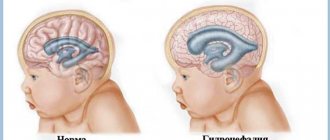
Hydrocephalus is an excessive accumulation of cerebrospinal fluid in the cranial cavity, which results in an increase in the size of the subarachnoid spaces, basal cisterns, and ventricles of the brain. All conditions have been created for the treatment of patients with hydrocephalus at the Yusupov Hospital. The neurology clinic employs candidates and doctors of medical sciences, doctors of the highest category. Neurologists have the knowledge and experience to quickly diagnose the disease and provide adequate therapy.
Causes of hydrocephalus
Hydrocephalus develops due to the accumulation of cerebrospinal fluid in the cerebrospinal fluid system of the brain in the event of the production of an excess amount of cerebrospinal fluid, impaired absorption or disturbance of the circulation of cerebrospinal fluid. In case of exposure to damaging factors on the fetal brain during intrauterine development, congenital hydrocephalus occurs. Acquired hydrocephalus develops under the influence of various pathological mechanisms after the birth of a child.
The following causes of congenital hydrocephalus are known:
- intrauterine infections (hydrocephalus, toxoplasmosis, cytomegaly, syphilis);
- birth injury;
- defects in the development of the cerebrospinal fluid system (atresia of the foramina of Magendie and Luschka, stenosis of the Sylvian aqueduct, structural defects of the subarachnoid space, Dandy-Walker syndrome);
- developmental anomalies of the skull and spine (congenital basilar impression, Chiari malformation).
Acquired hydrocephalus occurs as a result of inflammatory processes of the brain and its membranes, traumatic brain injuries, acute and chronic vascular disorders. Hydrocephalus in adults often develops against the background of a colloid cyst of the third ventricle and intracerebral tumors (germinomas, astrocytomas, ganglioneuromas) growing into the ventricles of the brain or compressing the cerebrospinal fluid tract, disrupting the normal circulation of cerebrospinal fluid and its outflow from the cranial cavity.
Make an appointment
What types of external hydrocephalus of the brain are there?
External hydrocephalus of the brain refers to the accumulation of cerebrospinal fluid (cerebrospinal or cerebrospinal fluid) outside the cerebral hemispheres - in the subarachnoid space. Due to the large accumulation of fluid, the subarachnoid fissures widen, which causes increased pressure on the cerebral cortex and the resulting negative consequences.
The nature and level of complexity of the disease directly depend on the specific type of dropsy. Several criteria are used for classification. The most common ones are:
- intensity of manifestation (pronounced - accumulation of a large amount of cerebrospinal fluid, causing neurological symptoms; moderate - minimal amount of fluid, no signs);
- degree of impact on brain structures (compensated - cerebrospinal fluid does not affect the brain; decompensated - there is a deterioration in the functioning of the nervous system and brain);
- causes of occurrence (replacement - more often diagnosed in older people and is accompanied by the death of brain cells; acquired - occurs due to the spread of infections and mechanical traumatic brain injuries);
- nature of the course (chronic form - a gradual increase in neurological disorders; acute form - a sharp deterioration in the patient’s well-being).
Employees of the Department of Neurosurgery of the City Clinical Hospital named after. Eramishantsev will first determine the type of external hydrocephalus and only then begin treatment. Particular attention is paid to diagnostic data and a thorough study of the symptoms of the identified disease.
Types of hydrocephalus in adults
There are open (communicating), closed (occlusive) and replacement hydrocephalus. Open hydrocephalus of the brain in adults involves free communication of spaces through which cerebrospinal fluid circulates. It develops when there is an imbalance in production and reabsorption of cerebrospinal fluid. There are hyperproductive, aresorptive and mixed forms of hydrocephalus.
Replacement hydrocephalus can be a consequence of physiological aging of the body or develop in pathological conditions of the central nervous system, accompanied by atrophic changes (Alzheimer's disease, Creutzfeldt-Jakob disease). This form of the disease does not refer to true hydrocephalus, caused by impaired cerebrospinal fluid dynamics, but occurs as a result of the filling of “free” spaces inside the skull with cerebrospinal fluid.
