Vascular tone is the tension of blood vessels, supported by smooth muscles, an important factor in the blood supply to internal organs, one of the tools for general blood circulation. Vascular tone is influenced by the endothelium, the inner layer of blood vessels. Very thin (one cell thick), but plays a significant role in regulating vascular and cardiac tone, as well as in angiogenesis (formation of new vessels) and immune defense.
The fact that the endothelium is formed by a single layer of flat mesenchymal cells should seem to mean its insignificance, “microscopicity”. In fact, it is the largest organ in humans, present in all tissues. It affects blood clotting, kidney filtration, brain nutrition, and many other processes.
Theory
Tests
Help the site
Disable advertising
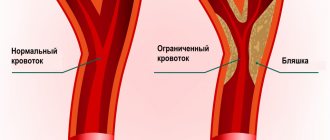
All vessels, with the exception of capillaries, have smooth muscle cells (SMCs) , due to which the lumen of the vessel , therefore the resistance to blood flow and the intensity of blood flow changes in a given region.
Local regulatory mechanisms:
- all vessels with SMCs are characterized by the original - basal tone created by the automaticity of smooth muscles;
- under the influence of various factors, basal tone can increase, while the vessels narrow and less blood enters the region;
- when vascular tone decreases, they dilate and blood flow into the region increases.
A decrease in tone leads to vasodilation, while an increase leads to vasoconstriction.
Regulation of vascular tone through surrounding tissue
The neighboring tissue, which is supplied with blood through these vessels, also participates in pressure regulation. Metabolic factors that arise in the tissue during energy production or, conversely, during its consumption, affect blood vessels. The channel for such an effect is either the endothelium or vascular smooth muscle. Reactions of the endothelium and smooth muscles lead to the expansion or contraction of blood vessels, which normalizes the pressure inside them.
In addition to direct metabolic products, blood vessels can also be affected by other factors related to tissue functions. For example, skeletal muscle secretes the enzymes nitric oxide (NO synthase) and cyclooxygenase (COX). This is in addition to "pure" nitric oxide and prostaglandins, which are also typical of skeletal muscle. During heavy physical activity (that is, with regular tension of the striated muscles), these products are released in particularly large quantities, can reach local vessels, affect their tension or elastic relaxation of the walls, the width of the internal lumen, and pressure.
The extent of this influence (significant or insignificant) is not yet known to pathologists. Various hypotheses have been put forward - but be that as it may, the influence of skeletal muscles on the regulation of vascular tone cannot be excluded.
Moreover, new factors of such influence are constantly being identified. Thus, it became known that certain cells that make up the heart muscle (cardiomyocytes) also regulate vascular tone in their own way. These cells also secrete nitric oxide (NO), which spreads through the internal tissues to the vessels, primarily the coronary vessels. Thus, the heart regulates the pressure inside the vessels not only by supplying blood, but also additionally, through nitric oxide, making the lumens of the vessels optimal for a specific level of blood flow.
Vascular tone
Tone is the tension created by the asynchronous contraction of the SMC of the middle layer of the vascular wall, which has automaticity.
Tone components:
- basal tone,
- humoral,
- central (neurogenic).
Mechanisms for regulating vascular tone:
- Local mechanisms that ensure blood flow through individual organs and tissues, that is, controlling the amount of blood flow in individual regions.
- The central mechanisms regulating systemic blood circulation are the constancy of blood pressure, blood flow, blood volume, etc.
Local regulatory mechanisms
The principle of local regulation is to ensure the independence of blood flow in organs from changes in systemic hemodynamics, that is, the provision of blood to a given region in its interests.
Local mechanisms for regulating blood vessel tone include :
- myogenic,
- metabolic.
Myogenic mechanism
- myogenic autoregulation is characteristic of the vessels of the brain, kidneys, heart, liver, celiac region, that is, regions where it is necessary to maintain constant blood flow;
- an adequate stimulus to SMCs is their stretching;
- with an increase in blood pressure (BP) -> stretching of the vascular walls -> contraction of the SMC of the vessels -> an increase in vascular tone and maintaining the same lumen -> the blood flow in the vessels does not change;
- a decrease in blood pressure causes a decrease in vascular tone due to relaxation of the SMC: in this case, despite the decrease in blood pressure, the flow of the same volume of blood into the vessels remains,
- Thus, the amount of basal tone is influenced by the level of blood pressure.
Metabolic mechanism
- metabolic products, dilating blood vessels, increase blood flow in working organs;
- as a result of insufficient supply of oxygen and nutrients to the region, metabolites accumulate in the tissues and blood flow increases due to the expansion of precapillaries.
Vascular tone decreases with a decrease in oxygen and carbon dioxide pressure, an increase in H and C3H6O3 ions and temperature - as a result, blood flow in working organs increases in proportion to their activity.
