A cerebellar cyst is a dangerous neoplasm that can lead to disruption of brain activity and paralysis of the limbs. This type of benign tumor requires mandatory treatment. The characteristics of the compaction determine whether the doctor will prescribe drug therapy or surgical intervention.
It threatens with disruption of brain activity and paralysis of the limbs.
Features of the pathology
A thickening is a cavity that appears in different parts of the cerebellum. It is filled with liquid contents and gradually increases in size. This cyst provokes consequences, so it must be treated immediately after diagnosis.
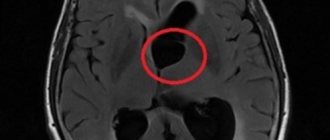
The pathology is located between the roof of the brain (blue arrow) and the pineal gland (red arrow).
The difficulty in prescribing therapy in a timely manner is that there are no symptoms, at least in the early stages of tumor development. As its size increases, signs appear, but by this time the capsule may already have grown significantly.
Causes
Cysts in the cerebellum can be congenital or acquired. Its causes depend on what type it belongs to. If the neoplasm is of the congenital type, it is formed during the period of embryonic development. This is due to developmental disorders during pregnancy or death of brain tissue. Necrosis may occur due to suffocation. This occurs during childbirth or in cases where the fetus, for certain reasons, lacks oxygen.
Risk factors that provoke the development of acquired pathology include:
Head injuries, concussions.
- acute foci of inflammation;
- hematoma in the brain area, which appeared due to mechanical impact;
- stroke;
- previous surgical interventions (related to the brain);
- concussions;
- injuries, blows, skull fractures;
- infections with parasites;
- multiple sclerosis.
Types of tumors of the cerebellopontine angle
Approximately every tenth brain tumor develops in the cerebellopontine angle. At the same time, the most common tumor localized in this area is neuroma of the vestibulocochlear nerve—it accounts for 85–95%. Meningiomas and cholesteatomas of the cerebellopontine angle are much less common.
In most cases, neuroma of the vestibulocochlear nerve is benign. Most often it develops in people of working age, usually women. Removal of tumors of the cerebellopontine ganglion can be either unilateral or bilateral.
Types of cysts
Doctors have developed classifications that relate to the location and etiology of the tumor. There are the following varieties:
- Cystic-glial changes usually appear against the background of previous injuries in the head area. A cyst of the right or left hemisphere of the cerebellum has pronounced symptoms. These include worsening migraines, constant loss of strength, and dizziness. Subsequently, convulsions appear;
- A retrocerebellar tumor occurs where necrosis of gray matter cells occurs. This is often associated with a stroke, surgery in the skull, or blows. If it appears between the hemispheres, it is triggered by problems with the blood supply to tissues, with infections and with a source of inflammation. It provokes a severe migraine, which painkillers cannot cope with, as well as significant changes in consciousness and even hallucinations;
Occurs in the place where cell necrosis occurs. - An arachnoid cyst appears in the cerebellar space. The appearance of the capsule is facilitated by scars on the tissue, which are associated with problems with the flow of cerebrospinal fluid. Signs appear depending on where the lump appears. An arachnoid cyst must be removed if it enlarges. When the capsule reaches a large size, it causes severe symptoms, such as seizures similar to epilepsy;
- the subarachnoid cavity is usually congenital. It is discovered after the baby is born during a standard examination. Less commonly, this type of neoplasm is acquired. Then the appearance is associated with infection with neuroinfections, with a stroke. Accompanied by pulsation in the brain tissue, convulsions;
- A pineal tumor appears in the pineal gland, which affects the production of hormones. An epiphysis cyst is characterized by loss of orientation in space and a constant desire to go to bed. The patient may experience double vision;
- pseudocyst is a congenital type of seal. They lack a lining of epithelial tissue.
Surgical treatment
Treatment of a tumor of the cerebellopontine angle is predominantly surgical. Surgery is performed after a complete neurological examination. Surgical treatment of the cerebellopontine angle includes surgical operations using modern endoscopic equipment. High-quality neuroimaging allows you to select the appropriate medical tactics and determine the approach for the best removal of the tumor.
