The complex structure of the human body allows distantly located organs to interact harmoniously to ensure internal balance - for example, the connection of the brain with underlying structures occurs through pairs of cranial nerves. One part of them provides sensitive perception of information, while others are responsible for motor activity. The smaller group has a mixed structure and is therefore ready for complex functioning. Understanding the characteristics of cranial nerves allows doctors to select the correct treatment for their diseases.
Diseases of peripheral processes
The main and most frequently diagnosed lesion of the peripheral plexuses, which is accompanied by functional disorders, is neuropathy or neuritis.
Symptoms characteristic of a violation of motor, sensory, and autonomic function occur. The person feels pain that radiates along the affected segment. Diseases that occur with dysfunction of the roots include: degenerative and dystrophic processes, metabolic disorders, inflammation of the roots and pinching by a tumor, osteophytes, hernia or other neoplasm.
Other peripheral plexus disorders:
- Optic nerves
- Diagnostics
- Cranial nerve examination
- Spinal cord, medulla spinalis. Development of the spinal cord.
- Neurology of motor nerves
- Second branch of the trigeminal nerve. Maxillary nerve, n. maxillaris. Pterygopalatine ganglion, ganglion pterygopalatinum.
- Vagus nerve (X pair, 10 pair of cranial nerves), n. vagus
- Functions of cranial nerves
- Taste nerves
- Treatment of the disease
- Diagnosis of neuralgia
- Sensitive nerve structures
- polyneuropathy, when several or many processes are involved in the lesion;
- plexitis is a disease characterized by damage to the entire plexus;
- radiculoneuritis is a simultaneous pathological process in the roots of the spinal canal and trunks;
- myeloradiculoneuritis - a condition characteristic of damage to the spinal cord, nerve trunks and roots;
- radiculitis – symptoms characteristic of injury to the spinal cord roots;
- ganglionitis is a pathological process characterized by damage to the intervertebral nodes.
Sensitive nerve structures
All brain nerves are important for the full functioning of the human body. If the predominant activity of a couple is the perception and transmission of information, then they are called sensory nerve fibers.
Thus, the olfactory nerve originates from the cells of the nasal mucosa. It then passes through the cribriform plate of the skull and moves deep into the brain to a structure called the olfactory bulb. Next, the nerve fiber forms a kind of tract, which passes into the olfactory triangle. The sensory structure ends in the tubercle of the cerebral cortex.
Another important sensory unit is the optic nerve. Its ganglion cells from the retina rush into the cranium, where the pair forms a kind of cross, from which the fibers run to the lateral geniculate structure of the brain. From here the optic nerve will continue to its final destination - the occipital part of the cerebral cortex.
Cells of the eighth pair of cranial nerves - auditory or vestibulocochlear. It is inherent not only to perceive and transmit the sounds of the surrounding world, but also to be responsible for the balance of the human body in space. Both parts of the nerve fiber - from the cochlear root and from the vestibular root, which begins from the vestibular ganglion, are directed to their final targets - the cerebellum, as well as the quadrigeminal cortex and the median geniculate body. The auditory nerve ends in the temporal gyrus.
Optic nerves
Visual disorders such as decreased acuity, color perception, visual field impairment, and blindness cause damage to any part of the second pair of the cranial nerve - visual. The types of violations depend on the dislocation of the source.
Tubular vision manifests itself in neuritis of the second pair of cranial nerves, hysteria, glaucoma, arachnoiditis. Complete blindness - as a result of injury, pathology of the chiasm. The condition is assessed based on the results of an examination of the visual components (acuity, visual field, etc.) and the fundus.
Polychromatic tables allow you to assess the level of color perception. Visual defects (so-called scotomas) detected by an ophthalmologist signal a pathology affecting the optic nerve. Patients themselves rarely consult a doctor when the severity decreases. Amblyopia can result in amaurosis. Sometimes complete loss of vision is the result of advanced pathology, when the pathological process is irreversible.
Pathologies of sensitive cranial nerves
In most cases, lesions of sensitive neurocytes of cranial nerves are associated with their hypothermia or damage, sometimes with neuroinfections suffered by a person.
For example, hearing impairment is expressed in people’s complaints about a persistent deterioration in their perception of sounds from the outside world, up to persistent deafness. At the same time, patients may experience noise in the head of varying intensity. If disorders occur in the vestibular pairs, symptoms of dizziness, disorientation in space, nausea and even vomiting will appear.