In accordance with the location of the expanded cerebrospinal fluid spaces in relation to the brain tissue, the following types of hydrocephalus in adults are distinguished: internal (intraventricular), external (subarachnoid) and mixed. Depending on the level of intracranial hydrocephalus, hypertensive and normotensive hydrocephalus are distinguished. In functional and clinical aspects, progressive (increasing), stabilized (not changing over time) and regressive (decreasing) hydrocephalus are distinguished. Progressive hydrocephalus can be decompensated or subcompensated.
In acute hydrocephalus, no more than three days pass from the moment of the first symptoms of the disease to severe decompensation. Subacute progressive hydrocephalus develops within one month from the onset of the disease, and chronic hydrocephalus develops within a period of 3 weeks to 6 months.
Hydrocephalus in adults
Department of Emergency Neurosurgery > Diseases
This section is intended for people suffering from hydrocephalus, as well as for their relatives and friends. We hope that the information provided will help you better understand the disease and how to overcome it. Here we will talk about the causes of hydrocephalus in adults, methods for diagnosing it in the early stages, provide a list of necessary studies, reflect modern techniques used in our institute for the diagnosis and treatment of hydrocephalus, as well as prospects for the development of this field of neurosurgery.
Most people, including doctors, classify hydrocephalus as a childhood disease. Indeed, from 1 to 10 children out of every thousand newborns suffer from hydrocele. During a specialized examination of patients over 18 years of age in neurosurgical hospitals, hydrocephalic syndrome is detected in every fourth patient. Due to the lack of clear criteria for diagnosing hydrocephalus, only single operations for the disease in question are performed annually in non-core neurosurgical departments. Patients are discharged from such hospitals with diagnoses: “psycho-organic syndrome”, “dyscirculatory or post-traumatic encephalopathy”, “dementia of mixed origin”, “consequences of traumatic brain injury”, consequences of stroke.” This is not a complete list of diseases, under the guise of which patients are unsuccessfully treated in clinics, neurological hospitals and psychiatric hospitals. Timely and correct diagnosis of hydrocephalus and adequate surgical treatment allow patients to achieve recovery, work and social rehabilitation in almost 100% of cases. Thus, most of our patients return to their previous work, and some of the sick, despite incomplete work adaptation, can live without outside help, perform simpler activities, becoming full-fledged members of society.
A special group of patients in our department are patients with acute forms of hydrocephalus
, mainly with intraventricular hemorrhages and hemotamponade of the ventricles of the brain due to
non-traumatic subarachnoid hemorrhages
.
In cases where there is no specialized surgical care for such patients, they die within the first 12 to 48 hours from the onset of the disease. Modern methods of external drainage
with the introduction of thrombolytics into the ventricles of the brain, used in our department, can not only reduce mortality in this pathology, but also stabilize the condition of patients for a long time.
Below we present the basic concepts and terms necessary to understand the problem of hydrocephalus in adults and how to control it.
Functional anatomy of the cerebrospinal fluid-containing spaces of the brain and the definition of hydrocephalus.
Normally, each person's central nervous system contains about 120-150 ml of cerebrospinal fluid (CSF, cerebrospinal fluid). The physiological significance of CSF is as follows:
- is a kind of shock absorber for the brain, thus providing its mechanical protection during shocks and shocks
- performs nutritional functions
- maintains osmotic and oncotic balance at the tissue level
- has protective (bactericidal) properties, accumulating antibodies
- takes part in the mechanisms of regulation of blood circulation in the confined space of the cranial cavity and spinal canal.
CSF is formed in the cells of the choroid plexuses of the ventricles of the brain.