The neurosurgeon primarily uses endotracheal anesthesia and modern inhalation anesthetics. The patient is in a sitting position. The removed tumor tissue can be subjected to additional studies in order to make a full prognosis for the future.
It is very important to contact a neurosurgeon at the first signs of the development of the disease. At the initial stage of tumor growth, microsurgical techniques are used to preserve the functionality of the nerve structures. In this case, specialists use translabyrinthine access to the tumor. If the size of the tumor does not exceed a few centimeters, it is possible to maintain full hearing for the patient. The severe stage of the disease requires the use of the posterior cranial fossa as a surgical approach.
The method of surgical treatment of a tumor is determined by the size of the tumor and its location. The neurosurgeon selects the appropriate tactics based on the results of a comprehensive diagnosis and assessment of the patient’s general condition.
Radiation therapy is used for subtotal removal of a tumor and is an auxiliary technique. But their effectiveness has not been proven to date. The only reasonable solution is to have surgery performed in a qualified medical facility. Most of such operations in the country are carried out at the Burdenko Research Institute. It has the necessary technical equipment for effective surgical treatment of brain tumors of various locations. Specialists use all available capabilities of modern neurosurgery to treat patients and prevent life-threatening complications.
Symptoms
It is quite difficult to determine the development of a cyst in the early stages. This happens because it does not manifest itself in any way and does not bother the person. Congenital tumors may not affect infants and sometimes resolve spontaneously.
If the acquired neoplasm increases in size or even provokes the appearance of adhesions, the following symptoms occur:
- there is a feeling of compression and pulsation in the area of the skull;
- Coordination gradually deteriorates, the patient experiences loss of orientation in space;
- tinnitus is accompanied by nausea. Possible partial hearing loss, bouts of vomiting;
- the pain in the head sometimes becomes very severe. Painkillers do not cope with it;
- the rhythm of sleep and wakefulness is disrupted, insomnia appears;
- in difficult situations, convulsions, trembling of hands and fingers occur;
- periodic fainting occurs;
- subsequently vision deteriorates, paralysis (partial or complete) cannot be ruled out;
- the person begins to limp and cannot relax the muscles that are cramped by tension or cramps.
If we talk about symptoms in newborns, we are talking about constant regurgitation and vomiting.
Clinical picture
Primary cysts most often do not manifest themselves in any way and do not interfere with a person’s life. As a rule, this pathology is not treated.
Symptoms of a secondary formation depend on its size and etiology. Small brain cysts do not have pathological symptoms; they are characteristic of large specimens. However, experts have identified several common signs of the disease:
- Severe pain in the head that is not relieved by painkillers.
- Dizziness, in some cases there is loss of consciousness.
- Bursting and pulsating sensations in the head area.
- Periodic nausea. Sometimes it ends in vomiting, which, in turn, does not bring relief.
- Disturbance of sleep and biological rhythms of patients.
- Cramps, tremor of fingers.
- Neurological symptoms.
- In children under one year of age, bulging and pulsation of the large fontanel and frequent regurgitation, in some cases vomiting, are observed.
- Coordination of movements worsens, gait changes.
- Partial or complete paresis and paralysis of the upper and lower extremities occur.
- Some areas of the skin may lose sensitivity.
- Pathological changes in hearing, vision, and speech are possible.
It is also necessary to note individual symptoms of cerebellar cysts depending on their type:
- hallucinations are characteristic of a retrocerebellar cyst;
- when the right half of the cerebellum is damaged, a person becomes quickly fatigued, both physical and mental;
- paralysis is more often observed with the development of pathology in the left half of the organ;
- hydrocephalus is a sign of cyst-like expansion of the subarachnoid space.
What is the danger?
Small seals do not pose a danger to human life and health. The problem is that in most cases they continue to grow and begin to put pressure on the brain tissue. This provokes the following complications:
Complete or partial paralysis cannot be ruled out.
- blood circulation deteriorates, insufficient oxygen reaches the cerebellum;
- irreversible processes occur that affect speech, vision, hearing, and coordination of movements;
- complete or partial paralysis cannot be ruled out, in which it is impossible to restore lost functions;
- in the most severe cases, the pathology leads to the death of the patient.
