996. P. 3961–3968.
- Perez C., Galvez R., Huelbes S. et al. Validity and reliability of the Spanish version of the DN4 (Douleur Neuropathique 4 questions) questionnaire for differential diagnosis of pain syndromes associated to a neuropathic or somatic component // Health Qual Life Outcomes. 2007. Vol. 5. P. 66.
- Mullan S., Lichtor T. Percutaneous microcompression of the trigeminal ganglion for trigeminal neuralgia // J. Neurosurg. 1983. Vol. 59. P. 1007–1012.
- Hakanson S. Trigeminal neuralgia treated by the injection of glycerol into the trigeminal cistern // Neurosurgery. 1981. Vol. 9. P. 638–646.
- Sweet WH, Wepsic JG Controlled thermocoagulation of trigeminal ganglion and root for differential destruction of pain fibers. Part I: trigeminal neuralgia // J. Neurosurg. 1974. Vol. 39. P. 143–156.
- Barker FG, Jannetta PJ, Bissonette DJ et al. The long-term outcome of microvascular decompression for trigeminal neuralgia // N. Engl. J. Med. 1996. Vol. 334. P. 1077–1083.
- Tyler-Kabara EC, Kassam AB, Horowitz MH et al. Predictors of outcome in surgically managed patients with typical and atypical trigeminal neuralgia: Comparison of results following microvascular decompression // J. Neurosurg. 2002. Vol. 96. P. 527–531.
- Jannetta PJ Microsurgical management of trigeminal neuralgia // Arch. Neurol. 1985. Vol. 42. P. 800.
S. A. Gordeev*, Doctor of Medical Sciences L. G. Turbina**, Doctor of Medical Sciences, Professor A. A. Zusman**, Candidate of Medical Sciences *First Moscow State Medical University named after. I. M. Sechenov, **MONIKI im. M. F. Vladimirsky, Moscow
Contact information for authors for correspondence
Complications
Complications of intercostal neuralgia occur quite rarely, however, in severe cases, without appropriate treatment, the patient may encounter the following problems:
- severe spasm of the respiratory muscles, limiting inhalation and exhalation;
- inability to get out of bed due to significant increase in pain;
- excessive pain syndrome that is not relieved by conventional analgesics and NSAIDs;
- heart rhythm disturbances due to muscle spasms and nerve pathology;
- decreased leg mobility.
In addition, complications can be caused by attempts to be treated outside the clinic. Abscesses and cellulitis after acupuncture, paralysis and decreased sensitivity after manual therapy are not a complete list of problems. That is why you should not treat intercostal neuralgia either independently or with the help of dubious specialists.
Prevention
Prevention of intercostal neuralgia is mainly general measures aimed at strengthening the muscle frame and improving the health of the body. Neurologists recommend:
- lead an active lifestyle, play sports at an amateur level;
- minimize hypothermia and colds;
- watch your posture;
- avoid lifting heavy objects;
- maintain a high level of immunity;
- eat a balanced diet, if necessary, take additional vitamins, especially group B;
- treat chronic diseases in a timely manner;
- avoid stress, get proper rest and ensure yourself at least 8 hours of sleep every night.
Following these simple rules will significantly reduce the risk of developing intercostal neuralgia.
Prevention of intercostal neuralgia
The main preventive measure is gymnastics. It is necessary to perform exercises that promote muscle development, strengthening and mobility of the spine. Avoid drafts, uncomfortable positions and excessive physical activity. Everything should be in moderation.
It is important to control your posture, not lift excessive weights, eat a rational and balanced diet, take vitamins, and avoid fasting and mono-diet.
Do not forget to promptly treat diseases that can cause the development of neuralgia.
Treatment at the Energy of Health clinic
Doctors at the Energy of Health clinic will always come to the aid of patients with intercostal neuralgia. We offer each client:
- a full examination with consultations with specialists for an accurate diagnosis;
- individual selection of treatment regimen;
- services of a qualified chiropractor;
- own exercise therapy room for the most effective and safe exercises;
- modern methods of physiotherapy;
- massotherapy;
- drug blockades for severe pain syndrome.
Regular observation by a neurologist after the acute period of the disease has subsided will help prevent recurrent attacks.
Advantages of the clinic
In the neurology department of the Energy of Health clinic, every patient receives the highest level of specialists and modern equipment for diagnosing and treating diseases. We take an integrated approach to therapy and use not only medications, but also physiotherapy, exercise therapy and massage.
Treatment is prescribed only after a thorough examination and is monitored by a specialist until the patients fully recover. Adequate prices, convenient location, private parking - we do everything for the convenience of our clients.
If intercostal neuralgia interferes with living, walking and moving, do not delay treatment. Sign up for the Health Energy clinic and get rid of pain.
Epidural administration of anesthetics and steroid hormones
Spinal epidural block involves the injection of drugs into the epidural space, which leads to loss of sensation in the area of impact. This means that this procedure involves introducing the active substance directly into the source of pain. Achieving a therapeutic effect in this case is possible due to the following factors:
- analgesic properties of the drug;
- the maximum possible concentration in the affected area;
- reflex action at all levels of the nervous system.