In the hemispheres of the brain
The cortex is a brain structure and a layer of gray matter that ranges from 1.3 to 4.5 mm in thickness. It is located on the periphery of each of the hemispheres, covering them. Its greatest thickness is located in the upper parts of the postcentral and precentral gyri, as well as the precentral lobe (lobules).
The cerebral cortex plays a vital role in the implementation of higher mental (nervous) activity of the whole organism. It makes up more than 80% of its total mass. In humans, on average, it is approximately 44% of the total volume of each hemisphere.
- Sections of the brain - their structure and functions
- Brain cells
- Structural features
- Pathologies and signs of damage to departments
- Tick-borne encephalitis
- Structure of the cerebral cortex
- Structure
- There is a bridge inside the skull
- White matter
- Study of brain development
The cerebral cortex is divided into four types:
- Paleocortex (ancient).
- Archicortex (old).
- Neocortex (new).
- Intermediate (consists of intermediate parts of the paleocortex and archicortex).
This membrane covers the entire brain and forms a fairly large number of grooves, which differ in depth and length. Between them there are convolutions of different sizes.
Today, the cerebral cortex and all other parts of it have been studied quite deeply. It is known which areas of the brain are responsible for certain processes in the body. However, there are still unanswered questions.
As can be seen from the above, bark is a term that has a large number of meanings that affect various areas of human life.
Treatment of frontal lobe damage
Treatment for frontal lobe damage is aimed at eliminating the cause of the injury. Your doctor may prescribe medications for an infection, perform surgery, or prescribe medications to reduce your risk of stroke.
Depending on the cause of the injury, treatment is prescribed that may help. For example, if a frontal injury occurs after a stroke, it is important to adopt a healthy diet and physical activity to reduce the risk of future stroke.
The drugs may be useful for people who have problems with attention and motivation.
Treatment of frontal lobe injuries requires ongoing care. Recovery from injury is often a lengthy process. Progress can come suddenly and cannot be completely predicted. Recovery is closely related to supportive care and a healthy lifestyle.
Sections of the brain - their structure and functions
The center of the nervous system is both a single “control unit” and a group of individual structures working harmoniously. The main parts of the brain, posterior, middle and anterior, perform certain functions, therefore they differ in structure and energy consumption. Even the cells that make up each area of the organ have their own structural features.
Posterior part of the brain
This area includes two structural units:
- Pons.
The continuation of the medulla oblongata, on the other hand, borders on the middle section. The task of the bridge is to transmit nerve signals. All pathways (ascending and descending) that connect the spinal cord with the forebrain, cerebellum and other parts of the organ pass through it. The pons contains the nuclei of the facial, trigeminal, and abducens nerves. It is responsible for many reflexes - eye reflexes, blinking, urination, intestinal motility and others.
Cerebellum
. Located under the occipital lobes of the cerebral hemispheres. The structure of the brain allows the cerebellum to communicate with neighboring sections through three pairs of “legs”. This structure occupies only 10% of the area, but contains more than half of all available neurons. The main functions of the cerebellum are autonomic regulation, coordination of movements, maintaining balance and muscle tone. Additionally, it supports the functioning of the gastrointestinal tract and cardiovascular system. In the last 10 years, studies have shown that the cerebellum is also involved in higher nervous activity - memory, thinking, and the accumulation of experience.
Medulla oblongata of the brain
Alternative names are myelencephalon and bulb. The section is a direct continuation of the spinal cord. It is located at the base of the skull in the back. The tasks of the bulb are to control breathing and circulatory processes. The structure of the brain and functions in this case are closely dependent, therefore, if the myelencephalon is damaged, its work is not compensated by other parts, and death occurs instantly. Additionally, the bulb helps maintain balance, metabolism, coordination and muscle activity, and communication with the senses.
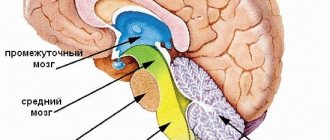
Middle part of the brain
One of the smallest structures, about 2 cm in diameter. Located between the hindbrain and diencephalon. The structure includes the following parts:
- roof (green);
- midbrain tegmental area (red);
- Sylvian aqueduct (black);
- legs (blue).
Its small size does not prevent this section from performing the most important functions of the brain, which are often mistakenly attributed to the hemispheres:
- general level of excitation of the central nervous system;
- hearing;
- vision;
- concentration of attention;
- defensive, orientation and protective reflexes;
- movement control;
- maintaining normal body temperature.
In the described department, dopamine is produced, so the midbrain regulates:
- emotional activity;
- reproductive behavior and excitability;
- level of motivation;
- development of habits and addictions, including addictions;
- pain sensitivity;
- cycles of sleep and wakefulness.
Forebrain
The structure of this part of the central nervous system includes the diencephalon and the cerebral hemispheres. Other names are diencephalon and telencephalon. The diencephalon is the “substrate” of the hemispheres, but has a complex structure:
- Thalamic brain.
Includes the thalamus, epithalamus and subthalamus. - Hypothalamic department (hypothalamic-pituitary system).
It includes the posterior lobe of the pituitary gland and the hypothalamus.
The diencephalon performs many important functions in the body. It regulates:
- body temperature;
- sleep and wakefulness patterns;
- thirst and hunger;
- feeling of fullness;
- neurohumoral processes;
- the work of the endocrine glands;
- hormone production.
The telencephalon consists of the right and left hemispheres. They are connected to each other by transverse nerve bundles (commissures). The main “bridge” between the hemispheres is the plate of the corpus callosum. In popular psychology, the assertion is promoted that the structure of the telencephalon implies the separate work of its halves. One is responsible for logic and rationality, the other for creativity and imagination.
Modern scientific research refutes the theory of asymmetry. Both hemispheres of the brain simultaneously take part in higher nervous activity. The distribution of tasks is uneven, but the differences are insignificant. Functions of the telencephalon:
regulation of movements; vision; speech; musculocutaneous sensitivity; sense of smell; hearing; taste sensations; thinking; logics; attention; memory; education; formation of emotions and others.
General information
Formed from the anterior end of the primary neural tube. In embryogenesis, it is divided into 2 parts, one of which gives rise to the telencephalon, the second - the intermediate brain.
According to Alexander Luria’s model, it consists of 3 blocks:
- Block regulating brain activity levels. Ensures the implementation of certain types of activities. Responsible for emotional reinforcement of activity based on predicting its results (success - failure).
- Block for receiving, processing and storing incoming information. Participates in the formation of ideas about ways to implement activities.
- Block of programming, regulation and control over the organization of mental activity. Compares the resulting result with the original intent.
