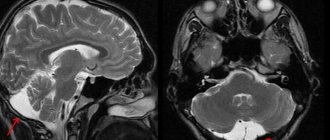
Magnetic resonance imaging has high tissue and fluid contrast. The procedure allows visualization of loose structures of the body without significant invasive manipulations. MRI is actively used in neurology and neurosurgery to diagnose diseases of the nervous system. Magnetic resonance scanning is considered the most informative method of studying the brain. According to the results of tomography, inflammatory, degenerative, dystrophic changes, and tumors are detected.
Colloid cyst on MRI
A brain cyst is a benign neoplasm inside the skull. It is a closed pathological formation with predominantly liquid contents. Congenital cysts appear when intrauterine development is disrupted; acquired ones can be the result of head trauma, infectious disease, cerebrovascular accidents and other conditions. The formations are not prone to malignant degeneration, but when they reach an impressive size they can compress surrounding structures. It is important to diagnose a cyst as early as possible and determine treatment tactics. MRI scanning allows you to identify and differentiate formations and track the dynamics of the process.
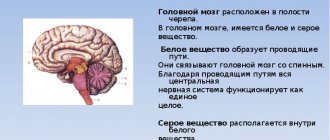
1.Cysts of the brain
Brain cysts
– common benign neoplasms, which are a rounded cavity filled with liquid contents. The reasons why cysts occur can be very diverse.
A considerable part of cysts are congenital, some are formed as a result of previous injuries, sometimes even in the distant past. Such brain tumors can also be the result of inflammatory processes, hemorrhages, circulatory disorders and dystrophic-degenerative changes in the brain.
Cysts are localized between the membranes of the brain (arachnoid) and directly in the tissues of the brain, in its depths.
A must read! Help with treatment and hospitalization!
Types of epidermal cysts
Doctors distinguish several types of formations. Classification is carried out according to structure, symptoms and the presence of complications.
The most common diagnosis is atheroma. This formation is localized in the face, arms, neck and scrotum. A single atheroma may appear on the skin or several may appear at once.
This type of epidermal cyst, such as atheroma, has a round shape and soft contents. As a rule, this formation is yellow or red in color.
Atheroma does not bother a person; it can remain the same size or rise slightly above the skin.
When an infection occurs, the formation suppurates and leads to inflammation of neighboring tissues.
2.Types of brain cysts
Cysts can be formed by various types of cellular structures, and depending on this they are divided into the following types:
- arachnoid;
- pineal;
- colloidal;
- dermoid;
- epidermoid (cholesteatomas).
With the exception of arachnoid cysts, which were already mentioned above, all others are classified as intracerebral.
Epidermoid and dermoid cysts
consist of epithelial cells that, due to certain processes, ended up in the wrong place, but got inside other tissue masses. This may be a consequence of embryogenesis disorders (congenital cysts), or the result of injuries when epidermal cells enter tissues located deep in the brain (acquired cysts).
Dermoid cysts
characterized by the presence of various dermal inclusions - fat and sweat glands, hair follicles, etc.
Most of these cysts are found in the following parts of the brain:
- pontocerebellar ganglion (MCG);
- chiasmal-sellar region (CHS);
- ventricular cavity;
- cerebellum;
- brain stem.
Visit our Neurosurgery page
How is an epidermal cyst treated?
The formation must be removed through surgery. However, there are some restrictions. If it is close to parts of the brain, then complete excision is impossible. The neurosurgeon will perform only partial removal and recommends annual examinations for timely diagnosis of relapses.
When the formation is malignant, it is treated by an oncologist surgeon. Usually the tactic of simultaneous radiation and chemotherapy is chosen. If atheroma is diagnosed, the size of the tumor plays an important role. Small formations can be left without treatment, but only observed. When the tumor begins to grow, excision under local anesthesia is indicated.
The operation to excise a superficial epidermal cyst usually lasts no more than 20 minutes. The doctor makes an incision and removes the cyst along with the capsule. Then the cavity is scraped, the skin is cleaned and the wound is sutured.
If relapse occurs, repeat surgery is recommended.
3. Symptoms of a brain cyst
Small cysts are asymptomatic and can be accidentally detected during examination. When the tumor reaches a large size, the symptoms that appear depend on its location. Among the most characteristic symptoms are:
- headache, dizziness;
- feeling of fullness in the head;
- auditory and visual impairments;
- convulsions, paralysis of limbs;
- epileptic seizures;
- impaired coordination of movements;
- fainting, hallucinations;
- sleep disorders.