The largest amount of CSF is produced by the plexuses of the lateral ventricles of the brain (Fig. 1). The volume of CSF in the cranial cavity and in the spinal canal in an adult does not exceed 125–150 ml. About 500-600 ml of CSF is produced per day and the same amount is continuously absorbed. From the lateral ventricles of the brain, which contains about 25 ml of CSF, which enters the third ventricle through the foramen of Monroe, and from there, through the cerebral aqueduct (Aqueduct of Sylvius), the fluid enters the cavity of the fourth ventricle. The third and fourth ventricles of the brain contain approximately 5 ml of CSF. From the fourth ventricle, through the median foramen of Magendie and two lateral foramina of Luschka, located in the area of the lateral inversions of the fourth ventricle, CSF enters the subarachnoid space of the brain. At the base of the brain, the subarachnoid space expands and forms cavities filled with CSF (basal cisterns). The largest of them is located between the cerebellum and the medulla oblongata - the large cistern of the brain (cerebellar-medullary cistern). From it, CSF enters the premedullary and lateral cerebellar-medullary cisterns, located on the lower and lateral surfaces of the medulla oblongata, respectively. On the lower surface of the pons of the brain there is a rather large prepontine (prepontine) tank, which receives CSF from the above tanks. The prepontine cistern is separated from the midbrain and diencephalon cisterns (covering, interpeduncular, peduncular, chiasmatic, optic nerve) by a sheet of semipermeable membrane (Liliekvist membrane), which promotes one-way flow of CSF in the direction from back to front and from bottom to top. From the cisterns of the brain, CSF enters the convexital part of the subarachnoid space, washing the cerebral hemispheres, then is absorbed into the venous bed through the arachnoid cells and villi. The accumulation of such villi around the venous sinuses of the dura mater of the brain (there are especially many of them in the superior sagittal sinus) is called pachyon granulations. Liquid is partially absorbed into the lymphatic system, which occurs at the level of the nerve sheaths. The movement of CSF in different directions is also associated with vascular pulsation, breathing, and muscle contractions. (Fig. 1-2). If there is a violation of the relationship between the production and absorption of CSF at any of the listed levels (increased production of CSF by the choroid plexuses; closure of the ventricular openings by a tumor, adhesions, blood clots; obstruction of cells, villi and pachyonic granulations by erythrocytes, fibrosis of the membranes after hemorrhage or previous meningitis; occlusion of the sinuses) leads to a significant (maximum up to 12 liters in congenital hydrocephalus) accumulation of CSF, forming the development of hydrocephalus. The term “hydrocephalus” itself is formed by the merger of two Greek words “hydro” - water and “cephalus” - head (“dropsy of the brain”).
Below is the most complete definition of the concept of “adult hydrocephalus”.
Hydrocephalus in adults is an independent nosological form, or a complication of a number of brain diseases (tumor, hemorrhage, trauma, stroke, infectious process, etc.), characterized by an active progressive process of excessive accumulation of CSF in the cerebrospinal fluid spaces, caused by disturbances in its circulation (proximal and distal forms of occlusive hydrocephalus), absorption (aresorptive and dysresorptive forms), or production (hypersecretory form) and manifested morphologically by enlargement of the ventricles of the brain, periventricular leukareosis (decrease in the density of the medulla due to its saturation with CSF) and narrowing of the subarachnoid spaces. Clinical manifestations of hydrocephalus depend on its form.
Diseases that contribute to the formation of hydrocephalus in adults.
It has now been established that almost any pathology of the central nervous system can lead to such a complication as hydrocephalus.
Below we provide a list of only the main diseases in which hydrocephalus most often occurs:
- Brain tumors (usually stem, para-stem, or intraventricular localization).
- Inflammatory and infectious diseases of the central nervous system (meningitis, ventriculitis, encephalitis, tuberculosis, etc.).
- Subarachnoid and intraventricular hemorrhages (traumatic and non-traumatic), most often due to rupture of aneurysms and arteriovenous malformations of cerebral vessels.
- Acute cerebrovascular accidents of ischemic and hemorrhagic type.
- Encephalopathies of various origins (alcoholism, chronic hypoxic conditions, etc.).
In the department of emergency neurosurgery of the Research Institute of Emergency Medicine named after.