The forebrain takes part in the work of all blocks. Based on information processing, it controls behavior. Administrator of higher psychological functions: perception, memory, imagination, thinking, speech.
Brain cells
The brain is made up of two types of cells: nerve cells (neurons) and glial cells.
Nerve cell
Neurons come in many sizes and shapes, but they all consist of a cell body, dendrites, and an axon. A neuron transmits information through electrical and chemical signals. Try to imagine the electrical wiring in your home. An electrical circuit consists of numerous wires connected in such a way that when a light switch is turned on, a light bulb will glow. An excited neuron will transfer its energy to neurons in its immediate vicinity.
Important Causes, symptoms and types of tachylalia
Neurons transmit their energy, or “speak,” to each other through a tiny gap called a synapse (Figure 12). A neuron has many arms called dendrites, which act like antennas that collect messages from other nerve cells. These messages are passed to the cell body, which determines whether the message should be passed along.
Important messages are carried to the end of the axon, where sacs containing neurotransmitters open into the synapse. Neurotransmitter molecules cross the synapse and are placed into special receptors on the receiving nerve cell. This stimulates the cell to transmit the message.
Figure 12. Nerve cells consist of a cell body, dendrites, and an axon. Neurons communicate with each other by exchanging neurotransmitters through a tiny gap called a synapse.
Glial cells
Glia (Greek word meaning glue) are brain cells that provide neurons with nutrition, protection, and structural support. There are approximately 10-50 times more glia than nerve cells and are the most common cell type involved in brain tumors.
Structural features
The frontal lobes are a part of the brain that is responsible for communication skills (the ability to talk, think, remember). The anatomical structure of the frontal lobe suggests a clear limitation from the temporal regions by the lateral grooves. On the frontal side, the frontal part is separated from the parietal area by the central sulcus. The lower edge of the section is limited by the Sylvian fissure.
The main gyri located in the frontal lobe include the vertical precentral and superior, middle, inferior, running horizontally. The gyri are separated by grooves. During wakefulness, neurons and neurotransmitters in this area are more active than during sleep.
The area of the prefrontal cortex is functionally connected and actively interacts with parts of the limbic nervous system - brain structures located on both sides of the thalamus. The limbic system is involved in regulating the sense of smell, the functioning of internal organs, the expression of emotions, sleep and wakefulness, and memory.
The hypothalamus, part of the limbic system, controls the autonomic nervous system with the help of hormones, due to which a person feels thirst and hunger, wakes up and falls asleep in accordance with nature’s biological clock, and experiences sexual attraction to members of the opposite sex. The hippocampus is involved in the process of forming the base of long-term memory. This structure is responsible for the perception, analysis and storage of spatial information.
The frontal lobe is considered the cortical region of the limbic system. In the frontal part of the brain there are association zones where information received from outside is processed and compared with data stored in memory. The anatomy of this brain structure involves division into sections:
- Motor.
- Premotor.
- Dorsolateral prefrontal.
- Medial prefrontal.
- Orbitofrontal. It is the intersection of neural pathways through which information is transmitted to the associative zones of the cortex - a place of close interaction between the prefrontal and limbic systems.
The prefrontal region regulates complex behaviors and patterns, ensuring the interconnection of motivational, emotional and thought processes. The department participates in assessing the environment, taking into account the circumstances, formulating the order of planned actions, analyzing the consequences of planned actions, and developing typical behavior patterns for specific situations.
Functions of the cortex
The human cerebral cortex is responsible for controlling many functions that are used in different aspects of the human body. Its thickness is about 3-4 mm, and its volume is quite impressive due to the presence of channels connecting the central nervous system. How perception, information processing, and decision-making occur through an electrical network using nerve cells with processes.
Various electrical signals are produced within the cerebral cortex (the type of which depends on the current state of the person). The activity of these electrical signals depends on the person’s well-being. Technically, electrical signals of this type are described in terms of frequency and amplitude. A larger number of connections and neurons are localized in places that are responsible for ensuring the most complex processes. At the same time, the cerebral cortex continues to actively develop throughout a person’s life (at least until his intellect develops).
In the process of processing information entering the brain, reactions (mental, behavioral, physiological, etc.) are formed in the cortex.
The most important functions of the cerebral cortex are:
- The interaction of internal organs and systems with the environment, as well as with each other, the correct course of metabolic processes within the body.
- High-quality reception and processing of information received from the outside, awareness of the information received due to the flow of thinking processes. High sensitivity to any information received is achieved due to a large number of nerve cells with processes.
- Supporting a continuous relationship between various organs, tissues, structures and systems of the body.
- Formation and proper functioning of human consciousness, the flow of creative and intellectual thinking.
- Exercising control over the activity of the speech center and processes associated with various mental and emotional situations.
- Interaction with the spinal cord and other systems and organs of the human body.
The cerebral cortex in its structure has the anterior (frontal) sections of the hemispheres, which are currently least studied by modern science. These areas are known to be virtually impervious to external influences. For example, if these sections are influenced by external electrical impulses, they will not give any reaction.
Some scientists are confident that the anterior sections of the cerebral hemispheres are responsible for a person’s self-awareness and his specific character traits. It is a known fact that people whose anterior sections are affected to one degree or another experience certain difficulties with socialization, they pay practically no attention to their appearance, they are not interested in work activity, and are not interested in the opinions of others.
From a physiological point of view, the importance of each section of the cerebral hemispheres is difficult to overestimate. Even those that have not yet been fully studied.
Pathologies and signs of damage to departments
Extensive damage to the medial areas of the frontal lobe provokes the development of abulia, which is manifested by slow reactions, indifference, and indifference to what is happening. If an area of the prefrontal orbital cortex is damaged, the patient experiences a lack of critical assessment of his own behavior and emotional lability.
Bilateral injury in the frontal region is accompanied by signs: agitation, restless behavior, obsessiveness, verbosity. Abnormal behavior is a sign of dementia, which develops against the background of degenerative processes affecting the frontal lobes. Damage to the motor cortex medulla causes hemiparesis, or muscle weakness.
Disorders develop on the side opposite to the location of the pathological focus in the brain. Damage to the visual area in one hemisphere leads to the development of bilateral blindness in half the visual field. A lesion in area 19 is associated with visual agnosia, a disturbance in visual perception. The patient sees an object, but cannot recognize it.
The information that comes through the visual analyzer is not processed or processed incorrectly, which leads to the inability to distinguish between familiar objects and people's faces. In such patients, color perception is impaired - they cannot distinguish shades.