Sometimes spontaneous rupture of the capsule membranes occurs, which leads to sepsis and a purulent inflammatory process in the cerebrospinal fluid. There is also a risk of internal bleeding, paralysis and death.
A cerebellar cyst in a newborn child (if it does not resolve) causes developmental disorders and delays in many functions.
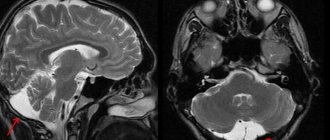
Arachnoid cysts
Arachnoid cysts (AC) are congenital, predominantly extracerebral formations, the walls of which are the arachnoid membrane, and the contents are cerebrospinal fluid (CSF). In children, arachnoid cysts, according to various sources, account for about 10% of all volumetric formations of the brain and in 7.4% of cases are found in children with hydrocephalus. The division of arachnoid cysts into two large groups is pathogenetically justified: 1. Cysts of the cerebral hemispheres: - lateral (Sylvian) fissure; - convexital surface of the brain; - parasagittal interhemispheric fissures).
2. Mid-basal cysts: - suprasellar; - intrasellar; - tentorial notch; — posterior cranial fossa (upper and lower retrocerebellar, cysts of the cerebellopontine angle).
The group of mid-basal cysts can also include mid-stem cysts (retrocerebellar), since they are identical in their pathogenetic mechanisms.
The most common locations of arachnoid cysts are the Sylvian fissure (lateral fissure), interhemispheric fissure and suprasellar cistern. However, they can occur anywhere where the arachnoid membrane is located. Morphologically, the inner and outer walls of the cyst consist of thin layers of arachnoid cells and are often connected to the unchanged arachnoid membrane. Cysts can be congenital (primary) or acquired (secondary). Unless there is a history of trauma or inflammation, the cysts are considered congenital. Currently, there are several theories about the occurrence of arachnoid cysts. The first is the “intraarachnoid cyst theory,” in which cyst formation is the result of splitting and duplication of the arachnoid membrane. The second is the “subarachnoid cyst theory,” which explains the occurrence of middle cranial fossa cysts as a result of agenesis of the temporal lobe. The formation of arachnoid cysts occurs at the stages of embryogenesis during the formation of the membranes of the brain. Under pathological conditions, mainly with subarachnoid hemorrhage caused by hypoxia, infection, intoxication, etc., it becomes possible to form microcavities in the arachnoid membrane, which subsequently increase in size, turning into arachnoid cysts.
Most arachnoid cysts remain undiagnosed during life. The patient’s condition can remain compensated for a very long time, and the course of the disease is asymptomatic. The first manifestations can be noticed in adulthood. The timing of referral of children with congenital arachnoid cysts to neurosurgical departments, as a rule, depends on the location and size of the cysts. It is known that cysts of the tentorial notch cause more severe neurological symptoms. Common symptoms, which, however, manifest themselves to varying degrees in cysts of different localizations, include: - volumetric effect on the surrounding structures of the brain; — presence of an asymptomatic period; - no signs of inflammation in the membranes of the brain.
Positive meningeal symptoms are usually observed only when the disease is complicated by subarachnoid or intracystic hemorrhage. Hyperthermia and inflammatory changes in the blood are not typical for arachnoid cysts. — the severity of compensatory mechanisms and the absence of gross neurological manifestations in the presence of significant morphological changes, which is especially typical for hemispheric cysts. The clinical picture of arachnoid cysts is determined in most cases by three symptom complexes: hypertensive-hydrocephalic, focal neurological symptoms and damage to the brain stem. Signs of damage to the brainstem only in cysts of the cerebral hemispheres should be regarded as dislocation; in cysts of mid-basal localization, they can also be caused by the direct effect of the cyst on the brainstem. The uniqueness of the clinical picture of cysts in individual locations is determined by the duration of the asymptomatic period, the severity and characteristic coloring of the three leading neurological syndromes. It is believed that children with intracranial arachnoid cysts that have a mass effect should be operated on, because the volumetric effect of the cyst can lead to a delay in the development and formation of the brain, and rupture of the cyst is usually accompanied by intracystic and subdural bleeding. These complications justify the risk of surgical intervention. A direct indication for surgical treatment is progressive hydrocephalus that occurs when a cyst blocks the cerebrospinal fluid circulation pathways.