Visual disturbances are no less common - due to stagnation, swelling or injury of the nerve fiber, a significant decrease in visual acuity occurs for patients. There may be areas of no image on the retina of the eyeballs and excessive light sensitivity.
Lesions of the olfactory pair are less common in medical practice, since they are the shortest among the cranial nerve fibers and are located deep in the brain. People may experience olfactory hallucinations or deterioration/loss of the ability to distinguish odors.
Pathologies of mixed cranial-cerebral formations lead to a decrease in a person’s quality of life - disruptions in cardiac and respiratory activity, food absorption, distortion of taste perception, unpleasant sensations in the facial part of the skull, up to persistent pain syndrome due to chronic inflammation, for example, of the trigeminal pair. Such changes in the innervation of the cranial nerves can only be dealt with by competently selected complex treatment, which will be selected by a doctor taking into account the etiology of the disorder.
Diagnostics
Diagnosis is based on symptoms, medical history, and research:
- The doctor talks with the patient, finds out the symptoms. Finds out what the pain is and where it is located. Are there any infectious diseases in the head area? For example, otitis media, sinusitis, tooth extraction, adenoiditis.
- Then he examines and palpates the damaged area. The presence of swelling and redness is detected.
- When the doctor roughly presents the diagnosis, he examines for the presence of diseases with similar symptoms. That is, differential diagnosis is carried out. Refers for examination to a dentist and otolaryngologist.
- To determine the diagnosis, there is a method of applying a solution of cocaine hydroxide to the mucous membrane of the front of the nose. If the patient stops feeling pain, then this is inflammation of the nasociliary nerve.
- Next, instrumental studies should be carried out. Ophthalmoscopy, MRI of the head, biomicroscopy, anterior rhinoscopy.
- Once the diagnosis is made, treatment is prescribed.
With the help of additional examination, neuralgia of the nasociliary nerve is differentiated from other diseases. And they establish an accurate diagnosis.
Biomicroscopy of the eye
This is done using a slit lamp, the main part of which looks like a large slit. The device examines the structure of the eye, the back and front walls. This method allows you to see any damage, foreign body, and detect the disease at an early stage. Biomicroscopy allows you to see the condition of the retina and optic nerve.
Ophthalmoscopy
The fundus of the eye is examined using an ophthalmoscope. With the help of an eye mirror you can see blood vessels and nerves. Identify changes, redness, swelling.
Anterior rhinoscopy
This is done using a nasal speculum.
The anterior part of the nasal cavity is examined by inserting the device into the nostrils. The most suitable for this procedure is the Hartmann mirror. The doctor holds the device in his left hand, slightly dilating the nostril. In this case, the nasal septum and passages are visible. This is how redness, curvature, atrophy and hypertrophy are noticed. Sometimes it is possible to examine the nasal cavity using reflector lighting. It is used to examine children, as they may be frightened by an unknown object.
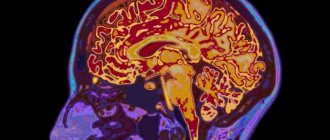
MRI of the head
To accurately confirm the diagnosis, an MRI of the head is performed. X-ray radiation is not used here. The examination is carried out using magnetic fields, which create an energy change in the examination area. This is how photographs are taken without the use of contrast. A cross-sectional image is displayed on the computer monitor.
What can damage each pair of nerves lead to?
Damage to cranial nerves, their tracts or nuclei leads to dysfunction:
- If the facial nerve is damaged, one side of the face will be unable to express emotions.
- The optic nerve can be damaged by skull fractures. In this case, irreversible blindness in the affected eye may develop.
- Any damage or injury to the vestibulocochlear structure can lead to hearing loss or balance problems.
- Injury to the hypoglossal nerve can cause complete paralysis of the tongue, leaving the person unable to eat or speak normally. There are many reasons that can damage the hypoglossal nerve, such as infection or nerve damage, causing the tongue to become paralyzed.
- Any dysfunction of the accessory nerve can cause the shoulders and neck to not function properly.
- Damage to the abducens nerve can result in blurred vision or double vision.
- If the vagus nerve is damaged, your resting heart rate may be around 100 beats per minute.