Damage to field 22 leads to the development of musical deafness (impaired perception of musical works), the appearance of auditory hallucinations, and impaired reactions focused on auditory stimuli. Damage to field 41 is accompanied by the development of cortical deafness (inability to perceive sound signals).
Damage to field 34 is accompanied by impaired perception of smells, including olfactory hallucinations. Pathological structural changes in the nerve tissue of area 39 lead to the inability to read and write. When the field tissue is damaged, 37 people do not remember the names of objects.
Areas of the brain are divided into sensory and motor, as well as associative - and all areas interact with each other. Each department is endowed with certain functions, which together determine higher mental and complex motor activity.
PsyAndNeuro.ru
The history of the study of psychomotor disorders since its beginning in the early years of the 19th century is a complex and confusing sequence of successive paradigms and concepts. It all started with Wilhelm Griesinger, who first introduced the concept of “psychomotor disorders.” However, his followers combined slightly different things under this term: Emil Kraepelin - sensorimotor disorders, Karl Kahlbaum and August Hoch - the psychomotor concept of catatonia, Gilles de la Tourette - involuntary movements, Jean-Martine Charcot and Pierre Marie - motor symptoms of hysterical paralysis. Carl Wernicke and Karl Kleist then described the so-called “motor” and “cycloid” psychoses as two distinct episodic states with their own psychomotor manifestations. However, in a surprisingly short time - with the advent of the first antipsychotics in the 1950s - the concept of truly psychomotor disorders was practically forgotten, and “all roads began to lead” to exclusively motor disorders. It was only in the 1960s that Karl Leonhard (a student of Karl Kleist) began to return attention to psychomotor disorders themselves.
Although psychomotor impairment is one of the key features of conditions such as major depressive disorder (MDD), bipolar affective disorder (BD) and schizophrenia, the generally accepted modern diagnostic classifications (ICD-10 and DSM-5) emphasize cognitive , affective and social symptoms, but not psychomotor ones. The RDoC dimensional classification still addresses motor symptoms of mental illness, but still places an emphasis on exclusively motor-related changes in dopaminergic cortico-striato-pallido-thalamo-cortical motor pathways. In contrast to these approaches, in our work we set a goal to revive the concept of a truly “psycho-motor” in the literal sense of the word, showing specific psychomotor (and not just motor) mechanisms.
What exactly do we mean by the term “psychomotor”? Obviously, this word consists of two parts: “psycho” and “motor”. In contrast to the reduction of the first component, i.e. “psyche”, for the sake of the second, i.e. “motor”, as often happens, we tried to directly assess the direct connection between mental and motor functions and consider the neurobiological mechanisms underlying this connection. At the neuronal level, psychomotor mechanisms determine how primary motor functions (i.e., dopaminergic subcortical-cortical pathways) are modulated by non-motor functions, i.e., cognitive and emotional systems. From a psychological point of view, psychomotor mechanisms determine body movements as a result of some mental activity, which is necessary for interaction with the environment and objects. This view is consistent with the original understanding of “psychomotor,” which emphasizes the very interaction of affective, cognitive, and motor functions. As indicated in the title of our work, we will show the pathophysiological mechanisms by which affective and cognitive changes that are not connected to motor areas in one way or another (i.e., by different roads) lead to dysfunction of the motor cortex and, accordingly, to the appearance of psychomotor symptoms .
In our work, we sought to revive the traditional understanding of psychomotor phenomena as something more than just motor disorders. Indeed, according to recent research, the neuronal and biochemical mechanisms underlying psychomotor disorders affect a much larger number of brain systems than just the dopaminergic basal-thalamo-cortical motor loop. We built our review not according to the traditional scheme, starting from nosologies, but, rather, following the RDoC concept, we grouped information according to various psychomotor syndromes.
In this paper, we present the results of MRI studies of MDD, bipolar disorder and schizophrenia, dedicated to the search for neurobiological correlates of psychomotor phenomena. We first focus on how exactly the dopaminergic subcortical-cortical motor system is modulated by other neurotransmitter systems, in particular the serotonin pathways (subcortical-cortical modulation). We then describe how the sensorimotor network (SMN) and related motor functions are modulated by other non-motor networks, in particular the brain's default mode network (DMN). We also describe how global cortical activity influences local motor cortical activity (i.e., corticocortical modulation).
Changes in the raphe nucleus modulate the activity of subcortical-cortical motor pathways
One important brainstem region influencing the dopaminergic motor network is the serotonergic raphe nucleus (RN). Since at present a fairly small number of studies have been published on the direct influence of the raphe nucleus on the motor cortex, in this section we also present data from fMRI studies of the raphe nucleus itself.
Han et al. in their study, they studied resting-state functional connectivity, rsFC (this term refers to the temporal correlation of changes in the activity of different areas of the brain; that is, two areas are considered more functionally connected if their excitation patterns are more synchronized, provided , that both of these areas are parts of the same functional network - the raphe nucleus) with other areas of the brain in patients with bipolar disorder and MDD. It turned out that in bipolar disorder and in MDD, opposite patterns of rsFC of the raphe nucleus with other subcortical regions, in particular with the thalamus and putamen, are observed. In addition, in bipolar disorder, rsFC of the hypothalamus was increased, and in depression, on the contrary, it was decreased. These findings were supported by the results of a study by Anand et al., which found a significant decrease in rsFC of the raphe nucleus with the prefrontal cortex and middle cingulate cortex in MDD. In addition, rsFC of the raphe nucleus with the hippocampus and amygdala was correlated with the severity of depressive symptoms. Finally, Wohlschlager et al. went further with rsFC studies and studied the spectral characteristics of infraslow oscillations (0.01-0.1 Hz) in the activity of the raphe nucleus and ventral tegmental area (VTA) in patients with MDD who did not receive therapy. It was found that in both areas there was a significant increase in lower frequency activity, which also directly correlated with the severity of depressive symptoms.
All these data indicate that in depression there are certain changes in the raphe nucleus itself, as well as in its connections with subcortical motor areas (thalamus and basal ganglia) and various non-motor areas of the cortex. However, at present there are very few studies devoted to possible functional changes in the raphe nucleus and its rsFC, as well as serotonergic dysfunction, in schizophrenia. However, the above studies suggested that abnormalities in the functional connections of the raphe nucleus (as the central structure of the serotonergic system) with other subcortical and cortical regions may be transdiagnostic phenomena. All this leaves open the question of the connection of these abnormalities with motor function and especially with psychomotor symptoms.
Modulation of dopamine subcortical-cortical motor pathways by the raphe nucleus and serotonin in the healthy brain.