Currently, effective methods of surgical treatment of arachnoid cysts, including in the Department of Neurosurgery of the Russian Children's Clinical Hospital, are: perforation of the walls of the cyst with excision of its walls using the microsurgical method (through a small trefination window), as well as the neuroendoscopic method. CSF shunt operations are used extremely rarely.
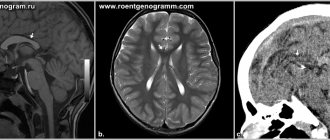
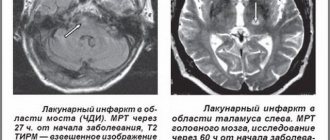
Diagnostics
During a visit, during which the patient complains of unpleasant symptoms, the doctor prescribes diagnostic measures to clarify the diagnosis. MRI is considered the most revealing examination method. Magnetic resonance imaging demonstrates where the tumor is located and clarifies its size and structure. During the examination, you can find out how the tumor affected the surrounding tissues, whether deformation of the worm and other parts has occurred.
In addition to MRI, the following procedures are prescribed:
- puncture. Provides analysis of cerebrospinal fluid in order to exclude or confirm an inflammatory process in tissues;
- the contents can be sent for histological examination in order to clarify the nature of the compaction. If cancer cells are present, the treatment will be radically different than for a benign type of cyst;
- An electroencephalogram is designed to calculate convulsive contractions of the brain. The results of this manipulation also influence the prescribed treatment;
- if the patient is a small child who has not yet turned 2 years old, neurosonography is prescribed. This is a safe type of research that gives a complete picture of the processes occurring in the cerebellum;
- A blood test is necessary in order to exclude concomitant infectious diseases or foci of inflammation.
Treatment
This type of neoplasm requires a special approach. Doctors seek to remove most thickenings in order to improve the person’s condition. But brain intervention always carries serious risks, so it is prescribed only in the most severe cases.
Therefore, most often they try to limit the growth of the cyst and reduce the unpleasant symptoms experienced by the patient. Drug treatment is prescribed in most cases.
Drug therapy
After completing diagnostic measures, the doctor chooses treatment tactics. It is aimed at preventing the growth of the cyst. In addition, it contributes to the achievement of the following goals:
- resorption of adhesions that appear due to the progression of pathology;
- ensuring proper functioning of the circulatory system;
- saturation of brain cells with oxygen and necessary components;
- lowering cholesterol;
- normalization of blood pressure levels;
- maintaining blood clotting;
- combating pathogens of dangerous infections (if they are present);
- maintaining a high level of immunity;
- antioxidants should increase cell resistance to increased pressure.
The attending physician decides how long the rehabilitation will last. The patient should not independently discontinue medications or change the established daily dosage.
Surgery
Doctors put off surgical intervention until last. It is prescribed when medications do not cope with their tasks. The operation is associated with a high risk of damage to brain structures, so it is prescribed in specific cases:
Microneurosurgery is used.
- coordination of movements is increasingly impaired;
- cancer cells have been identified;
- the patient suffers from severe cramps;
- the tumor is constantly increasing in size;
- there is a possibility of cerebral hemorrhage.
The intervention is carried out using one of three main methods. Microneurosurgery is used, which requires opening the skull. The accuracy of capsule removal is guaranteed, but the risk of damage to healthy tissue is also higher.
The endoscopic method minimizes the risk of complications and also shortens the recovery period. The third type of operation is bypass surgery. With it, a catheter is inserted into the cavity, through which the contents of the capsule are pumped out. However, it cannot be kept for a long time, otherwise there is a possibility of penetration of pathogenic pathogens.
Features of surgery to remove a tumor of the cerebellopontine angle
Removal of the tumor of the cerebellopontine angle is carried out surgically. Before surgery, patients of this profile undergo general clinical and neurootological examination, CT and MRI. According to indications, myo- and angiography and neuropsychological testing are prescribed.