The cranial nerves, 12 pairs (the table is presented in the article for reference) of which are located inside the skull, when damaged, require focusing on protecting the brain. Some treatments for their conditions include surgery. Tumors are treated using radio waves.
Cranial nerves transmit information from the brain to parts of the human body, especially the head and neck, and back. Many of the 12 pairs are connected by connecting branches. The structures and connections of the human body are presented in anatomical tables and atlases, which help to better understand the functioning of the body.
Author: Belyaeva Anna
Cranial nerve examination
Motor fibers control the muscles of mastication and some muscles of the middle ear.
The trigeminal nerve has three sensory nuclei, two of which are located in the medulla oblongata and pons, and one in the midbrain. The only motor nucleus of this nerve is located in the pons.
The name “trigeminal” is due to the fact that it consists of three branches carrying information from three “floors” of the face - the forehead; nose, cheeks and upper jaw; lower jaw. Motor fibers pass in the inferior branch of the trigeminal nerve.
Facial nerve
(VII pair) contains three types of fibers:
1) afferent sensory fibers bring impulses from the taste buds of the anterior two-thirds of the tongue. These fibers end in the nucleus of the solitary tract, the common sensory nucleus of the facial, glossopharyngeal and vagus nerves. It extends from the medulla oblongata into the pons;
2) somatic motor fibers innervate the facial muscles, as well as the muscles of the eyelids, and some muscles of the ear. These fibers come from the motor nucleus located in the pons;
3) autonomic parasympathetic fibers of the facial nerve innervate the submandibular and sublingual salivary glands, lacrimal glands, and glands of the nasal mucosa. They begin from the parasympathetic superior salivary nucleus, also located in the pons
Glossopharyngeal nerve
(IX pair) is similar in composition to the facial nerve, i.e. also contains three types of fibers:
1) afferent fibers bring information from the receptors of the posterior third of the tongue and end on the neurons of the nucleus of the solitary tract;
2) efferent somatic motor fibers innervate some muscles of the pharynx and larynx. The fibers begin in the nucleus ambiguus, the common motor nucleus for the glossopharyngeal and vagus nerves, located in the medulla oblongata;
3) efferent parasympathetic fibers begin in the inferior salivary nucleus and innervate the near-ear salivary gland.
Nervus vagus
(X pair) is so called because of the extensive distribution of its fibers.
It is the longest of the cranial nerves; with its branches it innervates the respiratory organs, a significant part of the digestive tract, and the heart. The Latin name for this nerve is p. vagus,
which is why it is often called the vagus.
Just like the VII and IX nerves, the vagus contains three types of fibers:
1) afferents carry information from the receptors of the previously mentioned internal organs and vessels of the chest and abdominal cavities, as well as from the dura mater of the brain and the external auditory canal with the auricle. These fibers carry information about the depth of breathing, pressure in blood vessels, stretching of organ walls, etc. They end in the nucleus of the solitary tract;
2) efferent somatic motor innervates the muscles of the pharynx, soft palate, and larynx (including those that control the tension of the vocal cords). The fibers begin in the double core;
Important ECG online transcript with data entry
3) efferent parasympathetic fibers begin from the parasympathetic nucleus of the vagus nerve in the medulla oblongata. The parasympathetic part of the vagus nerve is very large, so it is predominantly an autonomic nerve.
From sensory cranial nerves
Only the vestibulo-auditory nerve (VIII pair) departs from the brain stem. It brings impulses from the auditory and vestibular receptors of the inner ear to the central nervous system. The sensory nuclei of this nerve - two auditory (ventral and dorsal) and four vestibular (lateral, medial, superior and inferior) - are located on the border of the medulla oblongata and the pons in the area of the vestibular field (see 7.2.2).
The VIII nerve originates in the inner ear and consists of two separate nerves - the cochlear (auditory) nerve and the vestibular (vestibular) nerve.
***
In conclusion, it should be noted that the nuclei of the cranial nerves have many afferents and efferents. Thus, all sensory nuclei send efferents to the thalamus (diencephalon), and from there information enters the cerebral cortex. In addition, sensory nuclei transmit signals to the reticular formation of the brain stem (see 7.2.6). All motor nuclei receive afferents from the cerebral cortex as part of the corticonuclear tract (see 6.4). Finally, there are numerous connections between the cranial nerve nuclei themselves, which facilitates the coordinated activity of various organs. In particular, thanks to the connections between the sensory and motor nuclei, the arcs of the stem unconditioned reflexes (for example, gag, blinking, salivation, etc.), similar to the spinal unconditioned reflexes, are closed.