Does the serotonin raphe nucleus influence dopaminergic subcortical-cortical pathways and motor functions? Conio et al. based on pharmacological, structural and functional MRI studies, demonstrated the presence of complex interactions between serotonin and dopamine, as well as the influence of these interactions on brain activity. In particular, it has been shown that the dopaminergic substantia nigra is connected mainly with the sensorimotor network (and the VTA with the salience network (SAN). However, the serotonergic raphe nucleus has connections with both the sensorimotor network and the passive mode network brain. In addition to the various connections between the dopamine and serotonin nuclei of the brainstem, the activity of dopamine pathways leads to increased SMN activity, and the activity of serotonergic pathways, on the contrary, leads to a decrease in SMN activity and an increase in DMN activity. Moreover, substantia nigra rsFC was directly correlated with SMN activity, and rsFC of the raphe nucleus was inversely correlated with SMN activity.Martino et al., in their study showed that in healthy subjects, rsFC between the thalamus and SMN was modulated by functional connections from both the raphe nucleus and the substantia nigra, but in the opposite way. In other words, connections from the substantia nigra contribute to greater synchronization of activity between the thalamus and SMN, and connections from the raphe nucleus, on the contrary, reduce this synchronization. Thus, based on these data, it can be argued that serotonin in the raphe nucleus and dopamine in the substantia nigra have diametrically opposite effects on the activity of the motor cortex, in particular on the SMN. Dopamine signals increase SMN activity and its synchronization with the activity of the thalamus, while serotonin signals, on the contrary, lead to “anti-correlation” of the SMN and thalamus and a decrease in SMN activity.
Thus, in answer to the question posed at the beginning of this section, it can be argued that the raphe nucleus and serotonin do indeed modulate dopamine subcortical-cortical pathways. Accordingly, dopamine pathways from the substantia nigra and serotonin pathways from the raphe nucleus may not be regarded as primary motor pathways per se, but rather as modulators of psychomotor functions.
Modulation of dopamine subcortical-cortical motor pathways by the raphe nucleus and serotonin in depression, bipolar disorder and schizophrenia.
Based on data obtained in healthy subjects, it can be assumed that psychomotor inhibition, which is based on reduced SMN activity, should be due to a decrease in substantia nigra rsFC and/or an increase in raphe nucleus rsFC. Similar phenomena are indeed observed in patients with psychomotor inhibition in the depressive phase of bipolar disorder. Such patients are characterized by a decrease in rsFC of the thalamus and SMN and substantia nigra with the thalamus/basal ganglia, as well as a competitive decrease in rsFC of the raphe nucleus with the basal ganglia/thalamus. Together, these patterns promote “decoupling,” that is, desynchronization of thalamic and SMN activity, with subsequent inhibition of SMN activity and the occurrence of psychomotor inhibition. These findings are consistent with the results of a study by Yin et al., which demonstrated decreased blood flow in the motor cortex during psychomotor inhibition in patients with MDD.
For patients with mania, on the contrary, almost diametrically opposite changes are characteristic. These patients showed a decrease in rsFC of the raphe nucleus with the thalamus/basal ganglia, and also, unlike patients with depression, rsFC of the substantia nigra was preserved. Taken together, this leads to an increase in rsFC of the thalamus with the SMN, increased SMN activity and subsequent psychomotor agitation.
Thus, the data from these studies suggest a reciprocal balance between the dopaminergic connections of the basal ganglia/thalamus to the SMN on the one hand and the serotonergic modulation of these connections by the raphe nucleus on the other hand. A decrease in the activity of serotonergic pathways from the raphe nucleus to the basal ganglia leads to greater “connectivity” of the thalamus with the SMN, which leads to psychomotor agitation. A decrease in the activity of dopaminergic pathways from the substantia nigra to the basal ganglia, on the contrary, reduces the “connectivity” of the thalamus with the SMN and leads to the occurrence of psychomotor inhibition. If these two arms of modulation of thalamus-SMN connections, dopaminergic and serotonergic, are balanced, then psychomotor function is “normal”, that is, neither accelerated nor slowed down. If this balance is disturbed, then the thalamus and SMN become either overly or underfunctionally connected, leading to either psychomotor agitation (for example, in mania) or psychomotor inhibition (in depression). See Fig. for details. 1A.
Rice. 1. Biochemical and neuronal modulation of subcortical-cortical and cortico-cortical mechanisms of psychomotor phenomena. A. Modulation of the dopaminergic subcortical-cortical motor circuit by the raphe nucleus and serotonin. B. Modulation of the sensorimotor network (SMN) by the passive mode network (DMN). C. Modulation of the display of general activity in the SMN. SN – substantia nigra, RN – raphe nucleus, Thal – thalamus.
Modulation of the dopamine subcortical-cortical motor loop by the raphe nucleus/serotonin and other neurotransmitter systems - a dimensional and transnosological approach
The next question to be answered is: can serotonin modulation of the motor loop be correlated with different diagnostic categories, or, put another way, can it be correlated with different degrees of psychomotor impairment? A kind of “litmus test” that can help answer these questions is the phenomenon of psychomotor agitation in depression. Martino et al. We separately studied patients in the depressive phase of bipolar disorder with psychomotor agitation and compared them with corresponding patients with psychomotor inhibition. It turned out that in depressed patients with psychomotor agitation, a pattern similar to that observed in mania is observed: in both conditions, there is an increase in rsFC of the thalamus with the SMN, which, accordingly, leads to increased SMN activity and psychomotor agitation.
Further evidence of the dimensional and transnosological nature of bilateral “from the raphe nucleus and from the substantia nigra) modulation of the activity of the subcortical-cortical motor loop follows from the results of a recent study of schizophrenia. The authors studied two groups of patients with schizophrenia - with psychomotor agitation and with psychomotor inhibition - and compared them, respectively, with groups of patients with bipolar disorder in the manic phase (and with psychomotor agitation) and in the depression phase (with concomitant psychomotor inhibition). It turned out that patients suffering from schizophrenia with psychomotor inhibition are characterized by almost the same pattern of changes in thalamo-sensorimotor rsFC as patients suffering from depression with psychomotor inhibition, that is, a decrease in rsFC of the thalamus with SMN and a concomitant decrease in rsFC of the raphe nucleus and nigra substances with the basal ganglia and thalamus. A similar overlap was observed in patients suffering from schizophrenia with psychomotor agitation. The increase in rsFC of the thalamus with SMN and the decrease in rsFC of only the raphe nucleus with the basal ganglia and thalamus observed in such patients are similar to the corresponding changes in patients in the manic phase of bipolar disorder with psychomotor agitation.
