Magnetic resonance imaging is an informative non-invasive way to study cerebral structures. Diagnosis of pathological processes in the brain using other methods is complicated by the presence of the skull, which performs a protective function. Scanning using an induction field allows you to identify the slightest changes. Foci of gliosis are most accurately detected on MRI of the brain; a specialist can determine the nature and localization of the process.
Various forms of gliosis on MRI images of the brain
The study is carried out using a tomograph consisting of a mobile table and a wide tunnel. The device generates a magnetic field, under the influence of which the hydrogen atoms in water molecules are aligned in a special way. Sensitive sensors read the response of scanned tissues, obtaining information about the degree of fluid saturation of brain cells.
A computer program converts the signal into a series of layer-by-layer images taken in axial, sagittal and frontal projections. Based on the images obtained, the doctor can, if necessary, reconstruct a 3D model of the brain.
General information
Gliosis of the brain is a pathological process manifested by the replacement of neurons with glial elements.
Gliosis is not an independent disease; rather, it is a protective reaction to the death of neurons, that is, a secondary process. At the same time, the process of destruction of neurons stimulates the filling of the resulting voids with glial cells, which leads to a change in the quantitative ratio of elements of the nervous tissue. Brain tissue consists of a collection of neurons, ependymal membrane and glial cells. Normally, glial tissue is responsible for trophic/secretory functions and metabolism in brain cells, and also performs the function of protecting neurons. It accounts for about 40% of the total brain mass. The proliferation of glial cells forms foci of gliosis in the white matter of the brain, which, depending on the etiology of the primary disease, can be focal/diffuse in nature. Foci of gliosis can be located in any area (structures) of the brain. And the more glia are formed, the less efficiently the central nervous system functions. With a large proliferation of glia, a cystic-gliotic atrophied area of brain tissue can form. The more glia are formed in the white matter, the worse the functioning of the entire nervous system. A cystic-glial-atrophic area is formed.
There are no statistical data on the incidence of various types of gliosis. It can only be noted that supratentorial foci of gliosis are most common.
Supratentorial lesions - what are they? Supratentorial are foci of gliosis of vascular origin. Various pathological processes in the vessels of the brain ( thrombosis , fibrosis , necrosis ) that cause circulatory disorders contribute to the formation of small hyper/hypertensive areas, which are accompanied by such disorders as poor coordination, dizziness , and changes in handwriting.
Single foci of gliosis
Focal gliosis is characterized by single, clearly defined islands in the white matter, the size and location of which is determined by the causes of neuronal death. They occur in people of any age and, perhaps, as a manifestation of natural age-related degenerative processes in brain tissue, ischemia of cerebral structures, local inflammatory process, chronic hypertension demyelination process , and as a consequence of injuries during childbirth in infants. Typically, single (limited foci) of gliosis of the brain are an accidental finding on CT/MRI, since in most cases they are not clinically manifested and do not cause discomfort, with the exception of their localization in the frontal lobe, where the centers associated with feelings and sensations are located, which can manifested by the appearance of hallucinations. A single gliosis of the brain is not prone to proliferation.
Multiple foci of gliosis
The appearance of multiple foci of gliosis is caused by injuries and acute/chronic circulatory disorders of the brain, that is, of vascular origin. As the pathology/disease that causes neuronal death develops, both the number and size of the altered areas increase. They occur predominantly against the background of severe atherosclerosis , stroke , cerebral infarction , with compression of cerebral vessels and as a result of age-related changes. Multiple foci of gliosis for the most part enhance the clinical symptoms of the underlying disease and cause dysfunction of the central nervous system.
Types of changes
In medicine, dystrophic manifestations in the brain substance are divided into two types:
- Diffuse.
- Focal.
In the first case, pathological changes spread evenly to the entire brain, and not to its individual areas. They are caused either by general disturbances in the functioning of the blood supply system or by infections (meningitis, encephalitis, etc.).
An important cause of this condition is thought to be changes in blood flow to the area around the ventricles of the brain, which is fragile and prone to injury, especially before 32 weeks of gestation. Premature babies with intraventricular hemorrhage are also at increased risk of developing this condition
Exams used to diagnose periventricular leukomalacia include ultrasound scanning and MRI of the head. The cardiac, pulmonary, intestinal and renal activity of premature infants is carefully monitored and treated in the Neonatal Intensive Care Unit.