Date added: 2015-10-01; | Copyright infringement
Related information:
Search on the site:
How are the cranial nerves located?
The cranial nerves are anatomically and functionally connected to the brain. Detailed location diagrams can be seen in anatomical atlases and in images of a frontal section of the brain.
Places where nerves exit the brain and skull:
- I – olfactory bulb and cribriform plate of the same bone.
- II – optic chiasm and canal, formed on the posterior hemisphere;
- III - enters the interpeduncular fossa, passes in the groove of the oculomotor nerve. The ending goes into the eye socket.
- IV - under the lower convexities of the midbrain, on the side of the frenulum of the superior medullary velum, exits the skull through the superior orbital fissure.
- V is the place of demarcation between the pons and the middle cerebellar peduncle. The optic nerve exits through the superior orbital fissure. The maxillary nerve passes through the foramen rotundum. The mandibular nerve passes through the foramen ovale.
- VI - passes along the groove between the pyramid and the bridge, exits through the orbital fissure.
- VII – the junction of the pons, medulla oblongata and cerebellum (pontocerebellar angle). Passes through the internal auditory canal, the facial nerve canal, and the stylomastoid foramen.
- VIII – cerebellopontine angle, internal auditory canal.
- IX – upper segment of the posterior lateral groove, jugular foramen.
- X – lies in the middle section of the posterior lateral groove, jugular foramen.
- XI - cranial roots exit through the lower part of the posterior lateral sulcus. The place where the spinal processes exit the brain is the space between the posterior and anterior lateral sulci. They exit into the skull through the jugular foramen.
- XII – anterior lateral groove, canal of the hypoglossal nerve.
When the fiber bundles of the cranial nerves are damaged, pain appears and various dysfunctions develop. The main pathologies of the cranial nerve are paresis, paralysis, neuralgia, neuritis, neuropathy. Treatment of pathologies takes place in the neurology department.
Spinal cord, medulla spinalis. Development of the spinal cord.
As already noted, phylogenetically the spinal cord (trunk brain of the lancelet)
appears at stage III of nervous system development (tubular nervous system).
At this time, there is no brain yet, so the trunk brain has centers for controlling all processes of the body, both vegetative and animal (visceral and somatic centers)
. According to the segmental structure of the body, the trunk brain has a segmental structure; it consists of interconnected neuromeres, within which the simplest reflex arc is closed. The metameric structure of the spinal cord is preserved in humans, which determines the presence of short reflex arcs in humans.
With the appearance of the brain (cephalization stage)
Higher control centers for the entire body arise in it, and the spinal cord falls into a subordinate position. The spinal cord does not remain only a segmental apparatus, but also becomes a conductor of impulses from the periphery to the brain and back, and bilateral connections with the brain develop in it. Thus, in the process of evolution of the spinal cord, two apparatuses are formed: the older segmental apparatus of the spinal cord’s own connections and the newer suprasegmental apparatus of the bilateral pathways to the brain. This structural principle is also observed in humans.
Decisive factor in the formation of the trunk brain
is adaptation to the environment through movement. Therefore, the structure of the spinal cord reflects the way the animal moves. So, for example, in reptiles that do not have limbs and move with the help of the body (for example, a snake), the spinal cord is developed evenly along its entire length and has no thickenings. In animals that use limbs, two thickenings occur, and if the forelimbs are more developed (for example, the wings of birds), then the anterior (cervical) thickening of the spinal cord predominates; if the hind limbs are more developed (for example, the legs of an ostrich), then the posterior (lumbar) thickening is increased; if both forelimbs and hindlimbs (four-legged mammals) are involved in walking, then both thickenings are equally developed. In humans, due to the more complex activity of the hand as a labor organ, the cervical thickening of the spinal cord was differentiated more strongly than the lumbar one.
The noted phylogenetic factors play a role in the development of the spinal cord and ontogenesis
.