A textbook example of a psychomotor syndrome is catatonia, which is a truly transdiagnostic phenomenon. Catatonia can occur in schizophrenia, bipolar disorder, MDD, and other diseases. The development of catatonia is the result of dysfunction of several neurotransmitter systems. Indeed, catatonia is primarily manifested by motor disorders associated with changes in the activity of sensorimotor subcortical-cortical zones. However, catatonia is also characterized by affective disturbances associated with changes in non-motor areas of the cortex (for example, with dysfunction of frontoparietal connections), which emphasizes the truly psychomotor nature of this phenomenon. Accordingly, along with hypoactivation of dopaminergic receptors, disturbances in other neurotransmitter systems are observed in catatonia: hypoactivation of serotonin (5-HT2A) receptors, an imbalance between the activity of GABAA (hypoactivation) and GABAB (hyperactivation) receptors and, probably, also hyperactivation of glutamate NMDA receptors. On the one hand, lorazepam and zolpidem (allosteric modulators of GABAA receptors) increase the excitability of GABAergic inhibitory networks in the motor cortex and thus help alleviate the symptoms of catatonia. On the other hand, baclofen and valproic acid can increase the activity of GABA and NMDA receptors and, conversely, increase the severity of catatonia. However, there is still some evidence of a beneficial effect of valproic acid, topiramate, and carbamazepine on affective catatonic symptoms (presumably by increasing GABA and NMDA responsiveness). Finally, clozapine (a 5-HT2A receptor antagonist and GABAA receptor agonist) compensates for the serotonergic hypoactivation imbalance of GABAA-B activity and thus may reduce the severity of catatonia in some studies.
Another example of a transnosological psychomotor syndrome is parkinsonism (a combination of tremor, rigidity and bradykinesia), which is mainly a consequence of Parkinson's disease, which is primarily neurodegenerative in nature. However, the phenomena of parkinsonism can also be associated with other diseases (for example, parkinsonism can be observed in patients with schizophrenia). Parkinson's disease is primarily characterized by degeneration of dopaminergic cells in the substantia nigra and striatum, but the disease has also been found to impair the activity of the serotonergic system. Thus, in Parkinson's disease, there is a decrease in the number of serotonin transporters in the raphe nucleus, which is directly associated with the severity of tremor. In addition, other neurotransmitter systems are also affected in Parkinson's disease. It is known that GABAergic system modulators (zolpidem and clonazepam), amantadine, anticholinergic drugs and clozapine can improve the motor symptoms of Parkinson's disease. Patients with schizophrenia and Parkinsonism exhibit characteristic changes in gray matter volume and activity in frontothalamic/cerebellar and cortical somatosensory networks that are not found in patients without Parkinsonism. These facts make it possible to assume the existence of ascending modulation of the motor cortex as a central neuronal mechanism for the occurrence of parkinsonism in schizophrenia.
Finally, psychomotor impairments can also be observed in other diseases, in particular in autism. It is worth noting that there is evidence of changes in the activity of the dopaminergic, serotonergic (increased synthesis of serotonin), GABAergic and glutamatergic systems in the motor and somatosensory cortex, as well as in the striatum, associated with this disorder. Accordingly, dopamine receptor blockers, serotonin reuptake inhibitors, memantine, valproic acid, arbaclofen, and acamprosate have been shown to be effective in reducing psychomotor symptoms of autism such as stereotypies, impulsivity, and irritability in some studies.
Taken together, these results clearly demonstrate that modulation by the raphe nucleus and serotonin of the subcortical-cortical motor loop represents a phenomenon that extends beyond any specific disease category. It corresponds rather to the direction and severity of psychomotor disorders, rather than to any specific diagnosis, thus being a truly dimensional and transnosological phenomenon.
Modulation of the motor loop by other cortical networks
The cerebral cortex includes various neural networks: the passive mode network (DMN), sensory networks (visual, auditory, somatosensory), sensorimotor network (SMN), frontoparietal network, salience network, attention networks and many others. Recent studies have shown that all these networks are functionally interconnected. For example, the DMN and the frontoparietal network are opposite in their activity: a functional increase in the activity of one directly leads to inhibition of the activity of the other and vice versa. Most interestingly, the SMN also appears to be in reciprocal relationships with other networks, particularly the DMN and sensory networks. In a study by Martino et al. It has been demonstrated that an increase in neuronal variability in the DMN is associated with a decrease in this parameter in the SMN, even in healthy individuals.
Just as in the case of subcortical modulation, this reciprocal interaction is extremely pronounced in patients with bipolar disorder in the phase of depression and mania. Patients in the depressive phase exhibit abnormally high neuronal variability in the DMN, which, following a reciprocal mechanism, was accompanied by a decrease in neuronal variability in the SMN. Changes in these parameters correlated with the severity of symptoms: the greater the neuronal variability in the DMN compared to the SMN, the more severe the depressive symptoms were. Interestingly, in patients in the manic phase, on the contrary, neuronal variability in the DMN was reduced and, accordingly, increased in the SMN. This also correlated with manic symptoms: the greater the variability of the SMN compared to the DMN, the more severe the patient's manic symptoms. It is worth emphasizing that it was the ratio of DMN/SMN variability that correlated with the severity of symptoms, but not the absolute values of these indicators themselves.
In another study, Northoff et al. examined neuronal variability in the SMN and visual network in patients with bipolar disorder. The authors found that during mania, an increase in variability in the SMN was accompanied by a decrease in that in the visual network. The opposite picture was observed in depression: a decrease in variability in the SMN and an increase in that in the visual network. The authors associated this balance with “internal” and “external” perceptions of time speed. “Internal” perception was determined by the activity of the SMN and the subcortical-cortical motor loop, while “external” perception was determined by sensory areas, including the visual network. If we take the degree of neuronal variability as an indicator reflecting the perception of time (increased variability indicates a greater change in neuronal activity per unit of time and, accordingly, the “acceleration” of time at the neuronal level), then we can say that patients with depression tend to slow down “ internal" time, that is, abnormal "intrinsic slowing" (resulting from decreased neuronal variability in the SMN). In contrast, patients with mania are characterized by a subjective “acceleration” due to increased variability in the SMN. The question of how these anomalies of “internal time” are transformed into psychomotor disorders and whether they are transformed at all remains open.
These studies clearly demonstrate that neuronal activity in the motor cortex and SMN depends not only on the subcortical influences of the raphe nucleus and substantia nigra, but also on the activity of other, non-motor cortical networks. The clearest evidence for this is the reciprocal interaction between the DMN and SMN, as well as the modulation of the SMN by sensory networks. However, the mechanisms by which such reciprocal corticocortical modulation is associated with psychomotor performance remain to be explored.
