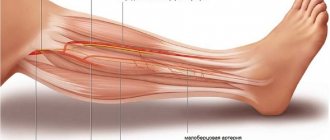
Pain in the foot or toes can be caused by a variety of factors, including pathologies of the osteoarticular apparatus itself and the soft tissues of the foot. But for no apparent reason, pain most often has a vertebrogenic origin, since it occurs with dystrophic-degenerative changes in the lumbosacral spine.
We are faced with pain in the foot and toes due to radicular syndrome - pinching of the fibers of the spinal nerves in the area of their exit from the spinal canal . In addition, foot pain can result from pinching of the sciatic nerve along its length. In any case, this manifestation requires careful diagnosis and treatment measures. Experienced clinic specialists provide appointments daily, after prior appointment .
Why does pathology occur?
Doctors consider primary and secondary neuropathy. The primary cause is injuries, infectious diseases and hypothermia. The list of reasons that can cause a secondary type of illness is much more extensive. These include:
- disc displacement;
- neoplasms of any nature;
- osteochondrosis;
- protrusion;
- osteophytes;
- spasmodic muscles;
- curvature of the ridge;
- tunnel syndrome;
- intervertebral hernia;
- post-injection suppuration.
Symptoms of inflammation of the sciatic nerve
Pain, which can even occur due to lifting a heavy bag or hypothermia, night attacks are the main indicator of sciatica. In addition to the sharp shooting pain syndrome, doctors advise paying attention to:
- “pins and needles” and numbness from the buttocks and below;
- constipation, urinary incontinence;
- weakness and gradual muscle atrophy, limping.
When a person moves or stands for a long time, pain is more disturbing. During attacks, redness of the skin, swelling, chills, and sweating are quite possible. At first, the pain syndrome is not very expressive, but gradually becomes so strong that there is a danger of loss of consciousness. It almost hurts for a person to breathe. If the disease is not treated, the entire leg will suffer: it will become cold, bending and unbending it will be problematic, and then the ability to move the foot and toes will be lost.
Prevention of sciatica
In fact, avoiding the development of sciatica is much easier than then suffering from unbearable pain and undergoing treatment. To do this, as well as to avoid relapse of the disease after successful treatment, it is enough to lead a healthy lifestyle and follow simple rules:
- maintain the level of physical activity at an optimal level (daily walking, morning exercises and visits to the pool 2-3 times a week are enough to maintain normal muscle tone and improve the condition of the whole body);
- take breaks every hour when working sedentarily and use an orthopedic corset if you need to sit for a long time;
- purchase an orthopedic mattress that will not sag under body weight;
- observe the correct technique for lifting heavy objects: with your knees bent and your back straight;
- refuse strong physical activity;
- normalize your diet and avoid overeating.
Thus, it is possible to cope with sciatica, improve the quality of life and avoid the risk of losing the ability to self-care at almost any stage of development. But it is much easier to do this when the first symptoms appear. Otherwise, the likelihood of needing surgery is very high.
Pinching symptoms
Doctors consider several syndromes that indicate that the patient has a pinched nerve.
- Lesera – straight leg does not rise;
- Sikara – pain intensifies if a person bends the foot;
- landing - it is impossible to take a sitting position yourself.
It hurts to walk and squat, but if you lie down or sit with your legs spread wide apart, it goes away. Signs of inflammation and pinching of the sciatic nerve are quite expressive, but they can still be confused with other diseases:
- spondylitis;
- myeloma;
- ankylosing spondylitis;
- phlebothrombosis;
- arterial insufficiency.
Types of lumboischialgia
According to the method of progression, lumboischialgia is divided into 2 forms:
- acute – characterized by acute lumbago that occurs for the first time;
- chronic - pain (they are nagging and dull) appears periodically and systematically, periods of exacerbation are replaced by remission.
Depending on the affected area, lumbago with sciatica occurs:
- unilateral – pathology covers the right or left side of the body;
- bilateral, or bilateral - inflammation spreads to both sides.
Depending on the cause, lumbar sciatica is distinguished:
- vertibral, or vertebrogenic – caused by diseases of the spine:
- discogenic – develops with intervertebral hernia;
- spondylogenic – caused by osteochondrosis;
- nonvertebrogenic – not associated with diseases of the spine:
- angiopathic - provoked by disruptions in the blood circulation of the lower back and lower extremities;
- myofascial – a consequence of damage to muscles and fascia;
- caused by pathologies of the peritoneal organs;
- caused by problems in the hip joints;
- idiopathic - the cause cannot be determined.
How to make a diagnosis
The disease is determined by a neurologist based on the results of motor tests that reveal the presence of the syndromes described above. But laboratory and instrumental studies are still necessary. As a rule, they are limited to x-rays in two planes. It may be necessary to obtain a more clear picture of the condition of the spine. In this case, a tomography will be prescribed. A radioisotope scan is done if a tumor is suspected.
When a person has inflammation of the sciatic nerve, treatment at home is not always acceptable, because the disease can manifest itself in such a serious form that the patient is prescribed bed rest in a hospital setting. Nerve-related illnesses must be taken seriously or you may lose your ability to move.
An immediate visit to a doctor is necessary in the following cases:
- severe numbness that prevents you from moving;
- increased body temperature;
- transfer of pain to other locations;
- incontinence of metabolic products;
- swelling in the lower part of the ridge.
Causes
Compression of the sciatic nerve can occur in a variety of different cases. This can occur due to injuries to the legs, pelvis and back, during pregnancy, prolonged immobility, pinched nerves by fibrous cords or neoplasms, etc.