The spinal cord develops from the neural tube,
from its posterior segment (the brain arises from the anterior segment). From the ventral section of the tube, the anterior columns of the gray matter of the spinal cord (cell bodies of motor neurons), adjacent bundles of nerve fibers and processes of these neurons (motor roots) are formed. From the dorsal section arise the posterior columns of gray matter (cell bodies of interneurons), posterior funiculi (processes of sensory neurons).
Thus, the ventral part of the brain tube is primarily motor
, and the dorsal one is
primarily sensitive
.
The division into motor (motor)
and
sensory (sensitive)
areas extends throughout the neural tube and is maintained in the brain stem.
Due to the reduction of the caudal part of the spinal cord, a thin cord of nervous tissue is obtained, the future filum terminale.
Initially, in the 3rd month of uterine life, the spinal cord occupies the entire spinal canal, then the spine begins to grow faster than the brain, as a result of which the end of the latter gradually moves upward (cranially). At birth, the end of the spinal cord is already at the level of the third lumbar vertebra, and in an adult it reaches the height of the first - second lumbar vertebra. Thanks to this “ascent” of the spinal cord, the nerve roots extending from it take an oblique direction.
Neurology of motor nerves
If cranial nerves are affected, neurological manifestations depend on their functional purpose. The group of motor ones emanating from the parasympathetic nuclei of the trunk includes:
- oculomotor (III);
- block (IV);
- abducent (VI);
- additional (XI);
- sublingual (XII).
Oculomotor pair
from the orbit it controls the oblique muscle, which ensures the elevation of the eyelid. The oculomotor provides neurons to the muscle that controls the pupil and eyelash movements. If it is affected, weakness and even paralysis of the above muscles appear. Then the eye opens only partially or does not open at all, accommodation is disrupted, the light reaction of the pupil disappears, and strabismus may develop.
Block
from the skull it runs into the eye socket and controls the rotation of the eyeball with the help of the oblique muscle. Its defeat is accompanied by deviations of the apple of the affected eye and double vision. The fibers of the trigeminal nerve branch into processes and perform many functions. They control and provide sensitivity to various parts of the face.
Neuronal bundle diverting
directs contractions on one side of the lateral muscle, and on the opposite side, the medial muscle. The symptoms that appear depend on the degree of damage to the nuclei or neurons. Various visual disturbances may occur: strabismus, double vision, hemiplegia. The greater length of the nerve increases the risk of damage.
Additional
consists of 2 (spinal and vagus) parts. Through a conductive (two-neuron pathway) it carries out motor functions. When the nerve is irritated, tonic muscle spasms develop in the sternoclavicular area (nodding movements of the head, its unnatural rotation). A one-sided lesion leads to difficulties in moving the head and shoulders; a bilateral lesion leads to the inability to make these movements, often the head tilts back.
Hyoid nucleus
located in the rhomboid fossa, its motor filaments innervate the lingual muscles. Damage to the 12th nerve leads to their paresis and decreased tongue mobility. Bilateral damage is fraught with the development of paralysis of the innervated organ (glossoplegia).
Important Hypothalamic syndrome: causes, symptoms and treatment
Motor nerve structures
In the nuclei of the midbrain, just below its aqueduct, the oculomotor nerve begins its journey. As it progresses, it forms a branched system of fibers - the upper parts of the pair are responsible for the functioning of the eyelids. While its lower three parts innervate the rectus muscle groups of the orbit.
Several more pairs of cranial nerve structures provide full movement of the eyeballs and adjacent tissues:
- trochlear - the nuclei of the pair are localized anterior to the cerebral aqueduct, and the fibers stretch to the superior oblique muscle of the orbit;
- abducens - the pair originates from the tegmental nuclei of the pons, the fibers extend to the lateral rectus muscle of the orbit;
- accessory nerve - its upper part begins in the region of the medulla oblongata, while the lower part in the upper part of the spinal cord, after exiting the cranial cavity through the foramen magnum, it again splits into two parts, which go to the fibers of the vagus nerve, as well as to the muscle structures of the brachial nerve belts;
- hypoglossal - the pair is localized mainly in the rhomboid fossa with its core, then its fibers move through the medulla oblongata and leave the cranial cavity to innervate the muscle structures of the tongue.
A person immediately learns about damage to the fibers of intracranial pairs - deviations in the functioning of the muscles of the orbit and oral cavity.