Modulation of local-regional activity of the motor cortex by general cortical activity
Traditionally, we measure neuronal activity locally, that is, in a specific area (signal amplitude from the area), or in a specific network (synchronization between different parts of the network, assessed using rsFC). However, in addition to these local methods, there are also methods that assess brain activity in general. One such method is to determine rsFC between entire neural networks, for example, between the DMN and SMN. In addition, if you take all the inter-regional and inter-network connections together, you can get the so-called “global signal”, assessed using fMRI. The global signal is calculated as the average of all rsFCs across the entire brain and reflects the degree to which different regions and networks are synchronized with each other, that is, global brain synchronization. Research demonstrates that the degree to which a particular region or network is synchronized with the rest of the brain varies among different regions. For example, neuronal activity in the SMN is more synchronized with overall brain activity (and thus exhibits greater global signal on fMRI) than the DMN, whose regions appear to operate more separately, that is, desynchronized (as reflected by lower global signal on fMRI).
Currently, there are reports of global signal changes in various mental disorders. Yang et al. demonstrated that patients with schizophrenia have a significantly higher global signal compared to patients with bipolar disorder and healthy subjects. This means that global synchronization of activity between distinct brain regions/networks is abnormally high in patients with schizophrenia (however, in another study, Argyelan et al., in contrast, demonstrated decreased global synchronization in patients with schizophrenia). Moreover, it has been found that in schizophrenia, global activity becomes less synchronized with the activity of lower order regions/networks, especially sensory areas. On the contrary, global activity becomes more synchronized with the activity of higher order zones. Wang et al. supplemented these data by showing that the synchronization of individual networks with general brain activity is a dynamic, time-varying process: first, global activity is synchronized with sensory networks, then with the DMN, and then with other networks. This sequence of synchronization of global brain activity with distinct regions/networks appears to be disrupted in schizophrenia.
In another study, Zhang et al. studied the global signal in bipolar patients in manic, depressive and euthymic phases. It was found that in patients with bipolar disorder in the depressive phase there is increased synchronization of global brain activity with the hippocampus, which may be associated with more frequent “memory recall” of autobiographical memories. In addition, it turned out that in manic patients, global activity is highly synchronized with the activity of the motor cortex, which reflects the greater psychomotor activity characteristic of these patients. The latter finding particularly emphasizes that synchronization of global activity is a true psychomotor mechanism: changes in the motor cortex cause changes in overall brain activity unrelated to the subcortical-cortical motor loop.
This review has the following important limitations. Firstly, the reviewed works differ greatly from each other in terms of diagnostic groups, approaches to the definition of psychomotor disorders and neuroimaging techniques. Secondly, the variety of approaches and methods, coupled with a small number of studies, did not give us the opportunity to conduct a full-fledged ALE-meta-analysis (activation likelihood estimation - an approach to meta-analysis of neuroimaging studies, which consists in determining the likelihood that areas of high the activities of the cortex really coincide - approx.). Third, due to the diversity of terminology related to the concept of “psychomotor,” we may have missed some important studies. Based on the reasons listed above, we consider it necessary to conduct further transdiagnostic longitudinal neuroimaging studies of psychomotor disorders using standardized methods.
This review has demonstrated the different neuronal mechanisms underlying psychomotor symptoms in various mental illnesses. This is a kind of continuation of the classical view of psychomotor syndromes, which is relevant at the present time, since it has been demonstrated that the neuronal and biochemical mechanisms of the occurrence of psychomotor disorders are not limited to the dopamine subcortical-cortical motor loop. We identified three transdiagnostic neurobiological mechanisms underlying psychomotor performance. 1) modulation by serotonin and the raphe nucleus of the dopaminergic subcortical-cortical motor loop; 2) reciprocal balance between the passive mode network of the brain, sensorimotor and sensory networks; 3) local synchronization of the sensorimotor network with global brain activity.
These mechanisms are fundamentally quite similar. Firstly, all three mechanisms depend not on any absolute values, but on relative indicators, that is, on the balance between any parameters. We encountered three types of neural balance, relating to different levels of manifestation of psychomotor functions: 1) balance between rsFC of the raphe nucleus and the substantia nigra; 2) balance between the activity of the passive mode network of the brain and the somatosensory network; 3) balance between global brain activity and local activity of the somatosensory network. In addition, we have identified different types of biochemical balance, for example between dopamine and serotonin, shaping psychomotor functions through modulation of subcortical-cortical and cortico-cortical neural balances.
Secondly, the data we analyzed indicate the dimensional and transnosological nature of psychomotor mechanisms that occur not only in various diseases (for example, schizophrenia, bipolar disorder or depression), but also in normal conditions. Accordingly, psychomotor mechanisms illustrate the advantages of using a dimensional transnosological syndromic approach (as done, in particular, by the authors of RDoc)
Third, these examples demonstrate a continuum of healthy and pathological psychomotor states in which the same mechanism is involved, but manifested to varying degrees. Within this continuum, the normal corresponds to the average values, while the pathological conditions are located at opposite ends, thus forming an inverted U-shaped curve (see Fig. 2)
Fig.2. Inverted U-shaped continuum curves of different neurobiological mechanisms of psychomotor activity. A. A continuum of different types of balance between the functional connectivity of the raphe nucleus (RN) and substantia nigra (SN) with the thalamus (Thal) and its connection with the sensorimotor network (SMN), which determines its activity. B. A continuum of different types of balance between SMN activity and the passive mode network (DMN) that determines the level of SMN activity. C. Continuum of different types of balance between global brain activity (GA) and level of SMN activity.
Fourth, the inverted U-shaped curve demonstrates that it is the average indicators of various types of neurobiological balance that are most optimal. In contrast, extreme forms of imbalance are dysfunctional, leading to impaired psychomotor functions.
Fifth, from a clinical point of view, psychomotor disorders can be characterized by a specific set of symptoms, that is, a combination of certain motor, affective and cognitive disorders. For example, psychomotor agitation may be accompanied by emotional disturbances (eg, increased affect) and cognitive impairments (particularly impaired attention). At the same time, psychomotor inhibition is often accompanied by negative emotions and increased attention to oneself. Such symptom constructs suggest the existence of connections between the subcortical-cortical motor system and non-motor, affective and cognitive neural systems, as evidenced, for example, by the existence of reciprocal interactions between the SMN, DMN and sensory networks.