Central regulatory mechanisms
- nervous (reflex),
- humoral.
Nervous mechanisms
Vasomotor - vasomotor nerves:
- vasoconstrictors - vasoconstrictor nerves,
- Vasodilators are vasodilating nerves.
Vasoconstrictors
- All vasoconstrictors are sympathetic adrenergic nerves.
- The vasoconstrictor effect occurs when norepinephrine (NA) acts on α-adrenergic receptors.
- Impulses through sympathetic vasoconstrictors constantly arrive to the vessels from the neurons of the lateral horns of the thoracolumbar segments of the SC with a frequency of 1-3 impulses/s, maintaining resting tone.
- At a frequency of more than 3 pulses/s (from 3 to 15) - increased tone.
Vasodilators
- Parasympathetic cholinergic nerves:
- chorda tympani - drum string - dilates the vessels of the submandibular salivary gland;
- n. lingualis - lingual nerve - dilates the vessels of the tongue;
- n. glossopharyngeus - glossopharyngeal - dilates the vessels of the tonsils, posterior third of the tongue, parotid salivary gland;
- n. pelvicus - pelvic - dilates the vessels of the area of the same name.
- Sympathetic nerves:
- cholinergic, innervating vessels of skeletal muscles;
- adrenergic - a vasoconstrictor effect occurs when NA acts on β-adrenergic receptors in the vessels of the heart, brain and lungs.
- Dorsal root sensory nerves - dilate skin vessels according to the axon reflex (mediator - ACh).
Axon reflex:
- dilation of skin blood vessels is observed when insects bite, under the influence of mustard plasters, rubbing, scratching the skin;
- blood vessels that do not have special vasodilators dilate due to a decrease in the tone of vasoconstrictors (for example: in the abdominal organs).
Impulses along the vasomotor nerves to the vessels constantly come from the vasomotor center (VMC) .
The main localization of the vasomotor center is in the medulla oblongata (Ovsyannikov, 1871).
How does the endothelium affect vascular tone?
Among the products of endothelial activity, nitric oxide (NO) attracts attention. It regulates vascular tone. The production of nitric oxide increases with increasing pressure at a given vascular site. Blood pressure may rise due to increased physical activity or under the influence of certain hormones (for example, acetylcholine).
Increased pressure on the vessel wall activates a special set of enzymes called endothelial nitric oxide synthase (eNOS). These enzymes spur increased production of NO. Nitric oxide molecules are freely released through cell membranes and penetrate into smooth muscle. Under the influence of NO, muscle tissue relaxes - the walls of blood vessels, without encountering resistance from smooth muscles, expand, and the pressure inside these vessels drops.
A decrease in pressure weakens eNOS activity in the endothelium. Less nitric oxide is released - the vascular muscles tense again, maintaining the pressure at the working level.
Vasomotor center (VDC)
SC centers (lateral horns of gray matter) -> bulbar centers: vasoconstrictor, vasodilator -> hypothalamic centers (anterior ( depressor zone ) and posterior ( pressor zone ) parts of the hypothalamus) -> cortical representation of the SDC.
After transection of the brainstem above the quadrigeminal artery, blood pressure does not decrease , but when the brain is transected between the medulla oblongata and the spinal cord, it drops from 120 mm Hg. Art. up to 70-80.
SDC consists of 2 departments:
- pressor department,
- depressor department.
Both of these departments do not have clear boundaries. They are located at the bottom of the 4th ventricle among the neural structures of the reticular formation and mutually overlap each other.
Pressor and depressor neurons of the SDC are in a reciprocal relationship.
There are more pressor neurons than depressor neurons. The state of the SDC is judged by pressor neurons .
The SDC also includes other parts of the central nervous system.
At rest, the hypothalamus does not actively participate in the regulation of blood pressure.
The influence of the cortex on the regulation of blood pressure is conditioned reflex - an increase in blood pressure before the start, with excitement.
Conclusion: a multi-level system for regulating the functions of the cardiovascular system ensures adequate adaptation to the conditions of the external and internal environment.
The tone of the SDC depends on the nerve impulses constantly coming to it from the receptors of various reflexogenic zones.
Vascular reflexes
Vascular reflexes are divided into:
- own and
- conjugated.
Own reflexes
They are carried out from mechanoreceptors located in the heart and blood vessels ( baroreceptors ).
These receptors stabilize blood pressure.
There are own reflexes:
- pressor - increasing low blood pressure,
- depressor - lowering high blood pressure.
Reflexogenic zones (areas of maximum accumulation of receptors):
- aortic arch,
- carotid sinus (bifurcation of the common carotid artery into external and internal).