Diffuse changes are manifested mainly by a decrease in a person’s performance, a dull headache, difficulty switching to another type of activity, a narrowing of the patient’s range of interests, apathy and sleep disorders.
And what a focal change in the brain substance of a dystrophic nature is can be understood by the fact that it can be caused by various minor pathologies:
These problems often arise during the first or second year of life. This condition can cause cerebral palsy, especially stiffness or increased muscle tone in the legs. These will likely be those that compromise movements such as sitting, crawling, walking, and weapon movement. These children may require physical therapy. Extremely premature babies have more problems with learning than with movement.
The child should visit his regular pediatrician for scheduled exams. Neonatal diseases of prenatal and perinatal origin. Hypoxico-ischemic encephalopathy: neuropathology and pathogenesis. Introduction. The predominant semiologic picture should be considered in conjunction with the patient's clinical context and epidemiological data to reach a diagnostic conclusion.
- cysts (small cavities that form in the brain),
- small foci of necrosis (tissue death in certain areas caused by lack of nutrients);
- gliomesodermal (intracerebral) scars that occur after injuries and concussions;
- minor changes in the structure of the brain matter.
That is, these are pathologies that cause disturbances in the blood supply in a small area. True, they can be either single or multiple.
The microcirculation of the brain forms a very complex vascular network of anatomy and varies among individuals. The vesicular arteries, in their deep course in the white matter, establish very little capillary anastomosis with adjacent nutritional arterioles, constituting relatively independent arterial metabolic units. On the other hand, the deep subepidemic arteries, which occur in the choroidal arteries, give penetrating branches to the white matter, although its path is shorter than that of the parade ground arteries.
There is a second terminal system of cortical and subepidemic arteries that supply the basal ganglia. There is very little anastomosis between the superficial and deep arteriolar systems. The arterial and venous systems are anatomically quite parallel. The perivascular space surrounds the wall of arteries and arterioles, as well as veins and venules, from the subarachnoid space to its intraparenchymal path.
Classification
The classification is based on the nature of the proliferation of glial cells and their localization.
Based on morphological characteristics, the following are distinguished:
- The isomorphic form is characterized by an ordered proliferation of neuroglia.
- Anisomorphic form - has a pronounced cellular structure and is characterized by chaotic growth; most often localized subcortically/paraventricularly. Periventricular gliosis - formed in the ventricles of the brain. Often periventricular gliosis is accompanied by the development of cysts. Fibrous form—the predominance of the fibrous type structure is noted.
According to the localization of the pathological process, the following are distinguished:
- Periventricular gliosis - glial cells are formed in the ventricles of the brain. Periventricular gliosis is often accompanied by the development of cysts.
- Perivascular (vascular) gliosis is the growth of glia along atherosclerotic vessels. It is often diagnosed on MRI as microangiopathy with the presence of foci of gliosis.
- Subependymal gliosis is predominantly localized on the inner lining of the ventricles of the brain.
- Marginal gliosis - located on the surface of the brain.
- Marginal gliosis - foci of degeneration are localized in the intrathecal region.
Based on quantitative criteria, single and multiple foci of gliosis are distinguished. Histologically, hypodense (without a definite structure, cannot be stained) and hyperintense (clearly structured, well stained) areas of gliosis are distinguished.
Based on the nature of the process/prevalence, the following are distinguished:
- A focal type of flow, involving a limited area of the brain (usually in the temporal/parietal regions).
- Diffuse type of course - characterized by multiple lesions of various sizes/localizations. Most often of vascular origin and may have the appearance of a cystic-gliotic formation.
Causes
The pathological process of replacing neurons with neuroglial cells may be based on a variety of reasons:
- Age-related changes caused by the natural process of neuron death.
- Diseases of hereditary origin - lysosomal storage disease ( Tay-Sachs disease ), inherited in an autosomal recessive manner, characterized by massive death of neurons in children, which is the cause of their death); genetically determined pathology - tuberous sclerosis .
- Birth injuries at birth.
- Traumatic brain injuries.
- Multiple sclerosis (destruction of myelin and the formation of foci of demyelination in various brain structures).