Finally, all of these mechanisms have potential diagnostic and therapeutic implications. They can be used for early diagnosis of borderline states and manifestations of mental illness, serve as potential biomarkers of therapeutic response and be targets of non-invasive methods of brain stimulation (transcranial magnetic stimulation, etc.) Despite the fact that these methods can stimulate different parts of the brain, all of them will in one way or another affect the activity of the subcortical-cortical motor loop and reduce the severity of psychomotor disorders. As with Rome, all roads ultimately lead to the motor cortex.
Author of the translation: Kibitov A.A.
Source: Northoff, G., Hirjak, D., Wolf, RC et al. All roads lead to the motor cortex: psychomotor mechanisms and their biochemical modulation in psychiatric disorders. Mol Psychiatry (2020). https://doi.org/10.1038/s41380-020-0814-5
Tick-borne encephalitis
This disease has a viral etiology and is preceded by an increase in temperature, the development of headaches and malaise, weakening of muscle tissue, which causes rigidity. With an advanced form of tick-borne encephalitis, the symptoms worsen: the patient often exhibits hallucinations and obsessions, he becomes aggressive and agitated, and suffers from seizures.
Measles
With the development of measles encephalitis, damage to the cerebral hemispheres is manifested by a sharp increase in temperature, confusion, as a result of which the patient cannot navigate in time and space, visual hallucinations and nervous excitability. Characteristic symptoms of measles encephalitis are also convulsions that develop in all parts of the body, paresis and weakness of the muscles of the limbs: there is a risk of coma.
Lethargic
If damage to the cerebral cortex is caused by the development of lethargic encephalitis, the patient’s temperature rises, speech deteriorates, and catatonia occurs - a pathological condition in which the body freezes in one position for several hours. Lethargic encephalitis is also characterized by symptoms such as apathy, malaise, and drowsiness caused by disruption of the daily routine.
Important Review and application of parapodiums for the rehabilitation of neurological patients
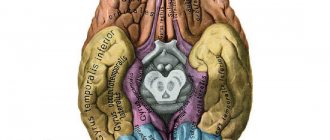
Structure of the cerebral cortex
The described section is the largest, it accounts for up to 80% of the total mass of the organ presented. The cerebral cortex is a layer of gray matter located on the surface and periphery of the cerebral hemispheres. It is responsible for higher nervous activity and most mental processes. The entire department is classified into 5 types of shares. Each of them has its own functions.
Frontal lobes
The anterior part of the cortex is separated from the parietal and temporal by two sulci (central and lateral). The frontal lobes of the brain consist of several main convolutions:
- precentral;
- superior frontal;
- middle frontal;
- inferior frontal.
The last gyrus is divided into 3 parts by small branches of the lateral sulcus:
- opercular;
- triangular;
- orbital.
What are the lobes of the brain in the frontal zone responsible for:
- motivation;
- inhibitory reflexes;
- purposeful (conscious) behavior;
- planning;
- fulfillment of assigned tasks;
- ability to write;
- speech;
- precision of movements.
Temporal lobes
The lateral zones have the most pronounced and clear boundaries. The structure of the brain in the presented lobes is separated by a lateral and two long temporal grooves (superior and inferior). Some areas are “cut up” by short transverse branches. The temporal lobes of the brain are divided into 3 main convolutions:
- lower;
- average;
- top.
Functions of this part of the cortex:
- hearing;
- visual memory;
- speech perception;
- formation of emotions;
- verbal memory;
- consciousness;
- perception and composition of music;
- processing of visual information.
Parietal lobes
The area shown is located at the top of the brain, towards the back of the brain. It is separated from other areas by the central and parieto-occipital sulcus. The main task of the part of the cortex under consideration is to analyze the surrounding space. The parietal lobes of the brain are divided into several areas, each of which has specific functionality:
- Primary somatosensory cortex.
Responsible for the perception and analysis of tactile sensations. It helps to correctly recognize objects, extract from memory knowledge about their structure, mass and shape. - Posterolateral parts of the parietal lobes.
They form visual-spatial relationships and combine them with other characteristics of objects. This zone ensures correct perception of the position and trajectories of movement of one’s body, limbs, and surrounding objects. - The medial parietal lobe is in the dominant hemisphere.
Functions – math skills, writing, understanding the difference between left and right sides, recognizing fingers. - Subdominant parietal lobe.
Regulates awareness of one’s own body and its parts, the relationship of objects in space, the ability to combine pieces into whole compositions, and the performance of simple mechanical tasks (dressing, combing, etc.).
Occipital lobes
This formation of the cortex is localized at the base of the skull, separated by lateral grooves. The tasks that the occipital lobes of the brain perform and their functions are determined by the nerve bundles in their structure. The structures responsible for vision are concentrated in the described area. The structure of the cerebral cortex of the occipital lobes includes 2 sections:
- zone of visual associations;
- primary visual cortex.
Basic functions:
- regulation of eye movements;
- obtaining visual information and processing it;
- image analysis;
- the ability to distinguish objects from each other visually;
- objective perception of reality.
Insula
The described part of the cortex is located deep in the lateral sulcus. So far this is the most unexplored area in terms of functions performed. Presumably the insular lobe of the brain is responsible for:
- formation of consciousness;
- the emergence of emotions;
- support of homeostasis;
- processing of any sensory information and its integration, analysis (visual, tactile, audio);
- motor control;
- empathy;
- speech;
- perception of heat, cold, satiety, fullness of the bladder;
- feeling of shortness of breath;
- equilibrium;
- reflex reactions (laughter, crying);
- movement training;
- social emotions (disgust, norms of behavior and others);
- orgasm.
Structure
The morphological structure of the cerebral hemispheres within the brain suggests the presence of a cortical layer consisting of gray matter and subcortical sections formed by white matter. Within the mass of white matter there are local areas of gray - the nuclei. White matter serves as the basis for nerve fibers:
- Associative. They unite different functional areas within one hemisphere.
- Commissural. They connect areas of different hemispheres, often symmetrically located.
- Conductive. They connect the parts of the brain - the brain and the spinal cord - thereby forming a single central nervous system network.
The structure of the cortex covering the cerebral hemispheres suggests the presence of grooves (depressions relative to the surface) and convolutions (elevations relative to the surface). In anatomy, the area of the cortex covering the cerebral hemispheres increases due to the presence of grooves. The duration and depth of the furrows are individual characteristics of a person.
The cortical layer, formed from gray matter, contains control centers that are responsible for higher mental functions, which are interconnected with processes such as cognitive and mental activity. The cortex, covering the cerebral hemispheres within the brain, coordinates the functions of the body, forming adaptive responses to external influences. The cortex is formed by 6 types of cells.