About our clinic Chistye Prudy metro station Medintercom page!
Why does an epidermal cyst form?
The formation appears as a result of the closure of the passage of the hair follicle with excess sebum production and horny cells.
Externally, the cyst resembles a ball up to 5 cm in diameter, is pink in color and covered with a network of small vessels. Often, her pores darken and expand.
The internal contents of the cyst resemble a yellow paste.
Getting an infection inside a cystic formation can cause inflammation, enlargement, and pain.
If the formation is localized on the head, then as it increases it can put pressure on the brain. And this, in turn, provokes blurred vision, severe headaches, and mental disorders. It is not uncommon for an epidermal cyst to provoke
4.Basic treatment methods
As a rule, cysts that do not show a tendency to grow do not require treatment at all. Otherwise, treatment of neoplasms is carried out surgically. It could be:
- transcranial surgery, which provides high efficiency of cystectomy, but is traumatic for the patient;
- shunting the cyst to evacuate the liquid contents, after which its walls collapse;
- gentle endoscopic surgery using special equipment.
Diagnosis and treatment of arachnoid cyst
Cysts that occur without any manifestations can only be detected by chance. In the case of neurological manifestations, the doctor first analyzes the patient’s complaints. However, the manifestations can only indicate that there are some malfunctions in the functioning of the brain, but do not allow us to classify the problem. Hematomas, brain tumors, cysts located inside the brain have the same symptoms. For a more accurate diagnosis, the doctor may prescribe electroencephalography, echoencephalography or rheoencephalography. The disadvantage of these methods is that they do not provide information about the exact location of the formation or its nature.
The main goal of any treatment for an arachnoid cyst is to drain fluid and reduce pressure on brain tissue.
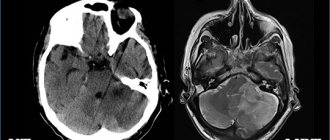
Today, the most accurate diagnostic method, which allows a high degree of accuracy to distinguish an arachnoid cyst from a tumor or hematoma, is computed tomography (CT) and magnetic resonance imaging (MRI).
This can be achieved by various methods including:
- Shunting. With this method, the surgeon installs a tube (shunt) into the cyst through which fluid is drained to other parts of the body (for example, the abdominal cavity), where it is absorbed by other tissues.
- Fenestration. In this case, holes are created in the patient's skull and the walls of the cyst to drain and ensure normal flow of cerebrospinal fluid.
- Needle aspiration and connection using holes of the inner part of the cyst with the subarachnoid space to drain fluid into it.
Epidemiology
The mean age was 58 years (range 24–86 years); the majority (69%) were women [2]. Small VR spaces (<2 mm) are detected in all age groups. With age, VR spaces are found with greater frequency and larger size (> 2 mm) [1]. Some studies have found a correlation between expanded VR spaces and neuropsychiatric disorders [1], multiple sclerosis [1], mild traumatic brain injury [1], and diseases associated with microangiopathy [1].
Sources
- "Virchow-Robin Spaces at MR Imaging." Robert M. Kwee, Thomas C. Kwee link
- "Large anterior temporal Virchow-Robin spaces: unique MR imaging features." Lim AT1, Chandra RV, Trost NM, McKelvie PA, Stuckey SL. link
- "Virchow-Robin spaces at MR imaging." Kwee RM1, Kwee TC. link
Author: radiologist, Ph.D. Vlasov Evgeniy Alexandrovich
Full or partial reprint of this article is permitted by installing an active hyperlink to the source
If you still have doubts about the conclusions of your MRI, you can order a review of your study with a detailed transcript here:
MRI
Manifestations on MRI are similar to those on CT; epidermoids are often indistinguishable from arachnoid cysts or dilated CSF spaces on many sequences.
- T1 is usually isointense to cerebrospinal fluid
- a more intense signal is often observed compared to the cerebrospinal fluid along the periphery of the formation
- may rarely have a hyperintense signal (“white epidermoids”)
- Rarely, internal hemorrhage may result in increased signal intensity
- sometimes there may be a subtle accumulation of contrast around the periphery
- usually isointense to cerebrospinal fluid (65%)
- usually inhomogeneous/dirty signal; higher than from cerebrospinal fluid
CT
The combination of cellular debris together with the high cholesterol content reduces the density of the epidermoids to approximately 0 HU; thus, epidermoid cysts may be identical in density to the cerebrospinal fluid, and appear the same as arachnoid cysts.