N.V. Sklifosovsky's priorities are the problems of diagnosis and treatment of acute and chronic hydrocephalus in non-traumatic subarachnoid hemorrhages due to rupture of arterial aneurysms of cerebral vessels or arteriovenous malformations, as well as post-traumatic hydrocephalus. Classification and pathogenesis of hydrocephalus.
- Based on its origin, hydrocephalus is divided into congenital and acquired.
Congenital hydrocephalus, as a rule, debuts in childhood. The causes of its occurrence are various intrauterine infections, hypoxia and, mainly, congenital developmental anomalies, leading either to disruption of the CSF circulation (stenosis and occlusion of the Sylvian aqueduct, Dandy-Walker anomaly, Arnold-Chiari anomaly, etc.), or accompanied by underdevelopment of structures, involved in CSF resorption (aresorptive hydrocephalus).Acquired hydrocephalus is further classified depending on the etiological factor (see causes of hydrocephalus).
- According to pathogenesis, there are three main forms of hydrocephalus.
- Occlusive (closed, non-communicating) hydrocephalus, in which the flow of cerebrospinal fluid is disrupted due to closure (occlusion) of the cerebrospinal fluid pathways by a tumor, a blood clot, or a post-inflammatory adhesive process. In the event that occlusion occurs at the level of the ventricular system (foramen of Monro, aqueduct of Sylvius, foramina of Magendie and Luschka), we are talking about proximal occlusive hydrocephalus. If the block in the path of the CSF flow is at the level of the basal cisterns, then they speak of a distal form of occlusive hydrocephalus.
- Communicating (open, dysresorptive) hydrocephalus, in which the processes of CSF resorption are disrupted due to damage to the structures involved in the absorption of CSF into the venous bed (arachnoid villi, cells, Pachionian granulations, venous sinuses).
- Hypersecretory hydrocephalus, which develops due to excess production of CSF (choroid plexus papilloma).
Previously, a fourth form of hydrocephalus was also identified, the so-called external (mixed, ex vacuo) hydrocephalus, which was characterized by an enlargement of the cerebral ventricles and subarachnoid space in conditions of progressive brain atrophy. However, this process should still be attributed to brain atrophy, and not to hydrocephalus, because the enlargement of the ventricles of the brain and the expansion of the subarachnoid space are not caused by excessive accumulation of CSF, due to disruption of the processes of its production, circulation and resorption, but by a decrease in the mass of brain tissue against the background of atrophy. - Based on current rates, they are distinguished:
- Acute hydrocephalus, when no more than 3 days pass from the first symptoms of the disease to severe decompensation.
- Subacute progressive hydrocephalus, developing within a month from the onset of the disease.
- Chronic hydrocephalus, which develops over a period of 3 weeks to 6 months or more.
- Based on the level of cerebrospinal fluid pressure, hydrocephalus is divided into the following groups:
- Hypertensive
- Normotensive
- Hypotensive
Clinical picture and diagnosis of hydrocephalus in adults.
With occlusive hydrocephalus, especially acutely developing, symptoms of increased intracranial pressure come first, which include:
- Headache;
- Nausea and/or vomiting;
- Drowsiness;
- Stagnation of the optic discs;
- Symptoms of axial dislocation of the brain.
Headache is most pronounced in the morning upon awakening, which is associated with an additional increase in intracranial pressure during sleep.
This is facilitated by vasodilation due to the accumulation of carbon dioxide, which is accompanied by blood flow, stretching of the walls of blood vessels and the dura mater of the brain at the base of the skull. Nausea and vomiting also worsen in the morning and sometimes lead to a decrease in headaches. Drowsiness is the most dangerous sign of increased intracranial pressure; its appearance precedes a period of sharp and rapid deterioration of neurological symptoms.
The development of stagnation of the optic discs is caused by an increase in pressure in the subarachnoid space surrounding the nerve and a disruption of the axoplasmic flow in it.