Most often, sciatica becomes a complication of various spinal diseases, including:
- lumbar osteochondrosis - degeneration of large intervertebral discs of the lumbar spine is the main prerequisite for the development of other spinal diseases and pinching of nerve fibers of different sizes;
- the formation of intervertebral hernias is the most common complication of osteochondrosis, manifested by protrusion of the disc, which leads to compression and damage to the spinal roots;
- spondylolisthesis – displacement of the vertebrae relative to the underlying one by different amounts, which can provoke pinching of the nerve roots;
- facet syndrome - nerve fibers are pinched in the narrow natural openings of the spine as a result of deformation of the vertebrae, the formation of osteophytes, or other disorders.
Another common cause of sciatica is spasm of the piriformis muscle located in the buttock. Since the sciatic nerve passes through it, an increase in its tone leads to stretching and irritation of the nerve fiber, which immediately results in severe pain.
Other prerequisites for the development of sciatica include:
- excessive physical activity;
- spinal tumors of various natures from hemangiomas to malignant neoplasms;
- arthritis;
- thrombosis of blood vessels;
- hypothermia and the development of inflammatory processes in anatomical structures adjacent to the spine at the level of the lumbosacral region;
- infectious gynecological and other diseases, including influenza, tuberculosis, typhoid fever, sepsis (released toxins affect the sheath of the sciatic nerve);
- spinal deformities (scoliosis, etc.).
How to treat inflammation of the sciatic nerve
Treatment measures are aimed at:
- relieving the patient of pain;
- improved sensitivity of the limbs;
- restoration of leg functionality.
To achieve this, they resort to methods of traditional and alternative medicine. Treatment begins with pain relief. Then physiotherapy, therapeutic exercises, and manual therapy come into play. In parallel, the rich experience of traditional medicine can be used.
Medicines prescribed for the treatment of sciatica include the following groups of drugs:
- non-steroidal;
- corticosteroids;
- vitamin complexes;
- biogenic stimulants;
- muscle relaxants;
- decongestants;
- angioprotectors.
External means are widely used - warming creams and ointments, which contain snake or bee venom, hot pepper, camphor, turpentine. Massage for inflammation of the sciatic nerve helps improve blood circulation and restore muscle tone.
A huge role in restoring leg functions belongs to physiotherapeutic procedures, for example, magnetic and laser therapy, electrophoresis, and dynamic current treatment. Various types of physical exercises, selected for a specific patient, reduce muscle spasms and strengthen the body.
To heal at home, you will have to be patient, since sciatica responds better to the efforts of professionals. There are cases when the disease started precisely because of insufficiently active therapeutic measures. The more complex the case, the more effective drugs have to be prescribed. So, if non-steroidal drugs do not help, although a person takes them for a long time, steroid drugs are prescribed, which have significant side effects.
In many clinics, in addition to the main treatment, patients undergo courses:
- acupuncture;
- ozone therapy;
- herbal medicine;
- cupping and vacuum massage;
- stone therapy;
- treatment with leeches;
- cauterizations.
Many recipes for compresses, lotions, and tinctures have been developed. But it is better not to try them on yourself without consulting your doctor. The doctor knows where and how they can help or harm. Therefore, it is necessary to consult.
Spa and hydrotherapy is an excellent way to improve overall health and regulate various pathologies, including inflammation of the sciatic nerve, the symptoms and treatment of which, due to their diversity and complexity, require long-term and careful attention.
If therapeutic methods do not produce results, the nerve has to be decompressed. This is done surgically.
It is not enough to know how to treat sciatica, that is, inflammation of the sciatic nerve. It is necessary to be aware of how to protect yourself from such a serious, life-spoiling and health-robbing illness.
Among the preventive measures, doctors recommend the following:
- do not freeze;
- strengthen immunity;
- lift weights correctly;
- develop posture;
- sleep on hard mattresses;
- beware of sudden movements.
A healthy body significantly increases the likelihood that the spine will work correctly, and the nerve roots will avoid inflammation and will not be pinched.
We specialize in the treatment of the musculoskeletal system, even in severe stages of disease. We have been helping thousands of patients avoid surgery for 10 years!
Our doctors
This is the strongest team of experts who teach at the RUDN Department. We are the clinical base of leading universities, where the best doctors in Moscow, unique specialists from Russia and abroad are trained.
Diagnostics
A neurologist diagnoses and treats sciatica. It is this specialist who should be contacted if any of the above symptoms occur. Already during the first appointment, based on the patient’s complaints and examination, the doctor may suspect compression of the sciatic nerve. But in order to find the most effective treatment, you need to find out why this happened. For this purpose, the patient is prescribed a set of studies, thanks to which the condition of the intervertebral discs, joints, bones, etc. can be assessed.
Therefore, as part of the diagnosis of sciatica and the causes of its occurrence, the following are used:
- X-ray of the sore leg, sacrum and lower back - the results of the study show the condition of the vertebrae and partly the intervertebral discs;
- MRI – provides comprehensive information about the condition of the intervertebral discs and spinal cord;
- CT is an informative method that allows you to detect pathologies of the sacrum and lumbar vertebrae;
- Electroneuromyography – provides data on the quality of transmission of nerve impulses to the muscles of the lower extremities and their contractility.
The most informative method for diagnosing diseases of the cartilage tissue from which intervertebral discs are formed, as well as pathologies of the spinal cord, is MRI. It is this method that allows you to thoroughly examine the discs, assess their size, position, and detect the slightest hernia and other disorders.