Calcification is uncommon (10-25% of cases); Rarely, an epidermoid cyst may be hyperdense due to bleeding, saponification, or high protein content (“white epidermoids”).
They do not accumulate contrast, and only in very rare cases show accumulation of contrast by the wall.
They can cause bone erosion, and with an intradiploic location they have a pronounced sclerotic rim along the edges of the cyst [2].
MRI diagnostics for arachnoid cyst
Despite the fact that CT allows you to accurately determine the size and location of the cyst, MRI provides the most accurate and complete information about the formation. Typically, to diagnose an arachnoid cyst, an MRI scan is performed with the injection of contrast into the patient's bloodstream. At the same time, brain tumors tend to accumulate contrast, and cysts do not absorb it from the blood vessels, which is very clearly visible on MRI.
Also, MRI scanning allows you to distinguish a cyst from hemorrhages, hematomas, hygromas, abscesses and other diseases with similar symptoms. In addition, MRI makes it possible to identify a cyst even in cases where the patient does not yet have any symptoms, and the cyst itself measures only a few millimeters.
Get an MRI of the brain in St. Petersburg
Prevention
To reduce the risk of cyst formation in newborns, women during pregnancy should follow a number of preventive measures. Experts recommend:
- Stop drinking alcohol and smoking. Carcinogenic substances contained in drinks and tobacco smoke negatively affect the body and the process of fetal formation.
- Walk outdoors every day
- properly . The diet must include vegetables and fruits.
- Treat infectious diseases in a timely manner. They cause the formation of cysts in the child’s brain.
- Avoid stress, neurosis and depression.
- Avoid heavy physical activity.
- Visit your obstetrician-gynecologist regularly. The specialist will prescribe the necessary research methods, which will allow timely detection of the presence of a cyst.
Women should also visit a doctor and undergo an examination before becoming pregnant. This will identify certain disorders and prevent the formation of a cyst in the child’s head in the future.
Compliance with preventive measures helps to significantly reduce the likelihood of developing the disease and eliminate the occurrence of serious consequences.
Cysts that affect brain structures are benign. But the danger of the pathology lies in the high risk of certain complications and degeneration of the formation into a malignant tumor. That is why, if a newborn is diagnosed with a cyst in the head, parents should pay special attention to the diagnosis and follow all the doctor’s recommendations.
It is important to remember that drug treatment or surgery are not always prescribed. If the formation does not increase, therapy is not carried out. The disease does not affect life expectancy. In this case, you must follow the doctor's recommendations.
"Scary" names
What is a cyst? A cyst (its other name is “cerebrospinal fluid cyst”) is a cavity filled with liquid, having a capsule that isolates it from other liquor-containing spaces.
Most often, parents of children who have been diagnosed with a retrocerebellar cyst
. And although this phrase frightens and even makes parents panic, it must be said that with these words radiologists describe a variant of the norm. Most often, this is not a cyst at all (that is, not an isolated cavity filled with fluid), and it does not require surgical treatment.
Children under two years of age diagnosed with a retrocerebellar cyst should be shown to a neurosurgeon to avoid the development of hydrocephalus.
Another normal variant is a pineal gland cyst.
. Perhaps the most common incidental finding on MRI. Does not require surgical treatment.
Epidermoid or dermoid cyst
– this is not a real cyst. It is filled not with liquid, but with skin appendages - follicles, sebaceous glands, hair, cartilage tissue, etc. In its structure, it is more similar to a tumor and requires the same treatment as for a tumor - removal.
Porencephalic cyst
usually occurs in the place where part of the brain has died as a result of hypoxia or hemorrhage; this place is filled with fluid. In itself, such a cyst does not interfere with development and does not require mandatory surgical treatment.
Pseudocyst
- looks like a cyst, but not a cyst, a cavity that is not limited by anything, it has communication with other parts of the skull. Does not require surgical treatment.
Septum pellucida cyst
in the vast majority of cases it is a variant of the norm, but if it is large in size, it can lead to impaired cerebrospinal fluid circulation, which requires surgical treatment.