With the development of dislocation syndrome, there is a rapid depression of the patient's consciousness to a deep coma, oculomotor disorders appear (due to the expansion of the cerebral aqueduct), and sometimes a forced position of the head. Compression of the medulla oblongata manifests itself in rapid depression of breathing and cardiovascular activity, leading to the death of the patient.
The clinical picture is fundamentally different in the formation of chronic hydrocephalus
. The main manifestation of chronic dysresorptive hydrocephalus is a triad of symptoms:
- dementia;
- apraxia of walking or lower paraparesis;
- urinary incontinence.
The first symptoms of the disease usually appear 3 weeks after hemorrhage, trauma, meningitis or another disease leading to the development of hydrocephalus.
Disturbances in the sleep-wake cycle come first: patients become drowsy during the day with disturbances in night sleep. Subsequently, the general level of activity of the patients sharply decreases, they become spontaneous, lacking initiative, and inert. Among memory disorders, short-term memory disorders, especially numerical memory, come first. Thus, a patient with hydrocephalus cannot name the date, month, year, and incorrectly indicates his age. In the later stages of the disease, severe mnestic-intellectual impairments develop; patients can no longer care for themselves; they answer questions asked in monosyllables with long pauses, often inadequately. Apraxia of walking is that a patient with hydrocephalus can freely pretend to walk in a lying position or ride a bicycle, but as soon as he takes a vertical position, this ability is instantly lost, the patient walks with his legs wide apart, unsteadily, his gait becomes shuffling. In the later stages stages of the disease, lower paraparesis develops.
Urinary incontinence is the most late and variable symptom.
Stagnation of the optic discs is atypical for chronic hydrocephalus; as a rule, there are no changes in the fundus of the eye in such patients.
Diagnosis of hydrocephalus.
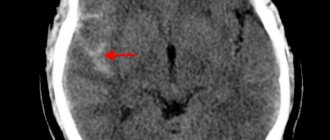
Computed tomography and magnetic resonance imaging play a leading role in the diagnosis of hydrocephalus (Fig. 1).
Rice. 1. Chronic dysresorptive hydrocephalus on CT: symmetrical expansion of the ventricular system with balloon-like enlargement of the anterior horns (one arrow), lack of visualization of subarachnoid fissures, foci of periventricular leukareosis (two arrows).
In the department of emergency neurosurgery of the Research Institute of Emergency Medicine named after. N.V. Sklifosovsky organized round-the-clock operation of the computed tomography department. We perform a CT scan on incoming patients with subarachnoid hemorrhage in the first hours after hospitalization to assess the nature and extent of the hemorrhage, then we conduct a CT scan as a control after surgery, or when the first signs of hydrocephalus appear.
To assess the stage of hydrocephalus and determine indications for surgical intervention, our department calculates ventriculo-cranial coefficients, which show the degree of expansion of the ventricular system and its decrease after the operation.
Computed tomography also makes it possible to clarify the presence and extent of concomitant ischemic brain damage in patients with subarachnoid hemorrhages.
To predict the outcome of surgical treatment of hydrocephalus, all patients undergo a tap-test
. The essence of the test is that when at least 40 ml of cerebrospinal fluid is removed during lumbar puncture, patients with chronic hydrocephalus experience a short-term improvement. In the case of a positive test, the patient's recovery after surgery can be more likely to be predicted. However, a negative result often does not indicate the impossibility of a good outcome in the late postoperative period.
Treatment of hydrocephalus.
Conservative treatment of hydrocephalus in adults with a full-blown clinical picture is ineffective.
- Treatment of acute hydrocephalus.
- Treatment of chronic hydrocephalus.
Acute hydrocephalus, which often occurs with intraventricular hemorrhages with the development of ventricular hemotamponade, is a serious complication requiring immediate neurosurgical intervention, the purpose of which is to “unload” the ventricular system, ensure normal cerebrospinal fluid flow, and reduce intracranial pressure
and
express sanitation of cerebrospinal fluid
.