Vagus nerve (X pair, 10 pair of cranial nerves), n. vagus
N. vagus, vagus nerve
, which developed from the 4th and subsequent gill arches, is so called due to the vastness of its distribution.
It is the longest of the cranial nerves. With its branches, the vagus nerve supplies the respiratory organs, a significant part of the digestive tract (up to the colon sigmoideum)
, and also gives branches to the heart, which receives fibers from it that slow down the heartbeat.
N. vagus
contains three types of fibers:
1. Afferent (sensory) fibers
, coming from the receptors of the named viscera and vessels, as well as from some part of the dura mater of the brain and the external auditory canal with the auricle to the
sensitive nucleus (nucleus solitarius)
.
2. Efferent (motor) fibers
for the voluntary muscles of the pharynx, soft palate and larynx and the efferent (proprioceptive) fibers emanating from the receptors of these muscles.
These muscles receive fibers from the motor nucleus (nucleus ambiguus)
.
3. Efferent (parasympathetic) fibers
emanating from
the vegetative nucleus (nucleus dorsalis n. vagi)
.
They go to the myocardium of the heart (slow down the heartbeat) and the muscular lining of the blood vessels (dilate the blood vessels). In addition, the cardiac branches of the vagus nerve include the so-called n. depressor, which serves as a sensory nerve for the heart itself and the initial part of the aorta and is in charge of the reflex regulation of blood pressure. Parasympathetic fibers also innervate the trachea and lungs (narrow the bronchi), esophagus, stomach and intestines to the colon sigmoideum
(increase peristalsis), embedded in the named organs of the gland and glands of the abdominal cavity - liver, pancreas (secretory fibers), kidneys.
Parasympathetic part of the vagus nerve
is very large, as a result of which it is primarily an autonomic nerve, important for the vital functions of the body. The vagus nerve is a complex system consisting not only of nerve conductors of heterogeneous origin, but also containing intra-trunk nerve nodes.
Fibers of all types associated with the three main nuclei of the vagus nerve
, leave the medulla oblongata in its sulcus lateralis posterior, below the lingual tray nerve, with 10-15 roots, which form a thick nerve trunk, leaving the cranial cavity together with the lingual tray and accessory nerves through the foramen jugulare.
In the jugular foramen, the sensitive part of the nerve forms a small node - ganglion superius
, and at the exit from the foramen - another fusiform ganglion thickening -
ganglion inferius
.
Both nodes contain pseudounipolar cells, the peripheral processes of which are part of the sensory branches going to the named nodes or receptors of the viscera and blood vessels ( ganglion inferius
) and the external auditory canal (
ganglion superius
), and the central ones are grouped into a single bundle, which ends in
the sensitive nucleus, nucleus solitarius.
Upon exiting the cranial cavity, the trunk of the vagus nerve
goes down to the neck behind the vessels in the groove, first between v.
jugularis interna and a. carotis interna, and below - between the same vein and a. carotis communis, and it lies in the same vagina with the named vessels. Next, the vagus nerve penetrates through the upper thoracic aperture into the chest cavity, where its right trunk is located in front of a. subclavia, and the left one is on the anterior side of the aortic arch. Going down, both vagus nerves go around the root of the lung from behind on both sides and accompany the esophagus, forming plexuses on its walls, with the left nerve passing along the front side, and the right one along the back. Together with the esophagus, both vagus nerves penetrate through the hiatus esophageus of the diaphragm into the abdominal cavity, where they form plexuses on the walls of the stomach. The trunks of the vagus nerves
in the uterine period are located symmetrically on the sides of the esophagus.
After the stomach turns from left to right, the left vagus moves forward, and the right one moves back, as a result of which the left vagus
, and the right one on the posterior surface.
Mixed nerve fibers
Their complex structure—the presence of both sensory and motor nerve cells—allows these cranial nerves to perform many important functions for humans.
Thus, the exit point of the trigeminal nerve can be called the area between the middle cerebellar peduncle and the pons. The sensory fibers of the pair - the orbital with the maxillary, as well as the mandibular - connect with the motor ones, and then branch into many smaller branches. In total, their number reaches 15, and their activity covers almost the entire facial part of the cranial muscles.