The cytoarchitectonics (location of cells in the tissue) of the cortex suggests the presence of molecular, granular (external, internal), pyramidal (external, internal), multiform plates. Within the brain, the surfaces of the hemispheres are distinguished: superolateral (covers the upper lateral areas), medial (located in the middle region), basal (adjacent to the base of the skull).
The superolateral surface has a convex shape and is adjacent to the bone structures that form the cranial vault. The flat medial surface is located opposite the similar surface of the second hemisphere. Each hemisphere consists of 5 lobes. The frontal lobe of the cortex, covering the cerebral hemispheres, is the largest part of the telencephalon. The central sulcus, anatomically transversely crossing the brain, is the border between the frontal and parietal lobes within the cerebral hemispheres.
The Sylvian fissure, also known as the lateral fissure, runs within the cerebral hemispheres perpendicular to the central one, separating the temporal lobe of the telencephalon from two segments - the frontal and parietal. The parieto-occipital sulcus is the border of the parietal segment on the posterior side. The insular lobe within the hemispheres of the brain is located deep in the Sylvian fissure. The insular lobe is visible if you lift the areas of the frontal and temporal lobes that cover it.
3 important signs of the development of pruritus syndrome after a fracture
The Sylvian fissure, also known as the lateral fissure, which separates the temporal lobe from the brain structures of the frontal and parietal, is one of the largest. It is formed at the 14th week of intrauterine development. Small grooves dividing the lobes of the cerebral cortex into convolutions are formed at 24-38 weeks, forming a peculiar relief of the surface of the hemispheres, individual for each person.
The sulci and gyri of the 3rd order continue to develop after birth, most intensively in the 1st year of life. In the frontal lobe of the cortex within the cerebral hemispheres, a precentral groove runs parallel to the central one, separating and limiting the precentral gyrus - the center where the initiation and regulation of conscious motor activity, directed by volitional effort, occurs.
The precentral gyrus is perpendicularly crossed by the frontal sulci (superior, inferior). They divide the frontal gyri into segments. In the posterior part of the frontal gyrus, located below, there is Broca's center, which is responsible for speech function. In the parietal lobe, the postcentral sulcus runs parallel to the central one.
The postcentral gyrus, located between these grooves, is a center of sensitivity, which is responsible for the body’s reactions to pain, tactile, and temperature influences. The temporal grooves (superior, inferior) lie in the temporal lobe and are located parallel to the Sylvian fissure.
The temporal sulci are divided into segments by the temporal gyri, where in the upper part there is a center responsible for hearing function and Wernicke's center, responsible for speech function. The calcarine groove, which provides visual function, lies in the occipital lobe, where it borders on the parieto-occipital groove.
Literature
- Collins A., Koechlin E. Reasoning, learning, and creativity: frontal lobe function and human decision-making //PLoS biology. – 2012. – T. 10. – No. 3. – P. e1001293.
- Chayer C., Freedman M. Frontal lobe functions // Current neurology and neuroscience reports. – 2001. – T. 1. – No. 6. – pp. 547-552.
- Kayser AS et al. Dopamine, corticostriatal connectivity, and intertemporal choice // Journal of Neuroscience. – 2012. – T. 32. – No. 27. – pp. 9402-9409.
- Panagiotaropoulos TI et al. Neuronal discharges and gamma oscillations explicitly reflect visual consciousness in the lateral prefrontal cortex // Neuron. – 2012. – T. 74. – No. 5. – pp. 924-935.
- Zelikowsky M. et al. Prefrontal microcircuit underlies contextual learning after hippocampal loss // Proceedings of the National Academy of Sciences. – 2013. – T. 110. – No. 24. – pp. 9938-9943.
- Flinker A. et al. Redefining the role of Broca's area in speech //Proceedings of the National Academy of Sciences. – 2015. – T. 112. – No. 9. – pp. 2871-2875.
There is a bridge inside the skull
A diagram of the structure of the brain shows that another component, the pons, is located below the peduncles and forms a prominent protrusion (due to transverse fibers directed into the cerebellum). In the anterior zone of the bridge there are predominantly conductive pathways. Namely: the path of the auditory nerve nuclei, the aforementioned pyramidal (motor, cortico-muscular), general sensory (from the spinal cord to the visual thalamus, medial lemniscus), etc.
The structure of the human brain includes such an element as the cerebellum. It is located above the medulla oblongata in the posterior cranial fossa. Covered on top by the occipital lobes of the cerebral cortex. The cerebellum has two hemispheres and a central part - the vermis. In a newborn, this organ weighs 20 grams, by five months the weight increases 3 times, by nine months - 4 times.
The final formation of this organ is completed by the age of 15. The surface of the hemispheres is gray matter - the cortex, under which lies the white matter. The organ has three pairs of legs connecting it with other parts: the lower pair - with the medulla oblongata, the middle one - with the pons, the upper one - with the midbrain.
White matter
It is presented in the form of numerous fibers. They are divided into three groups:
- Projection. This category is represented by bundles of efferent and afferent fibers. Through them, there are connections between the projection centers and the basal, stem and spinal nuclei.
- Associative. These fibers provide connection to the cortical areas within the boundaries of one hemisphere. They are divided into short and long.
- Commissural. These elements connect the cortical zones of the opposite hemispheres. Commissural formations are considered: the corpus callosum, posterior and anterior commissure and commissure of the fornix.
Prefrontal cortex
A large section of the cerebral cortex, which is represented in the form of the anterior sections of the frontal lobes. With its help, control, management, and focusing of any actions that a person performs are carried out. This department allows us to properly distribute our time. The famous psychiatrist T. Galtieri described this area as a tool with the help of which people set goals and develop plans. He was confident that a properly functioning and well-developed prefrontal cortex was the most important factor in a person’s effectiveness.
The main functions of the prefrontal cortex also include:
- Concentration, focusing on obtaining only the information a person needs, ignoring other thoughts and feelings.
- The ability to “reboot” consciousness, directing it in the right thinking direction.
- Perseverance in the process of performing certain tasks, the desire to achieve the intended result, despite the emerging circumstances.
- Analysis of the current situation.
- Critical thinking, which allows you to create a set of actions to search for verified and reliable data (checking the information received before using it).
- Planning, development of certain measures and actions to achieve set goals.
- Forecasting events.
The ability of this department to control human emotions is especially noted. Here, the processes occurring in the limbic system are perceived and translated into specific emotions and feelings (joy, love, desire, grief, hatred, etc.).