- Cerebral infarction (ischemic stroke).
- Hemorrhagic stroke is a hemorrhage into the structures of the brain, which forms foci of gliosis of vascular origin.
- Brain swelling.
- Epilepsy.
- Arterial hypertension/encephalopathy caused by a persistent increase in blood pressure.
- Neuroinfections ( encephalitis , meningitis ). oxygen starvation of brain tissue ( hypoxia ).
- Hypoglycemia (low blood sugar).
- Surgical interventions on brain structures.
- Atherosclerosis of cerebral arteries.
- Abuse of products containing animal fat.
Development mechanism
There are several provoking factors underlying this. They occur together or separately. It's more a matter of chance. In total there are 4 main ways:
- Consistently high blood pressure levels. A change in the nature of blood flow through the main vessels leads to stenosis (narrowing) of the arteries, a decrease in their elasticity and a reflex violation of capillary tone.
In addition, negative factors that provoke an increase in blood pressure (usually hormonal or toxic, from smoking, drinking alcohol) can also affect small vessels in the same way.
Then the process becomes complex. The entire brain is affected. Such a number of negative factors brings stroke closer every day.
- Inability to regulate vascular tone, changes in their physical properties due to hormonal instability. A textbook example of such a disorder is diabetes mellitus.
If treatment is not carried out, the body simply cannot provide homeostasis (a state of equilibrium). Hence the change in the tone of the capillaries, also arteries, veins.
Severe complications arise over a short period of time. Patients walk along the edge constantly.
- Improper functioning of the immune system. As a result, active synthesis of antigen-antibody complexes develops, followed by the formation of a special protein conglomerate—amyloid.
This substance settles on the walls of blood vessels and provokes degenerative changes over a short period of time. A similar mechanism applies to autoimmune ones. It is considered difficult to correct and dangerous because the prospects are vague.
- It is also possible for mineral salts to be deposited on the walls of the capillaries. Mainly calcium. This is a relatively common mechanism and occurs in children under one year of age. It is diagnosed during the same period.
In the initial stages, symptoms are not noticeable, but as they progress, health deteriorates.
Objectively, the clinical picture is presented by manifestations of nonspecific neurological deficit. Headaches, nausea, spatial disorientation and others are observed that cannot be linked to a specific disease.
Attention:
If you don't take control of the situation, the consequences are dire. Further development of deficiency, stroke, disability or death.
The timing of the negative scenario from beginning to end is different. In most patients, as a result of compensation of the body and adaptation of impaired blood flow, collaterals are formed. That is, parallel, additional networks of capillaries that were not there initially.
If they are sufficiently formed, the violations will not be so noticeable and the “X-hour” will come later. No one can say how much.
Symptoms
Clinical symptoms vary widely and are determined mainly by the symptoms of the underlying disease that caused gliosis. As a rule, single small foci of gliosis do not produce specific neurosymptoms and are discovered by chance during an MRI examination of the brain. At the same time, multiple (extensive) foci of gliosis almost always manifest neurosymptoms in the form of:
- Unreasonable long-term intense headaches that are not controlled by taking antispasmodics.
- Blood pressure instability (sudden changes in a short period of time).
- Periodically occurring dizziness .
- Decreased performance/increased fatigue.
- Changes in visual/auditory perception.
- Disorders of coordination, attention and memory.
- Motor disorders (with large lesions, up to convulsive conditions).
Clinical symptoms are largely determined by the localization of the focus of gliosis:
- Localization of foci of gliosis in the temporal lobes is characterized by frequent, intense, long-term headaches. With the vascular genesis of the process, the pain syndrome is combined with sudden changes in blood pressure.
- Supratentorial gliosis manifests itself mainly with visual disturbances – hallucinations; distortion of the outlines, sizes, shapes of objects; loss of visual fields, difficulty recognizing an object by appearance.
- Gliotic foci in the white matter of the brain can cause dizziness , an episyndrome characterized by increased convulsive activity with the possible development of epileptic seizures. Such symptoms develop as a complication of traumatic brain injury/surgery.