Removal of a tumor of the cerebellopontine angle is performed using modern methods of endoscopic microsurgery under conditions of constant neurophysiological monitoring (including stimulation and EMG of the facial nerve). After neuroimaging, the doctor develops a surgical plan, determines its volume and the point of best access. The intervention is carried out using high-speed drills and pneumatic drills, which ensure minimal invasiveness and reduce the extent of damage to nearby tissues.
Removal of a tumor of the cerebellopontine angle is carried out under endotracheal anesthesia in a closed circuit using Propofol and inhalational anesthetics (Sevoflurane, Isoflurane). Necessary conditions for the operation, which is performed in a sitting position, are also Doppler ultrasound of the heart and a special surgical table with supports for the surgeon’s hands. During the removal of a tumor of the cerebellopontine angle, it is possible to perform a rapid analysis of the removed fragment of the tumor with subsequent correction of the course of the operation.
The final result of surgical intervention is determined by the characteristics of tumor growth, the degree of damage to the base of the skull, and its fusion with neurovascular structures. In most cases, I, together with a team of assistants at the N. N. Burdenko Research Institute of Neurosurgery, manage to solve all the problems facing us.
Folk remedies
Traditional recipes help curb tumor growth. However, they should not be used thoughtlessly. Before using any product, you must obtain the approval of your physician. Otherwise, you may not improve the condition, but only provoke the development of complications.
Traditional recipes can be used during the recovery period, but not in the acute stage. They are used only in combination with medications prescribed by a doctor. To slow down the growth of a tumor, the following means are used:
- spotted hemlock. It is used alone or in combination with elderberry and violet;
- tea from viburnum, rowan or horsetail helps stabilize blood pressure, which has a positive effect on the patient’s condition;
Viburnum tea stabilizes blood pressure levels. - fresh vegetables (celery, asparagus, etc.) help strengthen the immune system and give strength to fight pathology.
Prevention
If we talk about the prevention of congenital neoplasms, then a pregnant woman should lead a correct lifestyle. You need to give up bad habits and avoid emotional stress. It's important to eat right. If the body does not receive enough nutrients with food, it is necessary to additionally consume vitamin complexes designed for pregnant women.
Secondary tumors can also be prevented. To do this, follow the general recommendations:
Monitor your blood pressure readings.
- diseases associated with the nervous system require prompt treatment. Their nature does not matter - infectious, vascular, etc.;
- undergoing a routine examination by a doctor. If you experience any disturbing symptoms, even minor ones, consult your doctor immediately;
- don't let yourself freeze. It's about the head - always wear a hat;
- monitor your blood pressure and take medications if it changes;
- watch your cholesterol;
- minimize the likelihood of developing infectious diseases, avoid contact with sick people;
- get rid of bad habits.
Neoplasms in the cerebellum usually require immediate treatment. In newborns, they can resolve spontaneously. But adults need to take medications under the supervision of a physician. In the most severe cases, surgical intervention is prescribed.
Preventive actions
Any unpleasant symptoms should not be ignored. Therefore, if the patient exhibits the above symptoms, it is necessary to seek advice from specialists (neurologist or neurosurgeon).
If a person is diagnosed with a cerebellar cyst, it is important to follow several recommendations that will help avoid complications:
- You need to visit your doctor periodically. This is necessary to monitor the patient’s condition and monitor the formation over time.
- Undergo diagnostic tests prescribed by a specialist.
- Carry out prevention against infectious diseases. You should increase the body's defenses: take vitamins, provide adequate nutrition, and healthy sleep.
- Prevent hypothermia of the body. A person should dress according to the season, avoid drafts, and keep his feet warm.
- Give up bad habits (drinking alcohol, smoking).
- It is necessary to monitor blood counts. If cholesterol or platelet levels increase, you should take medications prescribed by the doctor (prevention of blood clots, ischemia of brain tissue, and so on).
- Monitor blood pressure levels. If hypertension is observed, then constant medication is needed. This will help avoid strong pressure surges.
- If your health worsens, it is important to inform your doctor about it in order to adjust your treatment.