Depressor reflex: with an increase in blood pressure -> the baroreceptors of the aortic arch and carotid sinus are irritated -> excitation along the sensory nerves - aortic (depressor) and sinus (Hering's nerve) -> medulla oblongata -> the vagal center is excited and the vasomotor center is inhibited -> heart rate decreases - > blood vessels dilate -> blood pressure decreases (normalizes).
When blood pressure drops, the opposite is true, that is, the pressor reflex .
Own reflexes:
- are also carried out from chemoreceptors located in the aortic and carotid bodies;
- they are excited when CO2 and H ions increase in the blood and when O2 decreases;
- impulses arriving from chemoreceptors in the medulla oblongata increase the tone of the central nervous system, which leads to an increase in pressure.
Chemoreceptors are not in the vessel wall, but in the aortic and carotid bodies or glomeruli under the adventitia of the vessel and are penetrated by a network of capillaries.
From chemoreceptors -> SDC of the medulla oblongata -> SDC is excited -> vasoconstriction -> increase in blood pressure -> rapid blood renewal.
Conjugate reflexes
Carried out from receptors located outside the heart and blood vessels:
- they disrupt the stability of blood pressure, causing pressor reactions;
- distinguish conjugate reflexes: exteroceptive - from skin receptors,
- interoceptive - from internal organs.
Brakes and accelerators of vascular tone
Hormones produced by the adrenal medulla circulating along with the blood are important for maintaining tone (especially of peripheral vessels). Adrenaline is well known. But to maintain vascular tone, norepinephrine, which is the biological precursor of adrenaline, is more important. It has a more active effect on blood vessels - but is much gentler on the heart, bronchi and intestines, and does not harm metabolism.
Norepinephrine regulates both blood pressure and peripheral vascular resistance. If the position of the body changes abruptly (for example, a person is lying down and suddenly stands up), the amount of norepinephrine increases many times. It strongly constricts the blood vessels - this maintains the pressure inside the arteries, which, in theory, should drop when the body is transferred from a horizontal to a vertical position (it is one thing if the blood spreads horizontally, another thing when it needs to be pumped upward).
An increased level of norepinephrine affects the vascular muscles - it stabilizes the blood vessels. But with an increase in its level, the reaction of presynaptic adrenergic receptors slows down - which immediately leads to a sharp decrease in the secretion of norepinephrine. The pressure in the arteries is regulated, and there is no longer a need for smooth muscles to compress the vessels. Consequently, there is no need for norepinephrine - it “calms down”. Self-regulation of pressure is due to self-regulation of functions for the production of norepinephrine.
This is a very complex biochemical balance; its maintenance involves not only the hormones dopamine and tyrazine, from which norepinephrine is synthesized, but also adenosine, acetylchodine, histamine, serotonin, prostaglandin, and angeotensin. Moreover, if some hormones (angeotensin) spur the synthesis of norepinephrine, others (prostaglandin, etc.), on the contrary, inhibit it. The process develops cyclically, under the influence of brakes and accelerators.
This “device” is very important for vascular areas that are characterized by frequent and sudden changes in pressure.
The reaction of smooth muscles that regulate pressure in blood vessels is also ensured by the content of ion exchange. The positive ions of potassium and calcium are of particular importance. Their complex transformations in interaction with arachidonic acid and substances stimulate contraction (contraction) or relaxation of vascular muscles, adapting to pressure surges.
Humoral regulation
- Hormones formed in the endocrine glands: adrenaline, norepinephrine, vasopressin, etc. - constrict blood vessels.
- Vasoactive agents (local hormones) formed in tissues - acetylcholine, bradykinin, histamine, prostaglandins, etc. - dilate blood vessels.
- Dual-acting substances - catecholamines:
- alpha - narrowing
- betta - extension.
The hormones adrenaline and norepinephrine narrow the arteries and arterioles of the skin, skeletal muscles, and abdominal organs. Coronary vessels, vessels of the brain, and lungs expand at the same time, since it all depends on which adrenergic receptors perceive the hormone. When NA interacts with α-adrenergic receptors, the vessels narrow, and when interacting with β-adrenergic receptors , they dilate. β-adrenergic receptors predominate in the vessels of the heart, lungs, and brain.
Vasopressin mainly constricts arterioles and veins.
Angiotensin II is formed from plasma α-globulins under the influence of renin (JA cells of the renal cortex) and also constricts blood vessels.
Vascular tone:
- basal tone - the tone of the SMC and the influence of sympathetic vasoconstrictors;
- resting tone - tone of the SMC and the influence of sympathetic nerves with a frequency of 1-3 impulses/s;
- increased tone - impulses along sympathetic vasoconstrictors with a frequency of 3-15 impulses/s.