The nucleus of the seventh cranial pair is located in the pons, or rather its tire. It is also called the facial nerve. It rushes through the layers of the pons towards the base of the brain, where the pair will be divided into several branches:
- large rocky;
- stirrup;
- drum string.
The glossopharyngeal nerve is no less complex in structure. Experts trace the pair from the inferior olive to the pharyngeal plexus and the thickness of the tongue. Many branches and interweavings with other cranial bundles of neurocytes allow it to perform a variety of functions. Whereas the vagus pair, intertwining with the fibers of the glossopharyngeal and accessory intracranial formation, as well as vessels, creates a complex neurovascular structure. Its functioning affects the organs of the abdomen and solar plexus.
Functions of cranial nerves
There are 3 types of structures considered. Some are responsible for muscle contraction; these are the motor (activator) functions of the cranial nerves. Others transmit impulses and “knowledge” received from the senses to the cortex for analysis. There are also mixed cranial nerves that perform both tasks in parallel. Functionality is determined by the type of neuronal fiber transmission.
Motor cranial nerves
There are 4 pairs in this group, each performing separate tasks. Motor nerves:
- Trochlear (IV)
– associated with the upper muscle, facial (oblique). Provides the eyeball with the ability to rotate to the sides and rotate. - Abductor (VI)
– connected to the rectus lateralis muscle. Necessary for retracting the eyeball to the desired direction. - Accessory (XI)
- innervates the sternocleidomastoid muscle. Thanks to it, the neck bends, the head turns, tilts to the sides, leans back, and the shoulders move. - Hypoglossal (XII)
– the 12th pair of cranial nerves is connected to the oral cavity. The structure is primarily responsible for comfortable swallowing and precise movements of the tongue muscle.
Important Neural tube in the fetus
Sensory cranial nerves
An alternative name is sensory pairs, due to their connections with the sensory organs. Sensory cranial nerves perform the following functions:
- Olfactory (I)
– the shortest fibers in length. Necessary for the perception of smells. - Visual (II)
– transports impulse data from the photoreceptors of the retina to the cortex. These cranial nerves are responsible for visualization. - Vestibulocochlear (VIII)
– vestibular functions. This pair is necessary to maintain a sense of balance and transmit auditory signals.
Mixed cranial nerves
The described group of neuron fibers is responsible for both motor activity and the sensitivity of certain structures. Cranial mixed nerves:
- Oculomotor (III)
– transmits signals to the middle section. The pair is responsible for the sensitivity of the pupils to changes in light (constriction and dilation). At the same time, nerves provide movement of the eyeballs. - Trigeminal (V)
is the largest neural formation. This pair transmits sensory information from facial tissues and mucous membranes. Additionally, the structures regulate the movements of the masticatory muscles. - Facial (VII)
– the main task is to “command” facial expressions, control the functioning of the salivary and lacrimal glands. In parallel, the nerves transmit information about taste from the tongue receptors to the brain. - Glossopharyngeal (IX)
– associated with structures of the same name. In the oral cavity, these human cranial nerves collect sensory information about taste. The pair also provides swallowing by transmitting commands to the cervical muscles and the salivary gland. - The vagus (X)
is the most “loaded” nerve. “Serves” the heart, respiratory tract, digestive and filtering organs. It affects the swallowing process, regulates the overall activity of a person, and adjusts the intensity of stress. The pair can interact with the sympathetic system and most internal organs.
Classification
Cranial nerves supply sensory, motor and autonomic innervation to the structures of the head and neck. They are classified depending on their exit from the skull and on a functional basis.
At the exit point
All cranial nerves exit the brain, bypassing the spinal nerve. They are part of the peripheral NS, as they are directed to the cranial and cervical structures. Sensory nerves are formed from young neuronal cells, and motor nerves are formed from cells of the motor nuclei.
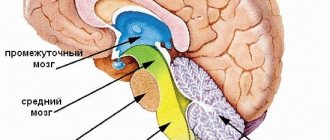
| Brain department | Associated cranial neuron |
| Brain | I |
| Thalamus | II |
| Midbrain | III IV V VI VII VIII (partially) |
| Medulla | VIII (partially) IX X XI XII |
After exiting, the nerves travel from their source to various parts of the body: the head, face, mouth, and some around the periphery of the body.
By function
Cranial nerves (the table characterizes 12 pairs for reference) are classified as sensory, motor, or a combination of both.