In our department, similar operations are performed, which involve the application of external ventricular drains followed by the introduction of streptokinase into the ventricular cavity - a drug that dissolves blood clots and thereby ensures normal cerebrospinal fluid flow.
In addition, the department carries out direct measurement of intracranial pressure
such patients in order to select optimal infusion therapy and adequately monitor the dynamics of the patient’s condition.
The goal of the operation is to create an artificial pathway to drain excess CSF to an area where fluid can be easily absorbed. To achieve this goal, special liquor shunt systems are used.
Shunt system design. Each CSF shunt system consists of three components:
- Ventricular catheter - intended for installation in the lateral ventricles of the brain.
- A valve is a device that allows you to regulate the outflow of CSF. The valve is designed for certain values of cerebrospinal fluid pressure and when a certain pressure is reached, the valve opens and CSF begins to flow out of the ventricular system. When the pressure normalizes, the valve closes and the flow of cerebrospinal fluid from the ventricles stops.
- Peripheral catheter - designed for installation in various cavities of the body that have the ability to absorb fluid (abdominal cavity, pelvic cavity, atrium, etc.) (Fig. 2).
a) b)
Rice. 2. Scheme of the ventriculoperitoneal shunt operation: a) cranial stage; after puncture and drainage of the anterior horn of the right lateral ventricle from Kocher's point (one arrow), the ventricular catheter is passed into the postauricular region, where it is connected to the valve of the shunt system at the level of the projection of the foramen of Monroe (two arrows); b) peritoneal stage; additional incisions in the supraclavicular region and at the level of the xiphoid process are marked with an arrow.
Every year, our department performs about 50 surgeries for hydrocephalus in adults.
We use the most advanced technologies in the installation of cerebrospinal fluid shunt systems: we use programmable valves
that allow non-invasive regulation of CSF pressure;
we install valve systems with a built-in anti-siphon device
that prevents the reverse flow of cerebrospinal fluid when the body position changes;
To implant a catheter into the abdominal cavity, endovideolaparoscopic equipment
, which allows to minimize the trauma of the operation and achieve the best results (Fig. 3).
a) b)
Rice.
3. Outcome of shunt surgery for chronic dysresorptive hydrocephalus. a) CT scan after non-traumatic subarachnoid hemorrhage. Severe internal hydrocephalus is determined (VKK2-26%). b) CT scan after implantation of a ventriculoperitoneal shunt. The normalization of the dimensions of the ventricular system is determined with the regression of foci of periventricular leukareosis and the appearance of visualization of subarachnoid fissures. Timely and correctly performed surgical intervention for hydrocephalus allows in almost 100% of cases to achieve recovery of patients, their labor and social rehabilitation.
Symptoms of hydrocephalus in an adult
The accumulation of an excess amount of cerebrospinal fluid in a limited space of the cranium leads to an increase in intracranial pressure, which causes the most typical signs of hydrocephalus: intense headache that cannot be relieved by analgesics, nausea and vomiting, a feeling of pressure on the eyeballs.
These symptoms of hydrocephalus in an adult patient can occur acutely or increase gradually, having a transient nature at the onset of the disease. Replacement hydrocephalus often occurs without signs of increased intracranial pressure. Neurologists at the Yusupov Hospital detect it only after additional examination of the patient. Hydrocephalus of the brain in an adult in the photo has characteristic signs: an increase in the volume of the head and frontal bone.
In most cases, hydrocephalus in adults is accompanied by neurological symptoms. It is caused both by compression of brain structures by expanded cerebrospinal fluid spaces and by the underlying disease, which is the cause of the development of hydrocephalus. With hydrocephalus, vestibular disorders are observed: gait instability, dizziness, noise in the ears and head, nystagmus. Visual function is impaired: there is a significant decrease in visual acuity and loss of certain areas of the visual field. During ophthalmoscopy, ophthalmologists identify congested optic discs. With prolonged hydrocephalus, atrophy of the optic nerves develops.