The localization of gliosis foci in the frontal lobes is often due to age-related changes. It is generally accepted that if diseases that can cause the death of neurons and the proliferation of glial cells have not been identified, then such a process should be considered a primary pathology that develops as the body ages and manifests itself as impaired concentration, attention, memory, fine motor disorders, and slowed reactions.
Treatment
There is no specific therapy for gliosis. Treatment methods depend on the underlying disease that caused the death of neurons. Main goals of therapy:
- slow down the progression of the process;
- ensure normal trophism of central nervous system tissues;
- eliminate oxygen starvation;
- normalize metabolic processes.
Traditional medicine
To eliminate the symptoms of brain changes, the following groups of drugs are prescribed:
- Vasoactive - drugs that activate cellular metabolism and improve tissue trophism (Cavinton, Vinpocetine).
- Antiplatelet agents are drugs that slow down platelet sedimentation (all derivatives of acetylsalicylic acid).
- Agents that improve the condition of the walls of small and large arteries (Ascorutin, vitamins).
- Nootropic substances - they increase the resistance of the central nervous system to the effects of negative factors (Piracetam, Nootropil).
- Statins – have lipid-lowering properties, preventing the development of atherosclerosis (Fenofibrate, Atorvastatin).
- Painkillers and antispasmodics to relieve headache attacks.
Surgery
Surgery for gliosis is prescribed extremely rarely.
Only for single large lesions. After surgery, treatment of the underlying disease that caused the death of neurons must be continued to avoid the development of relapses.
Indications for surgical intervention for a large single lesion are:
- violation of the outflow of fluid (CSF);
- convulsive seizures caused by a large area of gliosis;
- diagnosed neoplasm;
- changes in the functioning of internal organs.
With multifocal gliosis, only constant conservative treatment has a positive effect.
Complementary and alternative methods at home
Traditional medicine methods can be used only after consultation with a neurologist. Homeopathic remedies are prescribed as concomitants against the background of conservative therapy.
Decoctions and infusions of medicinal plants and fruits improve the functioning of the cardiovascular system and stimulate metabolism.
Diet for gliosis changes
The diet for gliosis is aimed at:
- Improving brain function and relieving vascular spasms. To achieve this result, you need to eat foods rich in magnesium: buckwheat, pearl barley, corn cereals, nuts, pumpkin seeds, lentils, cabbage of all varieties, figs.
- Relieving edema, improving heart function - foods with a high potassium content are introduced into the diet: citrus fruits, green vegetables and fruits, dried fruits, mushroom and potato dishes.
- Weight loss - to control body weight, remove baked goods, canned food, carbonated sweet drinks, smoked foods, fatty meats, fast food and semi-finished products from the daily diet.
The daily diet consists of fish, lean meat, cereals, fermented milk products, hard cheese, vegetables, nuts and fruits. It is better to steam, boil or bake foods.
Tests and diagnostics
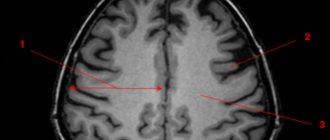
Diagnostics is based on imaging methods (MRI/CT) of the brain. These methods allow you to determine:
- location and size of pathological foci;
- the presence of marginal (perifocal) infiltration;
- structure (homogeneity) of the white matter of the brain;
- perivascular spaces of various areas;
- areas of the basal ganglia;
- the presence of other pathological formations;
- condition of the ventricles of the brain/pituitary gland, functionality/condition of the blood vessels of the brain.
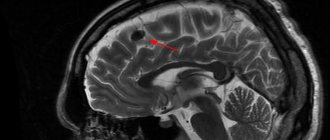
The image below shows multiple foci of gliosis.
MRI makes it possible to establish not only the presence of areas of gliotic changes, but also to identify the cause. MRI images provide a clear picture of the presence of areas in the brain that do not receive sufficient nutrition due to vascular obstruction by atherosclerotic plaques; allow you to identify inflammatory processes, areas of hematoma, and identify neoplasms. This, to a certain extent, makes it possible to eliminate the provoking factor and develop tactics to minimize the risks of further spread of the process.
Degrees
There is a WHO classification, according to which gliomas are divided into four grades:
- Grade I – slow-growing benign glioma, which is associated with a long life expectancy;
- Grade II – slowly growing “borderline” brain glioma, which tends to progress to grades III and IV;
- III degree – malignant glioma;
- IV degree – fast-growing glioma of the brain: the life expectancy of patients with this diagnosis is significantly reduced.