This means that the axons (neurites that carry nerve impulses) in these nerves originate from sensory ganglia (a ganglion of axons) outside the skull or motor nuclei in the brain stem. Axons with sensory functions form synaptic endings, with which they subsequently enter the stem nuclei.
| Sensory | Olfactory, visual, vestibulocochlear pair | The first 2 pairs, the olfactory and optic nerves, develop as outgrowths in the anterior medullary vesicle. These nerves do not have peripheral sensory nodes. |
| Motor | Oculomotor pair, trochlear nerve, abducens, accessory and hypoglossal nerves | Motor axons innervate the skeletal muscles of the head or neck. |
| Mixed (nerves of gill arches) | Trigeminal, facial, glossopharyngeal, vagus | The sensitive parts of the nerves of the branchial arches have nerve ganglia (ganglia), in which the organs of peripheral sensory neurons are located. |
The cranial nerve nuclei are functionally organized into distinct nuclei in the brainstem. In general, the nuclei located towards the back tend to be sensory, while the nuclei located towards the front tend to have motor functions.
Taste nerves
Ellipsoidal-shaped cells located in the mouth are designed to detect taste (taste bud). Taste buds consist of basal cells and chemoreceptors (the taste receptors themselves). Taste buds of different types are located on the tongue, cheeks, soft palate, epiglottis in the initial part of the esophagus.
Sensations of sweet, salty, bitter are transmitted to a certain part of the GM cortex through the nerves: glossopharyngeal (IX), facial (YII), vagus (YIII). Taste bioimpulses travel through nerve fibers to the thalamus, then to the guardian region of the GM cortex.
Damage to these nerves and the central parts of the brain (tumors, injuries, operations) provokes neural taste disorders:
- total ageusia, loss of the ability to distinguish taste (salty, sweet, etc.);
- ageusia partial;
- specific ageusia;
- dysgeusia (perverted taste).
Treatment of the disease
Treatment of nasociliary nerve neurosis consists of eliminating the disease that affects it.
In case of inflammatory processes in the ENT organs, patients are prescribed a course of treatment with antibiotics and a set of drugs that affect the elimination of inflammation and restoration of the mucous membrane, or surgical intervention (for pathologies of the nasal septum).
For vascular diseases, patients are prescribed drugs with antihypertensive and nootropic effects. Treatment is also carried out using vasoactive drugs.
To relieve pain and other symptomatic and clinical manifestations of neuralgia, local anesthetic drugs are used in medical practice in combination with non-narcotic painkillers and vasodilators. Their use is determined by which part of the nasociliary nerve has undergone pathological effects:
- For neuralgia of the long ciliary nerve, dicaine (0.25% eye solution) mixed with adrenaline (4 drops per 10 ml of solution) is used.
- For neuralgia of the subtrochlear region of the nasociliary nerve, cocaine hydrochloride (2% solution) mixed with 0.1% adrenaline (4 drops per 5 ml of the drug) is used. A solution of lidocaine is also used in the form of a spray, which is injected into the nasal passages on the corresponding side or both at once (for bilateral neuralgia) up to 4 times a day.
- If any part of the nerve is damaged, use a powder mixture of papaverine, glucose, antispasmodic, diphenhydramine and aminazine 2 times a day.
As an additional therapy for patients diagnosed with Charlin's syndrome, a course of intramuscular vitamin B12 is indicated, as well as intravenous administration of sulfonamide drugs.
Unpleasant chest pain is often a sign of heart disease. But a similar symptom is also characteristic of neuralgia. A competent specialist should be able to distinguish the signs of neuralgia in the heart area from heart pain. Read the article about how to treat this disease.
We will consider the causes and symptoms of trigeminal neuralgia in this topic.
Diagnosis of neuralgia
A neurologist is involved in differential diagnosis. Diagnosis of neuralgia begins with a neurological examination of a patient with typical complaints for this disease. The listed causes of neuralgia require a more complete examination to identify or exclude the underlying disease.
In some cases, additional instrumental examination (electroneurography) may be required if the cause of neuralgia was injury in the projection of the nerve. An MRI of the spine or any of the nerve plexuses may be required in the event of any volumetric impact on the nerve structures, as occurs with a herniated or protruded intervertebral disc or soft tissue tumors.