Hydrocephalus in adults can occur with disturbances in the motor and sensory spheres:
- paresis and paralysis;
- decrease or complete loss of all types of sensitivity;
- increased tendon reflexes and muscle tone;
- formation of spastic contractures of the limbs.
Occlusive hydrocephalus, caused by impaired circulation of cerebrospinal fluid in the posterior cranial fossa, is characterized by symptoms of cerebellar ataxia: changes in handwriting, large-scale disproportionate movements, impaired gait and coordination.
Patients suffering from hydrocephalus develop mental disorders over time, manifested by disorders of the emotional-volitional sphere: neurasthenia, emotional instability, causeless euphoria with a rapid transition to a state of apathy. With a sharp increase in liquor pressure, patients begin to behave aggressively.
Diagnosis of hydrocephalus
Neurologists at the Yusupov Hospital conduct a comprehensive examination of patients with hydrocephalus. Computed tomography currently occupies a dominant position among methods for diagnosing hydrocephalus. The procedure is carried out to determine the size and shape of the ventricles, identify developmental anomalies and neoplasms, cysts.
Magnetic resonance imaging allows you to determine the shape and severity of hydrocephalus. Using this diagnostic method, the cause of cerebral hydrocele is determined. Neurosonography helps assess the degree of expansion of the ventricles of the brain. The procedure is used only when diagnosing the disease in children with an open fontanelle, since the skull blocks ultrasound. Neurosonography is used to diagnose hydrocephalus in utero.
Cisternography is a research method in which a radioactive substance is injected into the cerebrospinal fluid. It is used to clarify the type of hydrocephalus and determine the direction of cerebrospinal fluid flow. During an angiography, a contrast agent is injected into the arteries that supply blood to the brain. After some time, anomalies at the level of blood vessels and pathological processes are detected. Doctors at the Yusupov Hospital use innovative methods for diagnosing cerebral vascular diseases - magnetic resonance angiography, which does not require the administration of contrast agents. A neuropsychological examination involves conducting a survey to identify abnormalities in the functioning of the brain.
results
Of all patients with cortical dysplasia (71 people), 27 had abnormalities of cell proliferation, 18 had abnormalities of migration, 25 had abnormalities of cortical organization, and 1 patient had a mixed anomaly. Histological confirmation was obtained in 20 patients (28%) of 71.
The complex “expansion of the subarachnoid space - deepening into the cortex” occurred in 29 patients (41%), including 5 people (19%) out of 27 with a proliferation anomaly, 2 patients (11%) out of 18 with a migration anomaly, and 22 patients (88%) out of 25 had an anomaly of cortical organization (Fig. 2). Of the 25 patients with an anomaly of cortical organization, the “expansion of the subarachnoid space - deepening into the cortex” complex was identified in all 9 patients with polymicrogyria (Fig. 3), in all 4 patients with schizencephaly (Fig. 4) and in 9 (75%) of 12 patients with features associated with focal cortical changes. In 3 out of 4 patients with schizencephaly, the brain had an “open-labial” configuration.
Visualization of the complex does not have any value in identifying abnormalities of proliferation, migration, or mixed abnormalities. For example, in cases of hemimegalencephaly with the complex “expansion of the subarachnoid space - deepening into the cortex,” the identification of this complex is not decisive in the diagnosis of this anomaly, such as, for example, hemihypertrophy, thickening of the cortex, hyperdensity.
However, the identification of this complex helped in establishing a diagnosis in 12 (48%) patients out of 25 with a disorder of cortical organization (Fig. 5). In these patients, recognition of the complex “expansion of the subarachnoid space - deepening into the cortex” helped establish the diagnosis of dysplasia (Fig. 6, 7) or correctly classify cortical dysplasia (Fig. 4). Identification of the complex “expansion of the subarachnoid space - deepening into the cortex” was especially helpful in interpreting MRI data in 7 (58%) of 12 patients with mild focal thickening of the cortex or focal morphological changes in the cortex. The identification of the complex “expansion of the subarachnoid space - deepening into the cortex” prompted researchers to study the state of the cerebral cortex in more detail, which, in turn, led to the identification of cortical malformation (Fig. 6, 7). In 2 patients with polymicrogyria, the complex “expansion of the subarachnoid space - deepening into the cortex” was one of the leading MRI signs. The complex was a mandatory feature for the diagnosis of schizencephaly in 3 patients, since, by definition, the presence of expansion of the subarachnoid space distinguishes this anomaly from other developmental anomalies.