For children in whom the cerebrospinal fluid cyst rapidly enlarges, causes increased intracranial pressure, neurological symptoms or seizures, surgical treatment is indicated.
If your child has a photo taken and a cyst is found, don’t panic! Having received a description of the x-ray image, first of all, pay attention to the conclusion. If the report says: “There are no pathological abnormalities,” most likely you will not need any surgical intervention. Even if you see the word “cyst” somewhere, most likely the radiologist needed it to describe a normal condition. Just in case, check with him whether you need a consultation with a neurosurgeon.
Diagnostics
The basis for verifying the diagnosis are:
- data from a visual medical examination or examination by specialized specialists (urologist, neurologist, etc.);
- Ultrasound (detects a cavity formation with smooth contours, clarifies its size);
- CT/MRI (studies are informative for rare localizations of epidermal cysts);
- histological examination (reveals a thinned epidermis without other skin appendages on the inner surface of the cyst and horny scales inside it, which sometimes become calcified).
Morphology
VR spaces surround the walls of blood vessels and extend from the subarachnoid space through the brain parenchyma. Small VR spaces are popping up across all age groups. With age, VR spaces are found with greater frequency and larger apparent sizes. Upon visual analysis, the signal intensity of the VR spaces is identical to the intensity of the cerebrospinal fluid in all sequences [3].
There are three types of VR spaces:
- Type I VR spaces appear along the lenticulospiral arteries entering the basal ganglia through the anterior perforated substance [3].
- Type II VR spaces are found along the paths of perforating medullary arteries as they enter the cortical gray matter along high bulges and extend into the white matter [3].
- Type III VR spaces appear in the midbrain [3].
Fig.2 Perevascular spaces of type I VR.
Fig. 3 Perevascular spaces of type II VR.
Fig.4 Perevascular spaces of type III VR.
From time to time, VR spaces have an atypical appearance. They can become very large, predominantly involve one hemisphere, take on bizarre shapes, and even have a mass effect. Knowing the signal intensity characteristics and location of VR spaces helps to distinguish them from various pathological conditions [3].
The arteries in the cerebral cortex are covered with a layer of leptomeningocytes, which are lined with the pial membrane; With this anatomical arrangement, the spaces of the intracortical arteries are in direct communication with the spaces of the VR around these arteries in the subarachnoid space [1].
Fig. 5 Multiple cystic-dilated pervascular Virchow-Robin spaces in the white matter of both hemispheres of the cerebrum.
The expansion of RV spaces was described by Durant-Fardel [1] in 1843. The expansions of the perivascular spaces are regular cavities that always contain the patent artery. The mechanisms underlying the expansion of VR spaces are still unknown. Various theories have been put forward: segmental necrotizing arterial angitis or another unknown condition causing permeability of the arterial wall [1], dilation of the ER spaces resulting from disruption of the circulation of interstitial cerebrospinal fluid drainage pathways in the cisterns [1], spiral elongation of blood vessels and brain atrophy, resulting from an extensive network of tunnels filled with extracellular fluid [1], gradual leakage of interstitial fluid from the intracellular space into the pial space in the brain parenchyma [1] and fibrosis with obstruction of the VR spaces along the length of the arteries and subsequent impedance to fluid flow [1].
Fig. 6 Large cystic-dilated pervascular Virchow-Robin space in the area of the basal ganglia on the left.
Second opinion for arachnoid cyst
Despite the fact that MRI diagnostics using a contrast agent provides the doctor with the necessary information, there is still a risk of error. It is associated primarily with the doctor’s lack of residual experience in interpreting MRI results and identifying cysts. Not a single patient is immune from such errors, and they happen both in large cities and in small towns. In this situation, the only way to eliminate an error or at least significantly reduce its likelihood is to obtain a second opinion from a highly qualified specialist
The National Teleradiological Network (NTRS) offers you the opportunity to receive consultations from the country's leading specialists in the field of MRI diagnostics, who have extensive experience in analyzing tomographic images of various diseases. To get a consultation, you just need to upload the scan results to our server and within a day you will receive an alternative opinion to the opinion of your doctor.
Perhaps it will be the same as the first medical opinion, perhaps it will differ from it, but the second opinion will definitely allow you to reduce the risk of misdiagnosis and incorrect treatment to almost zero.