Diet
There is no special diet, but it is recommended to adhere to the diet recommended for the underlying disease that initiates the process of formation of glial lesions ( Diet for stroke , Diet for hypertension , atherosclerosis , diabetes mellitus , Diet for obesity , etc.). In general, it is recommended to adhere to a low-calorie diet with sufficient vitamin content (vegetables, fruits) and a minimum content of animal fats in the diet.
Prevention
No drugs or methods of specific prevention of neuronal death have been developed. To maintain the activity of neuro-processes and brain vessels, we can only recommend:
- Lead a healthy lifestyle.
- Monitor your body weight.
- Maintain age-appropriate physical activity.
- Constantly monitor blood pressure, cholesterol , and blood sugar levels.
- Minimize bad habits.
- Practice a healthy balanced diet by minimizing foods containing animal fats.
- Train brain functions: solve puzzles/crosswords, learn poetry, foreign languages.
Forecast
The prognosis of life with cerebral gliosis is largely determined by the underlying disease and can vary significantly depending on the volume of gliosis foci and the intensity of neuronal replacement. As a rule, the prognosis for life with single foci outside important brain structures is relatively favorable, while extensive foci of gliosis in areas of the brain responsible for important functions of the central nervous system can be unfavorable, for example, in the temporal lobe, initiating frequent epileptic seizures.
Turning to traditional methods of therapy
No matter how many medications are prescribed to the patient, additional maintenance of the body through the use of folk remedies will help improve the general condition.
- At the initial stage, in the presence of a few lesions, herbs perfectly support the human body, which help stabilize the blood supply system and increase metabolism.
- If a patient develops obesity, a diet based on a raw food diet is recommended; fasting days with periodic fasting are also required. This will contribute to the overall cleansing of the body from various substances that interfere with its healthy functioning.
- Taking tinctures and various decoctions, the action of which is aimed at combating the symptoms of the disease. At the pharmacy you can buy ready-made preparations that are balanced for treatment.
It must be emphasized that treatment using traditional methods can only be effective as a complement to traditional therapy, which should be prescribed by specialists. A long-term effect from the use of medications and treatment using traditional methods will not be achieved until the cause of glial formation is eliminated. Next, we will find out what preventive measures will help people avoid developing this disease.
How long do adults with cerebral gliosis live? This is a common question. More on this later.
List of sources
- Vereshchagin N.V., Gulevskaya T.S. Pathology of the brain in atherosclerosis and arterial hypertension. – M.: Medicine, 1997. – 228 p.
- Vasiliev V.N., Kindyashova V.V., Kozhevnikova V.V., Tikhomirova O.V., Lomova I.P., Serebryakova S.V. Clinical and diagnostic significance of microfocal brain lesions of vascular origin among management specialists // Medical, biological and socio-psychological problems of safety in emergency situations. 2014. No. 3. pp. 27-32.
- Gladky P. A., Sergeeva I. G., Tulupov A. A. Infectious lesions of the brain. Tutorial. Novosibirsk 2015. – 24 p.
- Putilina M.V. Chronic cerebral ischemia//Attending physician. 2005. No. 5.
- Yanishevsky S.N. Brain damage in patients with type 2 diabetes // International Journal of Endocrinology. No. 8(64). 2014 pp. 89-97.
Manifestations of gliosis in children
In children in the first months of life, gliosis develops as a result of the replacement by neuroglia of parts of the central nervous system tissue that died as a result of congenital diseases or intrauterine hypoxia. Lesions are often located in the ventricles of the brain.
- The child's reactions slow down;
- The functioning of the auditory and visual analyzers may be impaired;
- disappearance of the swallowing reflex;
- the child has a convulsive syndrome when he is afraid.
As a child grows, aggression often manifests itself in the form of self-harm, withdrawal, and delayed mental and physical development. Paralysis develops as glial changes increase.
Congenital anomalies leading to gliosis are associated with impaired fat metabolism. They can be diagnosed by examining amniotic fluid in the second trimester of pregnancy. If the diagnosis is confirmed, it is recommended to terminate the pregnancy, as there is no cure for this type of disease.