Treatment of hydrocephalus
Neurologists at the Yusupov Hospital take a differentiated approach to treating patients with hydrocephalus. In case of a regressed form of the disease, drug therapy is not used. To reduce cerebrospinal fluid pressure, patients are prescribed diuretics: Diacarb, mannitol, Lasix. Nootropics, venotonics and angioprotectors improve the functional activity of the brain.
For progressive hydrocephalus, neurosurgeons at partner clinics of the Yusupov Hospital perform shunt operations. If there is an obstacle to the outflow of cerebrospinal fluid, the space-occupying lesion is removed or the adhesions are cut. If a hematoma is present, it is removed surgically.
An innovative method of treating hydrocephalus is endoscopic surgery:
- endoscopic ventriculocisternostomy of the bottom of the third ventricle;
- endoscopic installation of a shunt system;
- septostomy;
- aqueductoplasty;
- ventriculocystocysternostomy;
- endoscopic removal of intraventricular brain tumor.
Endoscopic operations have a number of advantages compared to bypass interventions: they restore the physiological flow of cerebrospinal fluid, are less traumatic, and improve the patient’s quality of life.
Treatment with endoscopic methods
Endoscopic treatment of hydrocephalus, or dropsy of the brain, is a priority in neurosurgery, since this disease is common among both children and adults. Hydrocephalus of the brain occurs due to impaired absorption of cerebrospinal fluid into the venous system.
Endoscopic surgery
Endoscopic interventions for hydrocephalus of the brain are used to reduce intracranial pressure. Surgeries for dropsy are most effective in comparison with drug therapies, which help slow the progression of the disease, but do not eliminate it. Endoscopic surgery for hydrocephalus, the cost of treatment of which is determined by the severity of the disease, is divided into several types:
- Septostomy;
- Ventriculocisternostomy of the floor of the third ventricle;
- Ventriculocisternostomy;
- Installation of the shunt system endoscopically;
- Removal of intraventricular tumors endoscopically;
- Aqueductoplasty.
The most widely used is endoscopic ventriculocisternostomy of the bottom of the third ventricle. The main task of the surgeon with this technique is to create pathways for the outflow of cerebrospinal fluid from the ventricles into the cisterns of the brain, through which the cerebrospinal fluid is absorbed into the vascular walls, as in a healthy person.
Advantages of endoscopic operations
Endoscopic surgery can only be effective if it is performed by a good specialist. One wrong move by the surgeon during brain surgery can lead to irreparable, severe consequences. When shunts are installed, they are often blocked by blood clots, tumor cells, etc. During endoscopy, no foreign objects remain in the body, and accordingly, the development of such complications is excluded.
In severe cases, patients are given brain drains. Such an event is very dangerous, since the infection can easily penetrate the brain through the drainage. With endoscopic intervention this complication does not occur.
Bypass surgery
Many people who have been diagnosed with the disease wonder where to treat hydrocephalus: in a public medical institution or a modern clinic. Yusupov Hospital is equipped with the latest equipment. Doctors regularly improve their skills and master new treatment methods. The clinic staff ensures a comfortable stay for patients.
Shunt surgery for hydrocephalus in adults, the price of which varies depending on the characteristics of the disease, is performed safely and efficiently at the Yusupov Hospital. Installation of a shunt system ensures the removal of cerebrospinal fluid. The procedure lasts about 90 minutes and is performed under general anesthesia for patients of any age.
Bypass surgery is a safe intervention, but there are certain risks when using it, which the neurologist informs the patient about. For example, a reaction to anesthesia or bleeding may develop. Shunt surgery allows the patient to restore normal brain function.